How to determine gangrene?
The symptoms of gangrene are reflected depending on the type of necrosis. Gangrene symptoms of the digestive system manifest themselves in the form of peritonitis. A person may experience signs of food poisoning and severe pain.
In a general sense, there are 2 main types - dry and wet gangrene . Separately, gas gangrene is distinguished.
signs of gangrene
Signs of necrosis
Symptoms of intestinal gangrene develop approximately 6 hours after an attack of acute ischemia. The patient's condition is extremely serious. The following pathological manifestations are noted:
- sudden severe weakness;
- pale skin;
- unbearable abdominal pain;
- flatulence;
- vomit;
- diarrhea or delayed bowel movements;
- rapid heartbeat;
- weak pulse;
- a sharp drop in blood pressure;
- loss of consciousness.
Signs of pathology also depend on the location of the area of necrosis. Gangrene of the small intestine is characterized by vomiting of bile and blood. As necrosis develops, fecal admixture appears in the vomit. When the colon is affected, bloody diarrhea occurs.
12-14 hours after the cessation of blood supply, peritonitis begins. The patient's pain disappears, as the nerve endings become necrotic. Gases and feces do not pass away. The patient is inhibited and apathetic. In severe cases, seizures occur and the patient falls into a coma. This condition can be fatal within 48 hours.
Gangrene: causes and symptoms
Dry gangrene spreads to the skin, fingers and toes. In case of impaired blood circulation and stagnation in the arteries, the tissues will receive the necessary nutrition. Symptoms of dry gangrene:
- The damaged part of the body is always colder than the healthy part.
- Over time, a person may lose sensitivity.
The patient's general condition remains stable, since there is no poisoning of the body. with this type of gangrene , but no one excludes the possibility of transformation into the wet form. If you contact a specialist in a timely manner, normal blood circulation can be restored and the need for amputation can be avoided. The main cause of the disease is the gradual occurrence of stagnation in the blood vessels.
Wet gangrene is very dangerous. Both types of gangrene have similar symptoms: cold extremities, lightening of the skin, lack of pulse. The beginning of the development of gangrene of the foot:
- A body part cannot move fully. The foot has indicators of cadaveric decomposition.
- General health is poor: the patient gets tired quickly and is weakened.
- To all of the above is added temperature, anemia, and decreased blood pressure.
Darkening of a certain part of the body, the appearance of an unpleasant odor. When you press on the affected area, you can hear a specific sound due to the accumulation of hydrogen sulfide.
diagnosis of gangrene
The most important thing is timely recognition of the symptoms of gas gangrene. In theory, it is similarly a wet gangrene, which is caused by certain bacteria and toxic substances.
An indicator that is specific to gas gangrene is poisoning and a rapid deterioration of the general condition, as the sending substances spread throughout the body, causing intoxication. The main reason for such infection is the penetration of microorganisms into wounds.
Causes
Impaired blood supply to tissues is now one of the most common causes of gangrene. In this case, the tissues do not receive enough oxygen and necessary nutrients, which leads to changes in their structure, and subsequently necrosis. The pathological condition can occur with the development of various peripheral arteries, as well as against the background of:
- Diabetes mellitus.
- Atherosclerosis.
- Oncological diseases.
- Diseases of the endocrine system.
Another common cause of gangrene is the activation of pathogenic microorganisms, most often bacteria. Against this background, tissue destruction and death occurs. As a rule, processes occur when the immune system is weakened and various infectious diseases develop. In particular, gas gangrene is caused by the anaerobic pathogen Clostridium.
Factors that provoke tissue necrosis include physical and chemical influences that lead to tissue damage. The pathological condition often occurs due to thermal, radiation or chemical injury.
Which symptoms should be given more importance?
The first signs of gangrene are severe pain, which can be eliminated exclusively with the help of analgesics. In addition, a change in skin color is considered a primary indicator. It is possible to establish the presence of gangrene in the internal organs due to the deterioration of the general condition.
The negative side will be the presence of diabetes mellitus, so patients with such pathology are advised to be more attentive and not turn a blind eye to the first signs. Damage to blood vessels, burns, radiation sickness play a negative role in the spread of gangrene of the arms , legs, and the like.
Stages of ischemia
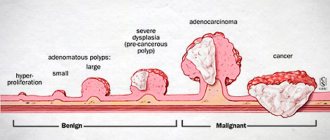
Necrosis of intestinal tissue develops in several stages. Doctors distinguish several stages of ischemia:
- Impaired blood supply. Due to a lack of nutrients in the intestinal tissues, metabolism deteriorates. Dystrophic changes occur in the epithelium. Because of this, the production of enzymes decreases and food digestion is disrupted, and peristalsis also changes. At this stage, the oxygen deficiency is compensated by the flow of blood through bypass routes.
- Intestinal infarction. This stage of ischemia is considered decompensated. Blood stops flowing even through the bypass branches of the vessels. Tissue necrosis occurs. At this stage, intestinal gangrene occurs. Photos of necrotic areas of the epithelium can be seen below.
It should be noted that with decompensated ischemia, the color of the intestinal wall changes. First, due to lack of blood supply, anemia occurs and the epithelium of the organ turns pale. Then the blood begins to leak through the vessels. The intestinal wall becomes red. Blood appears in the stool. In this case, doctors talk about hemorrhagic gangrene of the intestine, since tissue necrosis is accompanied by bleeding. As necrosis develops, the affected area becomes black.
Without surgery, necrosis very quickly leads to peritonitis. Tissue death is aggravated by inflammation. The wall of the organ becomes thin and ruptures. The contents of the intestines come out, and inflammation of the peritoneum occurs. This often causes death.
How to properly treat gangrene?
The first thing you need to know is that self-medication can lead to dire consequences, so you should abandon this idea. No need to waste time, make an appointment with a doctor immediately.
An exceptionally experienced specialist will be knowledgeable about how gangrene on the arm can be cured, etc., and will therefore be able to prescribe treatment for you without the need for amputation.
gangrene treatment
To avoid negative consequences, it is necessary to restore normal blood circulation, so doctors prescribe minimally invasive endovascular operations on arteries and vessels to patients with gangrene on the arms and legs. In addition, specialists can resort to necrectomy, which will ensure that there is no need for amputation.
Wet gangrene - symptoms and treatment
If wet gangrene is not treated or it is too late to see a doctor, then within the first year 20% of patients die, 25% of patients undergo amputation, and only 55% of patients have a chance to save a limb or organ. These indicators reflect the full drama of the situation: the threat to the health and life of patients is very high [8].
Amputation, as the only possible way to save the patient’s life, is indicated when complex treatment is ineffective, the wound is enlarged, surgery is impossible, the patient’s condition worsens, and late treatment to the doctor results in gangrene developing.
Mortality after limb amputation reaches 18-20% [9]. This is due to the patient’s advanced age, the presence of many concomitant diseases and the prevalence of the lesion: many tissues of the limb are involved in the process, the infection is septic in nature. In such cases, toxins and decay products of dead tissue poison the entire body. Despite this, amputation is the only option to save the patient’s life.
To avoid complications associated with amputation, the operation should be performed in two stages:
- primary amputation - removal of dead tissue, an attempt to restore blood flow and save the limb;
- secondary amputation - is carried out when measures to save the limb are ineffective and there is no positive dynamics: the wound after the primary amputation does not heal [9][14].
In the presence of a purulent-necrotic lesion and the risk of blood poisoning, its primary sanitation should be performed before surgery [10].
Other treatment-related complications are possible with critical limb ischemia. It is dangerous to perform surgical treatment of the wound in this case: it can expand the area of necrosis. Before this, revascularization of the limb, such as stenting, is required.
During revascularization, complications may develop in the form of nephropathy—impaired kidney function. Patients with generalized atherosclerosis, renal artery calcification, and stage II or higher chronic kidney disease are especially at risk [8][15][16]. To prevent nephropathy, before and after surgery, patients at risk should discontinue metformin, loop diuretics and administer 1 liter of saline solution dropwise intravenously.
Prevention of wet gangrene consists of regular examination, monitoring of existing diseases and early consultation with a doctor at the first symptoms of thrombosis or ischemia of the limb. Even a seemingly small wound can lead to the loss of a limb.
If there is a hereditary predisposition to varicose veins, it is necessary to perform an ultrasound scan of the veins of the lower extremities every year and consult a phlebologist. For preventive purposes, your doctor may prescribe wearing compression garments: this will help avoid the formation of blood clots and the progression of chronic venous diseases.
In case of diabetes mellitus, it is important to adjust the level of glucose in the blood, perform an annual ultrasound of the abdominal organs, arteries and veins of the lower extremities, and also properly care for the skin of the legs:
- apply nourishing and softening creams;
- treat dry calluses and nail plates;
- wear orthopedic shoes.
Diagnostics
In case of gangrene, the patient requires immediate surgery and there is very little time left for diagnosis. When palpating the abdomen, a swollen area of the intestine with the mesentery is determined. This is a specific manifestation of necrosis.
Upon admission to the hospital, the patient is given an X-ray of the intestine. No contrast agent is administered. If the image shows signs of tissue destruction or peritonitis, then surgical intervention is started immediately.
Treatment
Surgery is the only treatment for intestinal tissue necrosis. Dead parts of the organ have to be removed. First, the surgeon restores the blood supply and then resects the affected area. After this, sanitation of the abdominal cavity is performed.
After the operation, the patient is prescribed a course of antibiotics and anticoagulants. Special solutions are administered to dissolve blood clots. Novocaine blockades are given to prevent intestinal spasms. It is also necessary to administer medications to maintain heart function.
Drug therapy is only an additional method of treatment and is used after surgery. It is impossible to get rid of such a disease using conservative methods alone.
Disability
The most pronounced consequences are observed in patients after surgery for gangrene of the small intestine. Is there a disability group or not? This question often interests patients.
During surgery, part of the intestine is removed. As a result, the length of the organ changes and its function changes. Patients experience periodic abdominal pain, flatulence, diarrhea, and weight loss. The condition after surgery is called short bowel syndrome (SBS). The purpose of the disability group depends on the degree of its severity:
- 3rd group. It is prescribed if the manifestations of SCM are moderate or moderate, and body weight is no more than 5-10 kg below normal.
- 2nd group. It is established if the patient has a severe form of SBS. At the same time, in addition to diarrhea, there are signs of vitamin deficiency and metabolic disorders, and the person loses more than 10 kg of weight.
- 1 group. It is prescribed to the most severely ill patients in whom SBS occurs with complications and has intestinal fistulas. This disability group is also assigned to those patients from whom 4/5 of the small intestine has been removed.
Diagnostic methods
Diagnosis of the disease, both acute and chronic forms, presents certain difficulties. An integrated approach is required, including examination of the patient, laboratory and instrumental studies.
Laboratory research
They help to assess the general condition of the patient and exclude some pathology (oncological process with decay). The most informative:
- general clinical blood test (leukocytosis without anemia, shift of the formula to the left with late presentation);
- disturbance of acid-base balance (acidosis);
- clotting factors;
- biochemical tests to exclude pancreatitis (amylase and blood sugar).
Only the entire complex of laboratory reactions can be correctly assessed, and not just one result.
Instrumental studies
The most informative angiographic study is an online assessment of the intestinal blood supply using a contrast agent. It is this method that allows you to accurately determine the location of the blood clot (embolus). With early angiography (the first 1-2 hours from the onset of clinical symptoms), it is possible to remove this obstacle without removing intestinal tissue.
Symptoms
The clinical symptoms of the disease are nonspecific and are similar to many other conditions included in the concept of “acute abdomen”. Establishing a correct diagnosis involves excluding such conditions; for a lay person this is an impossible task.
Acute form
- abdominal pain (in the upper parts or without a specific localization) of a spastic nature;
- increasing bloating and constant release of gases;
- diarrhea, sometimes mixed with blood;
- nausea and repeated vomiting without significant relief.
During the examination, the doctor draws attention to the absence of specific symptoms of peritoneal irritation against the background of a pronounced pain syndrome.
Chronic form
- cramping pain in the upper abdomen, which occurs a long time after eating (30-50 minutes);
- weight loss due to increasing necrosis and deterioration of nutrient absorption;
- alternating diarrhea and constipation.
If you suspect intestinal gangrene, you should consult a doctor as soon as possible, since early diagnosis is the key to a successful outcome of the disease. Self-medication and self-diagnosis will cause irreparable harm to the patient.
Forecast
The outcome of the disease largely depends on how timely medical care was provided for intestinal gangrene. The prognosis of this pathology is always very serious.
Even with timely surgery, death occurs in more than 50% of patients. Without surgical intervention, mortality is 100%. Patients die from sepsis or peritonitis.
The sooner a patient is hospitalized and operated on, the greater the chance of survival. If assistance was provided on the first day of illness, the prognosis is more favorable.