Abdominal pain, heartburn or belching are symptoms familiar to every person. Dyspeptic symptoms occur when the gastrointestinal tract function is disrupted. Due to the prevalence of diseases of the digestive tract, many people know that to eliminate unpleasant symptoms it is necessary to take antacids. Such drugs neutralize the aggressive effects of hydrochloric acid, thereby eliminating dyspepsia. The most effective and common antacids are Maalox or Almagel. The drugs have a quick effect and help cope with the symptoms of ulcers, duodenitis, pancreatitis or gastritis. To understand which product is better, you need to compare them.
Comparison of drugs
Both drugs represent a group of antacids and a group of drugs based on a combination of simple salts. Maalox was developed by a French pharmaceutical company, and Almagel by a Bulgarian one.
Maalox differs from Almagel in the list of indications. The instructions for the first drug indicate that it is used to eliminate heartburn, and in the Almagel instructions the list of indications includes stomach and duodenal ulcers, gastritis, gastroduodenitis and other gastrointestinal pathologies.
The differences between the drugs are also in the form of release: Almagel is available only in the form of an oral gel, and Maalox is available in the form of an oral suspension and chewable tablets. This form may be more suitable if you have difficulty swallowing.
Comparison of ease of use of Maalox and Almagel
This includes dose selection taking into account various conditions and frequency of doses. At the same time, it is important not to forget about the release form of the drug; it is also important to take it into account when making an assessment.
The ease of use of Maalox is approximately the same as Almagel. However, they are not convenient enough to use.
The drug ratings were compiled by experienced pharmacists who studied international research. The report is generated automatically.
Last update date: 2020-12-04 13:48:14
Difference between medications
When choosing which is better: Maalox or Almagel, you should compare their composition. The active ingredients in Almagel - alhydrate and magnesium hydroxide - are contained in a ratio of three to one, and in Maalox the same substances are contained in a ratio of one to one.
This difference is important because algedrate can reduce intestinal motility, and magnesium hydroxide can increase it.
Based on this, Maalox has no effect on the level of intestinal motility, and Almagel can cause constipation and intestinal obstruction. This side effect is especially observed with long-term use, as well as in the elderly and those prone to constipation.
According to reviews, the taste of Almagel is somewhat sweeter than that of Maalox. Comparing the price of drugs is complicated by the fact that they are available in different dosage forms and volumes. An approximate comparison of the same number of drugs shows only a slight difference in cost.
General characteristics
Comparison of medicines should be carried out not only by their composition and cost, but also by their effect on the body, which is manifested in the presence of certain adverse reactions, contraindications and indications. Only a gastroenterologist can take them into account individually for each case.
Comparison of the effectiveness of Maalox and Almagel
The effectiveness of Maalox is quite similar to Almagel - this means that the ability of the drug substance to provide the maximum possible effect is similar.
For example, if the therapeutic effect of Maalox is more pronounced, then using Almagel even in large doses will not achieve this effect.
Also, the speed of therapy - an indicator of the speed of therapeutic action - is approximately the same for Maalox and Almagel. And bioavailability, that is, the amount of a drug reaching its site of action in the body, is similar. The higher the bioavailability, the less it will be lost during absorption and use by the body.
Almagel
Suspensions based on algedrate and magnesium hydroxide paste in a ratio of 3:1, respectively. Sold in 10 ml sachets or 170 ml bottles with a dosing spoon. The effect of the drug develops quite quickly - within fifteen minutes after use.
Indications
It is used for esophagitis, hiatal hernia, gastroesophageal reflux disease, acute and chronic gastritis. Indicated for gastroduodenitis, peptic ulcer of the intestines and stomach, as well as post-resection gastritis. For pancreatitis, it is used to improve the effectiveness of enzymatic preparations.
As a prophylactic agent, it is used simultaneously during treatment with corticosteroids, non-steroidal painkillers and other drugs that have a detrimental effect on the gastric mucosa.
Contraindications
The use of Almagel is prohibited for:
- constipation;
- Alzheimer's disease;
- severe pain without an identified cause;
- acute appendicitis;
- ulcerative colitis;
- chronic diarrhea, hemorrhoids;
- renal failure;
- lactation;
- hypophosphatemia.
Before use, consult a doctor who will take into account possible contraindications and, if necessary, adjust the dosage.
Side effects
When treated with Almagel, the following undesirable reactions may develop:
- change in color of stool, nausea, constipation, stomach cramps;
- renal dysfunction;
- allergic reactions - local and systemic;
- osteomalacia and osteoporosis;
- change in taste sensations.
If adverse reactions are detected, you should contact your doctor, who will change the dosage or discontinue the drug.
General characteristics
Almagel and Maalox are gastroprotectors. They are presented in the form of tablets and suspensions. Contains aluminum hydroxide and magnesium hydroxide. Thanks to the action of the drugs, the negative effects of hydrochloric acid are reduced.
How they affect the body
Almagel helps to get rid of the irritating effect that occurs when hydrochloric acid enters the gastric mucosa and reduce overall acidity. As a result, the occurrence of heartburn, ulcers and other pathologies of the digestive organs is prevented.
The medicine has an enveloping effect, therefore reducing the likelihood of increased gas formation.
Maalox helps fight diseases of the esophagus - reflux esophagitis and effectively removes toxins from the body.
The drugs have the same effect on the body:
- stabilize the functions of the digestive organs;
- improve digestion;
- exhibit enveloping properties;
- regulate stomach acidity;
- do not allow dyspeptic symptoms to develop.
Almagel should not be taken if you have kidney failure.
Difference between medications
Medicines differ in composition. Almagel contains hyaetellose and lemon oil, and Maalox contains hydrochloric acid and peppermint oil. They differ in the concentration of the main component - Almagel contains more aluminum hydroxide. This remedy is prohibited for renal failure, and Maalox is prohibited for liver disease. The first drug is produced in France, the second in Bulgaria.
Which is better - Almagel or Maalox
When choosing a medication, the doctor takes into account the type of disease and contraindications. Experts recommend Almagel if gastritis has worsened and acidity has increased, as well as for flatulence. Maalox is best used for constipation and frequent bowel movements.
Maalox
Suspension and tablets based on magnesium hydroxide paste and algedrate in equal proportions. Maalox is sold in 15 ml sachets, 250 ml bottles and in tablet form with 20 and 40 tablets per package. Efficiency develops within the same time frame as that of Almagel.
Indications for use
It is used to treat heartburn, as well as acid regurgitation in children over 15 years of age and adults.
Contraindications
Treatment with Maalox is prohibited in case of severe renal failure, hypersensitivity to magnesium and aluminum compounds. Other contraindications are similar to those for Almagel.
Adverse reactions
With a diet poor in microelements, osteomalacia and osteoporosis, a decrease in phosphate in the body and hypercalciuria may develop during treatment.
Possible disturbances in the functioning of the gastrointestinal tract, angioedema, skin rashes, itching, urticaria. Excessive concentrations of magnesium and aluminum may be found in the blood.
Before starting to use Maalox, you should contact a gastroenterologist, who will prescribe a suitable dosage regimen and take into account the drug’s compatibility with other medications or existing contraindications.
Comparison of addiction in Maalox and Almageli
Like safety, addiction also involves many factors that must be considered when evaluating a drug.
So, the totality of the values of such parameters as “syndrome o” in Maalox is quite similar to the similar values in Almageli. Withdrawal syndrome is a pathological condition that occurs after the cessation of intake of addictive or dependent substances into the body. And resistance is understood as initial immunity to a drug; in this it differs from addiction, when immunity to a drug develops over a certain period of time. The presence of resistance can only be stated if an attempt has been made to increase the dose of the drug to the maximum possible. At the same time, in Maalox the meaning of the “syndrome” is quite small, however, the same as in Almageli.
What to choose between Maalox and Almagel?
The choice of Almagel or Maalox depends on the presence of contraindications, as well as the purpose of treatment. Almagel is often recommended for exacerbation of gastritis with high acidity of gastric juice. Maalox can be used for both acute and chronic forms.
If you have a tendency to constipation and stool disorders, it is better to choose Maalox, since when treated with it, the likelihood of constipation and obstruction is less. Otherwise, both drugs are identical; their price comparison is also inappropriate.
If there is renal dysfunction or a disorder of bone metabolism with the threat of osteomalacia and osteoporosis, it is strictly prohibited to take medications on your own without first consulting and receiving an individually selected treatment regimen.
Comparison of safety of Maalox and Almagel
The safety of a drug includes many factors.
At the same time, in Maalox it is quite similar to Almagel. It is important where the drug is metabolized: drugs are excreted from the body either unchanged or in the form of products of their biochemical transformations. Metabolism occurs spontaneously, but most often involves major organs such as the liver, kidneys, lungs, skin, brain and others. When assessing the metabolism of Maalox, as well as Almagel, we look at which organ is the metabolizing organ and how critical the effect on it is.
The risk-benefit ratio is when the prescription of a drug is undesirable, but justified under certain conditions and circumstances, with the obligatory observance of caution in use. At the same time, Maalox does not have any risks when used, just like Almagel.
Also, when calculating safety, it is taken into account whether only allergic reactions occur or possible dysfunction of the main organs. In other matters, as well as the reversibility of the consequences of using Maalox and Almagel.
Patient reviews
“After a starvation diet, my stomach upset and I developed serious gastritis. I tried Almagel, but for some reason it made my esophagus burn, the doctor prescribed Maalox in tablets. They dissolve slowly and the esophagus did not hurt.”
Olga, Nizhnekamsk
“You can rarely find Maalox anywhere here, which is strange. I take Almagel more often; after taking painkillers, I developed an ulcer. I can’t complain about the medicine, it works well, what about constipation is true. You can’t get carried away.”
Natalia, Pyatigorsk
special instructions
Almagel is not recommended for patients with diarrhea, ileostomy, colostomy, diverticulosis, ulcerative colitis, constipation, liver cirrhosis, acute hemorrhoids. The medicine does not contain sugar, so it is approved for diabetes. Maalox often provokes constipation, and as a result of an overdose, intestinal motility is weakened.
Pregnancy and lactation
Almagel is not recommended to be taken during pregnancy and lactation, but if necessary, it is taken under the supervision of a doctor and for no longer than 6 days. Maalox is prohibited for pregnant women, but can be used during breastfeeding.
Childhood
Almagel is prohibited for up to 10 years, Maalox for up to 15 years.
Elderly age
Taking Maalox in high dosages by older people causes obstruction and intestinal obstruction. Almagel is safe for older people.
Doctor's recommendations
“Both Maalox and Almagel are worthy representatives of antacids. Colleagues usually prescribe one that has already been tested in the treatment of certain pathologies and has shown itself to work well. I often prescribe Almagel to young patients, and Maalox to older patients, since this group of patients is more at risk of adverse reactions. Otherwise, I think it is inappropriate to compare such similar medications - the decision must be made after studying the anamnesis in detail.”
Vergun I.N., gastroenterologist-hepatologist, Moscow
Reviews
Svetlana, 35 years old, Moscow: “I was on a diet for a long time, which led to the development of gastritis. At first the doctor prescribed Almagel, but after 2 days an unpleasant burning sensation appeared in the stomach. Then the doctor recommended Maalox. This remedy worked well, the pain went away in 1 day.”
Dmitry, 48 years old, St. Petersburg: “I have high stomach acidity, which I have been suffering from for several years. In the last 2 months, severe heartburn and other unpleasant symptoms began to plague me. The doctor prescribed Almagel. I took it 1 scoop 2 times a day. After a week, the pain went away and the stool returned to normal. There were no adverse reactions.”
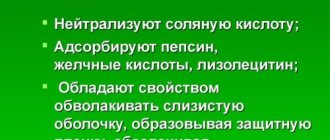
Efficacy of Maalox in long-term therapy of gastroesophageal reflux disease
In accordance with the national definition, approved by the VII Congress of the Scientific Society of Gastroenterologists of Russia, heartburn is a burning sensation behind the sternum and/or “in the pit of the stomach”, spreading from bottom to top, individually occurring in a sitting, standing, lying position or when bending the body forward, sometimes accompanied by a sensation acid and/or bitterness in the throat and mouth, often associated with a feeling of fullness in the epigastrium, occurring on an empty stomach or after consuming any type of solid or liquid food, alcoholic or non-alcoholic beverages, or the act of smoking [2]. The leading pathogenetic mechanism of the disease is pathological gastroesophageal reflux (GER). It occurs due to insufficiency of the obturator mechanism of the cardia (primarily failure of the lower esophageal sphincter and hiatal hernia), and the result of its effect on the mucous membrane of the esophagus is determined by the composition (hydrochloric acid, pepsin, bile acids, lysolecithin, pancreatic enzymes, etc.). ), duration of exposure (adequacy of esophageal clearance) and intrinsic mucosal resistance. An increase in intra-abdominal (for example, obesity, pregnancy, constipation) or intragastric pressure (functional or organic nature of gastric or duodenal stasis) contributes to the occurrence of GER. A systematic review of the results of 15 epidemiological studies conducted using a uniform method using the Mayo Clinic questionnaire [3] showed that the prevalence of GERD (the presence of heartburn and/or regurgitation once a week or more during the last 12 months) in Western Europe and Northern Europe America is 10–20%, and in Asian countries 5% [4]. Comparable data are demonstrated by epidemiological studies conducted in recent years in Russia. Thus, according to a study conducted by the Central Research Institute of Gastroenterology in 2003 in Moscow, the prevalence of GERD is 23.6% [5,6]. When performing an endoscopic examination, signs of reflux esophagitis are detected in less than 50% of patients with symptoms of GERD. It is noted that it is impossible to accurately predict the endoscopic picture of the disease, focusing on its clinical manifestations in a particular patient. That is, in the majority of patients, the disease manifests itself with symptoms associated with GER, which are disturbing, worsen well-being, and quality of life, but are not accompanied by changes in the esophagus that can be verified by esophagoscopy (complications of GERD). The morphological substrate of the disease is also present in such patients, but is of an ultrastructural nature and can only be detected by microscopic examination. It has been shown that in most patients, regardless of whether they receive treatment or not, the disease is not prone to progression [1]. The main goals of GERD therapy are relief of symptoms, improvement of well-being (quality of life), treatment and prevention of complications, primarily reflux esophagitis. Theoretically, based on the pathogenesis of the disease, the main directions of such therapy are reducing the volume and modifying the composition of the refluxant, increasing the anti-reflux function of the lower esophageal sphincter, reducing the pressure gradient directed from the stomach to the esophagus, increasing clearance (cleaning) of the esophagus, protecting the esophageal mucosa from damaging effects refluxant. Two strategies for drug treatment of patients with GERD are considered as alternative. The first of them, “step-up treatment,” involves changes in lifestyle and diet, as well as the use of antacid medications, at the initial stage of treatment. If this regimen was ineffective, a transition was sequentially made to the second (histamine H2 receptor blockers and/or prokinetics) and third stages (proton pump inhibitors (PPIs), a combination of PPIs and prokinetics). The second strategy is “step-down treatment”, in which initial treatment is carried out with a PPI and only after achieving a clinical and endoscopic effect, patients are gradually transferred to maintenance doses of PPI, therapy on demand, including taking antacids to relieve symptoms [7,8]. Recommendations for using a “step-down” strategy are based on the results of meta-analyses of works devoted to the comparative assessment of the effectiveness of the use of gastric secretion blockers, which showed that the healing rate of erosions of the esophageal mucosa within 12 weeks of treatment when using PPIs exceeds 80%, and when using H2 receptor blockers, histamine does not reach 50% [9]. In turn, these data explain Bell’s rule, according to which esophageal erosions heal in 80–90% of cases when the esophageal pH level is maintained above 4 for at least 16–22 hours a day [10]. This level of suppression of gastric acid production is achieved only with the use of PPIs, and therefore they are recognized as the most effective drugs in the treatment of GERD [11]. Thus, the “step-down” therapy strategy has a significant advantage in the form of the disease complicated by reflux esophagitis, since it not only quickly relieves the symptoms of the disease, but also significantly reduces the healing time of erosions of the esophageal mucosa. Without discussing the safety of long-term PPI therapy, we believe that not all patients with an uncomplicated (endoscopically negative) form of GERD need long-term and pronounced suppression of gastric acid production, in fact, only for the purpose of relieving symptoms associated with reflux. Probably, in a significant proportion of such patients, “gradually increasing” therapy is relevant and can be quite effective, and already at its first step, which involves changing lifestyle and taking antacids to relieve symptoms. It should be noted that lifestyle modification is beneficial for many patients with GERD, but alone is not able to control symptoms in most of them [12]. In this regard, the success of such therapy largely depends on the choice of antacid. Unlike PPIs and H2 blockers, antacids do not affect the acid production of the stomach, but have a neutralizing or buffering effect on the hydrochloric acid present in the stomach or entering the esophagus during GER. Modern antacids, in addition to the above, have a cytoprotective effect, stimulate the synthesis of prostaglandins and the secretion of bicarbonates [13], provide inactivation of pepsin, adsorption of bile acids and lysolecithin, decrease in intracavitary pressure in the stomach and duodenum, and improve esophageal clearance [14i]. One of the most effective non-absorbable antacid drugs is Maalox, which is a balanced combination of magnesium hydroxide and aluminum hydroxide. The drug is distinguished by a variety of forms and a pleasant taste. The mechanisms of its effectiveness in GERD are high acid-neutralizing ability (40.5 meq in 15 ml of suspension or 18.5 meq in 1 tablet), cytoprotective effect due to the binding of bile acids, cytotoxins, lysolecithin, activation of the synthesis of prostaglandins and glycoproteins, stimulation of the secretion of bi- carbonates and protective mucopolysaccharide mucus [15]. As part of a prospective multicenter, non-comparative, open study of the effectiveness and safety of Maalox in relieving symptoms of GERD (protocol ALUMI L 00697), we treated 20 patients. The purpose of the study was to evaluate the clinical effectiveness and safety of the antacid Maalox during long-term therapy in patients with an endoscopically negative form of GERD. Material and methods. We examined 20 patients (12 men, 8 women, average age 33.9±11.7 years, BMI 24.0±3.6) with GERD, grade 0 according to the Savary–Miller scale as modified by Carrison. After assessing the symptoms of the disease, general clinical examination and esophagogastroduodenoscopy, patients were prescribed a Maalox suspension 15 ml 4 times a day for 8 weeks, then 15 ml 2 times a day for 8 weeks, followed by observation for 8 weeks without treatment (Table 1 ). The dynamics of symptoms (heartburn, sour belching, bitterness in the mouth, heaviness in the epigastrium) were assessed on the Likert scale (Table 2), well-being on a visual analogue scale (VAS), quality of life (SF-36), as well as an assessment of adverse events . Results. While taking Maalox, there was a significant decrease in the severity of symptoms: heartburn on average from 6.8 points to 2.4 by the 16th week of therapy, sour belching from 2.6 to 0.8, bitterness in the mouth from 1 to 0, heaviness in the mouth. epigastrium from 1.2 to 0 (Fig. 1). A decrease in the severity of clinical manifestations was accompanied by an improvement in the well-being and quality of life of patients. At the same time, the most pronounced improvement in well-being according to VAS was observed against the background of 4 times the use of Maalox from 55.8 to 72.3 mm, followed by a slight decrease by the end of maintenance therapy to 68.6 mm. The most pronounced positive dynamics in quality of life indicators was noted on the RP and RE scales (Fig. 2). The first of them reflects the influence of physical condition on role functioning, that is, work, the performance of everyday activities. The RE scale characterizes the influence of the emotional state on role functioning and involves assessing the degree to which the emotional state interferes with the performance of work or other daily activities. After cessation of treatment, there was a gradual increase in the severity of the symptoms of the disease: heartburn up to 4.4 points, sour belching up to 2.4, heaviness in the epigastrium up to 0.6, bitterness in the mouth did not recur, which was generally reflected in a slight decrease in quality of life indicators and assessment state of health according to VAS up to 52.2 mm. It is known that the most common side effect of long-term use of antacids (especially aluminum-containing ones) is constipation. It should be emphasized that the latter has a certain pathogenetic significance in the development of GERD, since it contributes to an increase in intra-abdominal pressure, and, accordingly, an increase in GER. Maalox had no adverse effect on stool. In all treated patients, bowel movements remained daily, and there were no defecation difficulties. Discussion. The data obtained demonstrate the effectiveness of Maalox in long-term therapy of patients with an endoscopically negative form of GERD. Essentially, such patients require persistent relief of symptoms associated with GER. Our experience demonstrates the effectiveness of Maalox in controlling symptoms and, as a result, improving the well-being and quality of life of patients during regular use of the drug. The leading mechanism of action of Maalox in GERD is the modification of the stomach contents and, accordingly, the composition of the refluxant entering the esophagus during GERD: it neutralizes hydrochloric acid, absorbs pepsin, bile acids and lysolecithin. In addition, it helps to enhance the clearance of the esophagus and protects its mucosa from the damaging effects of the refluxant due to a complex of cytoprotective effects. Thanks to the latter, Maalox demonstrates high therapeutic efficacy not only in the endoscopically negative form of the disease, but also in erosive GERD, as was shown previously [13]. Conclusions. During Maalox therapy, a positive clinical effect was observed in all patients with an endoscopically negative form of GERD. Tolerability on average was rated as good. There were no adverse events associated with the use of Maalox. Maalox can be used for a course of treatment of patients with non-erosive GERD as an initial course of therapy as part of the “step-up” therapy strategy. RU.MAA.08.01.03
References 1. Vakil N., van Zanden SV, Kahrilas P., et al. The Montreal Definition and Classification of Gastroesophageal Reflux Disease: A Global Evidence–Based Consensus. Am J Gastroenterol 2006; 101:1900–1920 2. Lazebnik L.B., Bordin D.S., Masharova A.A. Modern understanding of gastroesophageal reflux disease: from Genval to Montreal. Exp. wedge. gastroenterol. 2007;5:4–10. 3. Locke GR, Talley NJ, Weaver AL, et al. A new question are for gastroesophageal reflux disease. Mayo Clin Proe 1994;69:539–47 4. Dent J, El-Serag HB, Wallander MA, et al. Epidemiology of gastro-oesophageal reflux disease: A systematic review. Gut 2005;54:710–7. 5. Lazebnik L.B., Vasiliev Yu.V., Manannikov I.V. Heartburn as one of the main criteria for GERD (results of one epidemiological study). Exp. wedge. gastroenterol. 2004;1:164–165. 6. Bor S., Lazebnik LB, Kutapcioglu G., et al. The prevalence of gastroesophageal reflux in Moscow. J Clin Gastroenterol 2006; 40(Suppl 4):S199. 7. Zimmerman Ya.S. Gastroesophageal reflux disease: state of the problem and controversial issues. Exp. wedge. gastroenterol. 2004;2:70–78. 8. Vigeri S., Tonini M., Scarpinato C., Savarino V. Improving opportunities for effective management of gastro-esophageal reflux disease. Dig. Liv. Dis. 2001;33:719–729. 9. Holtmann G. The clinical usefulness of PPIs: Are they all the some? (Yes) In: “PPIs: Are they all the some? – The Ultimate Debate.” – 10 UEGW, Absrtact Book. – Geneva, 2002.:10–11. 10. Bell NJV, Burget D, Howden CW et al. Appropriate acid suppression for the management of gastro-esophageal reflux disease. Digestion. 1992; 51(Suppl.1):59–67. 11. Moss SF, Armstrong D, Arnold R et al. GERD 2003 – a consensus on the way ahead. Digestion 2003;67(3):111–117. 12. DeVault KR, Castell DO Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. Am J Gastroenterol 2005;100: 190–200 13. Minushkin O.N. Antacids in the treatment of gastroesophageal reflux disease. Farmateka 2007;6 14. astroesophageal reflux disease. Ed. Maeva I.V. MGMSU, Moscow, 2000:36 15. Maev I.V., Samsonov A. et al. The place of Maalox in the treatment of functional dyspepsia syndrome. Doctor 2007;