Stage 4 liver cancer is an advanced cancer. It is impossible to completely cure such a patient. The doctor can only offer palliative therapy to relieve painful symptoms and prolong life.
The prognosis for patients in oncology is usually measured by five-year survival rate. It refers to the percentage of patients who are alive five years after their diagnosis.
For stage 4 liver cancer, the five-year survival rate ranges from 3 to 11%.
Briefly about the disease
According to statistics provided by the World Health Organization, the disease is widespread in the world (more than 700 thousand people are diagnosed annually) and is one of the leaders in the number of deaths from cancer (about 600 thousand people).
In liver cancer, metastasis processes are detected 30 times more often than primary cancer. It is difficult to treat at mature stages of development.
It affects men 3 times more often than women.
The average age of patients is 40-60 years.
Treatment
If we talk about methods of treating liver cancer, chemotherapy is primarily used. If this does not help, then surgical intervention is performed. The thing is that for liver cancer, surgery may be the only right solution. This is a radical way to get rid of the tumor once and for all.
But if we are talking about a secondary type of oncology and cases where the tumor has managed to metastasize to other organs, then in case of liver cancer, surgery does not always allow the tumor to be completely removed.
Chemotherapy for liver cancer kills malignant cells and prevents them from spreading. Sometimes several similar procedures are required. But it is quite difficult for the human body to cope with such a large load. Therefore, experts are trying to resort to an integrated approach in the treatment of liver cancer.
As for radiation therapy, there is no such method for treating liver cancer. It is simply not used due to poor effectiveness and increased sensitivity of the liver to radiation.
Primary and secondary cancer
In diagnosing liver cancer, in order to select a treatment method, it is important to identify its primary and secondary types.
Primary cancer is a pathology formed in the cellular structures of the gland. We are talking about stages 1 and 2 of the disease.
Primary cancer is:
- Hepatocellular carcinoma is the most common;
- Hemangiosarcoma - forms and develops in the blood vessels supplying the liver;
- Angiosarcoma - occurs infrequently, but is characterized by formation in people under 30 years of age;
- Cholangiocarcinoma - occurs in the bile duct;
- Hepatoblastoma – formed during fetal development;
- Hepatocellular carcinoma – more often found in men, appears in the liver epithelium.
A more severe form is secondary cancer. If it is present, metastasis processes are detected, i.e. These are stages 3 and 4 of the disease. As already noted, at this stage the disease is difficult to treat.
Unfortunately, the doctor has to deal with secondary cancer much more often than with primary cancer (95% to 5%), which means that the process of treating a patient causes many problems.
How long do people live with liver metastases: prognosis and life expectancy
to give an unambiguous answer to the question of how long people live with liver metastases
. A radical cure for stage IV cancer with distant metastases is impossible, so any antitumor treatment will be palliative.
The average life expectancy with liver metastases is about 3 years. With adequate and effective treatment, this figure could increase by an indefinite number of years.
The life expectancy of a patient with liver metastases is influenced by several factors: the degree of malignancy of the tumor, the location of the tumors and their size, the timeliness of contacting specialists, the correctness of the treatment regimen, the general status of the patient, and how the tumor will respond to treatment. The decision on the choice of treatment tactics for a patient with liver metastases is made by a council of doctors at our clinic individually in each case.
We make every effort, knowledge and achievements of modern oncology to help every patient with metastatic cancer
any localization. To make an appointment with an oncologist, please call the clinic numbers.
Causes
The true causes of the development of liver cancer have not been fully studied, however, this is also the case with other forms of oncology.
There are a number of factors that can lead to the disease, so people exposed to these factors are considered at risk.
The main risk factors are:
- Frequent drinking of alcohol;
- Tobacco smoking;
- Pathology in the body that is chronic in nature;
- Heredity;
- Hormonal imbalance;
- Mechanical damage to the liver;
- Metabolic disease;
- Intrauterine fetal development disorder;
- Presence of carcinogens.
Taking into account the above factors, we can safely say that among those at risk:
- Alcoholics;
- Drug addicts;
- Heavy smokers;
- People working in hazardous industries;
- People living for a long time in hazardous production areas;
- People living in areas with poor environmental conditions;
- Ignoring safety during promiscuity.
Liver cancer can occur due to a number of diseases, including:
- Inflammation of the gallbladder and bile ducts;
- Cholelithiasis;
- Acute form of hepatitis “B” and “C”;
- Acute inflammation that transforms the liver parenchyma into fibrous connective tissue;
- The presence of parasites in the liver;
- Syphilis.
It is useful for these categories to be periodically examined to detect liver cancer.
“Stage 4 liver cancer”: what does it mean?
Stage 4 liver cancer varies. Depending on how far the malignant tumor has spread in the body, two substages are distinguished:
- IVA: Cancer cells have spread to the lymph nodes that are near the liver.
- IVB: distant metastases were detected in other organs.
Most often, malignant liver tumors metastasize to the lymph nodes, portal vein (collects blood from part of the intestine and carries it to the liver), and lungs. Other localizations are much less common.
It is important to distinguish between concepts such as “liver cancer with metastases” and “metastatic liver cancer”. In the second case, we are also talking about a malignant tumor of the fourth stage, but the primary focus is in another organ, and its metastases are in the liver.
Symptoms
In the first stages of liver cancer, symptoms are absent or muted.
It is very important to pay attention to:
- Lack of attentiveness;
- Poor concentration;
- Constant feeling of fatigue.
Such conditions are not evidence of the presence of cancer, however, if they appear for more than a week, consult a doctor.
Further, as the disease develops and becomes a secondary cancer, the symptoms appear more clearly.
The disease makes itself felt:
- There is heaviness in the right side;
- Pain – in the right hypochondrium;
- Yellowish tints to the whites of the eyes and skin;
- Nausea;
- Vomit;
- Diarrhea;
- Swelling;
- Gas formation is increased;
- Loss of appetite;
- The temperature is constantly kept at 37.1-37.8.
If the disease has progressed to stage 4, its symptoms appear very sharply and, due to decreased immunity, can be supplemented by accompanying pathological processes. Remission in this case is extremely difficult to achieve - only 5% of cases.
Palate cancer
Liver cancer - symptoms and treatment
Treatment of liver cancer is a long, step-by-step process that does not always lead to a positive result. Treatment tactics depend on the stage of the oncological process, the presence of cirrhosis and concomitant disease.
The standard treatment for liver cancer is resection and transplantation . If patients cannot undergo liver resection, they have gone beyond the accepted criteria for transplantation or are awaiting a liver transplant, then they resort to non-resection locoregional therapy - local percutaneous treatment methods not associated with surgery:
- percutaneous injection of ethanol;
- radiofrequency ablation;
- transcatheter arterial embolization or transarterial chemoembolization;
- chemotherapy and immunotherapy;
- radiotherapy.
Liver resection
Resection is the removal of the entire tumor within healthy tissue. The only absolute contraindication to such an operation is affected lymph nodes and metastases (however, sometimes this criterion has exceptions). Relative contraindications to resection are:
- signs of severe liver failure - impaired liver function;
- insufficient volume of the liver remaining after resection, which cannot ensure its recovery and adequate functioning;
- tumor spread to the portal, hepatic or inferior vena cava [21][22][28].
Patients with normal liver parenchyma, the underlying tissue of the liver, can undergo extensive liver resection, but only if the remaining liver volume is sufficient for normal liver function.
Patients with early stage cirrhosis may also be candidates for resection, but this is rarely performed when there is sufficient remaining parenchyma [3]. If there is not enough remaining liver tissue, a two-stage operation :
- At the first stage, occlusion or ligation of the portal vein on the affected side is performed, which can be supplemented by transsection of the liver parenchyma (its dissection and suturing), which leads to an increase in the opposite lobe by 24-160% [29].
- In the second stage, the affected part of the liver is removed.
The main cause of relapse after liver resection is the formation of a new tumor against the background of cirrhosis. The frequency of such relapses is 30-70%. The main indicators that can predict poor survival and a high rate of relapse are the spread of the tumor through the vessels, severe fibrosis (liver cirrhosis) in the remaining parenchyma, as well as the absence of a tumor capsule and a low degree of differentiation of tumor cells [23].
If a focal intrahepatic tumor recurs, patients can sometimes undergo repeat resection. In some cases, single extrahepatic metastases in the lungs, diaphragm and abdominal wall can be resected, but only with a slowly progressing tumor [24].
Liver transplantation
Even after liver resection, there remains a high risk of disease recurrence. Therefore, some authors believe that the only radical treatment for liver cancer in the presence of cirrhosis is transplantation [26].
After the introduction of liver transplantation as the optimal treatment for active (decompensated) cirrhosis, it began to be considered as an option for the treatment of inoperable liver cancer, but early relapses often began to occur after surgery. Mazzaferro and others analyzed patients who underwent liver transplantation for grade B and C cirrhosis with a single tumor node ≤ 5 cm or three lesions with a maximum diameter ≤ 3 cm. The 4-year survival rate in these patients exceeded 85%, disease-free survival - 92% [18]. These features have been accepted as criteria for selecting patients for liver transplantation in the setting of cancer, but this study was small (48 patients) and none of the tumors had vascular invasion.
Subsequently, after observing 70 patients with liver cancer and cirrhosis who underwent transplantation at the University of California, San Francisco, different criteria : the presence of a single tumor < 6.5 cm or three lesions with the largest dimension ≤ 4.5 cm and a total tumor diameter ≤ 8 cm. Application of these criteria made it possible to achieve 5-year survival in 72.4% of cases [8].
There are now many criteria for liver transplantation. Most include a variety of markers such as AFP, PIVKA, etc.
You can estimate the prognosis of life expectancy after liver transplantation using special calculators. The most famous of them is The Metroticket Project from the founder of the Milan criteria , Mazzaferro. Life expectancy is calculated based on AFP data, the number of nodes and the maximum size of the node. You can view it on the official website of the Metroticket project [19].
Percutaneous ethanol injection
The introduction of ethanol into a tumor causes cell dehydration, necrosis and thrombosis of blood vessels, leading to the death of tumor cells. Some studies have shown patient survival rates similar to liver resection for very small tumors. However, cancer recurrence within two years with this treatment is 50%. Most relapses are new lesions in distant segments of the liver. Randomized trials have shown that this treatment is suitable for tumors ≤ 2 cm and causes fewer side effects than other ablative treatments [8].
Radiofrequency ablation
This method of tumor destruction involves the use of high temperature. Under ultrasound or CT control, a special needle-electrode with a non-insulated tip is inserted into the tumor. Under the influence of high-frequency alternating current, the tip heats up and leads to “dry” necrosis of the tissue around it.
Radiofrequency ablation can be performed percutaneously, laparoscopically (through a puncture), or through an open incision. Most effective for tumors < 3 cm in diameter.
Early relapse after tumor destruction is associated with a large tumor size, low differentiation, late stage of the disease, increased AFP and the presence of chronic hepatitis.
If the tumor is located near the bile ducts, radiofrequency ablation may be unsafe, as there is a high risk of biliary fistula formation. And if large vessels are located nearby, then the effectiveness of such treatment decreases: the vessel acts as a heat sink and reduces the temperature in the working area.
Dr. Mazzaferro noted that among a group of patients with tumors who underwent radiofrequency ablation followed by liver transplantation, 45% had evidence of residual liver cancer in the removed portion. Therefore, if liver resection and ablation are possible, resection should be chosen. However, when treating patients with small tumors (< 3 cm), with complex tumor localization and in the presence of cirrhosis, ablation is preferable, since it is associated with lower postoperative risks.
For patients who are not candidates for resection or whose tumor has recurred, ablation is the treatment of choice and can lead to long-term remission [8].
Transcatheter arterial embolization and transarterial chemoembolization
Transcatheter arterial embolization (TAE) involves blocking (occluding) the branch of the hepatic artery supplying the tumor, while transarterial chemoembolization (TACE) is a combination of arterial occlusion and intraarterial injection of a chemotherapy drug, most often doxorubicin. Chemotherapy agents may be administered prior to embolization or together with the gelatin sponges used for embolization [31].
TACE can increase life expectancy in patients with inoperable cancer [10]. This therapy is standard for patients who are not candidates for resection, transplantation, or ablation. Additionally, TACE can be used in combination with radiofrequency ablation and resection [15][25].
The rate of complications after TACE is as high as 23%, especially in patients with tumors >10 cm in diameter. After the operation, fever, nausea, and pain in the right hypochondrium are noted. Serious complications such as fatal liver necrosis and liver failure are rare. TACE is usually contraindicated in patients with ascites [16].
Chemotherapy and immunotherapy
Systemic chemotherapy has little activity against liver cancer. It is performed using one of the following drugs: 5-fluorouracil (5-FU), doxorubicin, cisplatin, vinblastine, etoposide, and mitoxantrone. It provides a response to treatment in 15-20% of cases. This response is usually temporary. Combination chemotherapy does not improve these results. The most active drug is doxorubicin, with an overall response rate of up to 19% [8].
When treating inoperable liver cancer with a combination of chemotherapy (doxorubicin, 5-FU) with immunomodulatory agents (alpha interferon), toxic effects occur, for example, myelosuppression - a decrease in white blood cells and platelets in the blood. But despite this, studies have shown its effectiveness: the tumor is reduced to a size that can be resected, and overall survival increases [14].
The recent SHARP trial showed that in patients with liver malignancy and preserved liver function (Child-Pugh class A), sorafenib increased 3-month survival compared with placebo. However, in a phase III study, there was no difference in disease-free survival after resection or ablation of liver cancer when sorafenib or placebo was used (mean 33.3 versus 33.7 months) [8].
Research on immunotherapy for liver cancer (atezolizumab, bevacizumab, etc.) is currently underway. In some cases, they significantly reduced the size of the tumor.
Radiation therapy
The safe dose for the liver is 30 Gy. Higher doses cause radiation hepatitis and liver failure. Therefore, radiation therapy was rarely used in the past. Currently, it is most promising for patients with inoperable tumors in the porta hepatis located near the portal vein or inferior vena cava, for whom radiofrequency ablation is not indicated.
To administer high doses to the center of the tumor, special equipment is used that allows for respiratory movements to be taken into account, which reduces the risk of damage to neighboring organs.
Radioembolization using labeled microspheres with the isotope yttrium-90 (Y90) has the advantage over external beam radiation: this method has a higher delivery to the tumor and higher radiation dose. The technique is similar to TACE, only radiolabeled particles - spheres 25 microns in size - are delivered to the tumor arterial vessels. The emitted radiation penetrates approximately 10 mm, the radiation dose is 150 Gy [5].
Studies have shown that patients who undergo Y90 radioembolization have a longer disease-free period (>26 months) compared with those who undergo TACE (6.8 months), but there is no difference in survival [27]. Radioembolization can be used as a bridge to liver transplantation.
Recent studies have demonstrated the feasibility of high-dose hypofractionated radiotherapy. In 91 patients with inoperable liver cancer or intrahepatic cholangiocarcinoma, this treatment method stopped tumor progression in 94.8% of cases. The 2-year survival rate was 63.2% [11].
How to choose a treatment method
The choice of appropriate treatment directly depends on the prevalence of the oncological process and the severity of liver failure.
Patients with a normally functioning liver or early stage cirrhosis are optimal candidates for liver resection. Before performing resection, it is necessary to calculate the residual volume of the hepatic parenchyma. If the volume is insufficient, it is advisable to consider performing a two-stage resection [17].
For patients with class B liver cirrhosis, non-extended liver resection is recommended, since extended liver resection is associated with high postoperative risks.
For patients with hepatocellular carcinoma within the Milan criteria for liver cirrhosis class B or C, it is advisable to undergo liver transplantation.
For inoperable cancer, it is necessary to consider non-resection locoregional therapy, which will increase life expectancy and, in some cases, wait for an organ to be transplanted.
Characteristics by stages
Stage 1. The most favorable for treatment: small tumor sizes, the area of segment damage is no more than ¼. The chances of recovery are high.
Stage 2. The neoplasm reaches sizes up to 5 centimeters. Adjacent liver segments are affected. The outer lining of the liver is destroyed. There is no metastasis. The survival prognosis is worse than at stage 1, but remains positive.
Stage 3. The tumor is up to 8 centimeters and has grown into neighboring tissues and organs. Secondary lesions appear. There is a decrease in immunity. Organs damaged by metastases malfunction.
Stage 4. The disease cannot be completely cured. The size of the tumor is over 8 centimeters. Metastases are spreading everywhere. The main systems of the body fail. If metastases penetrate the brain, life counts for months (3-4 months). If not, the patient can live up to 5 years.
Deviations in the intensity and completeness of breathing
The preagonia stage is accompanied by a decrease in respiratory rate and amplitude. This is due to inhibition of metabolic processes and a decrease in oxygen demand. The appearance of noise when inhaling and exhaling is a sign that there is fluid inside the lungs. In such situations, it is easier for the patient to breathe by turning him over to one side. The picture of a patient dying is described by the respiratory rate with so-called apnea intervals. To alleviate suffering, experts may suggest using an oxygen cushion, which will ensure the supply of oxygen. People caring for a dying cancer patient should systematically wet their lips and mouth with water.
Diagnostics
Diagnostic measures, as a rule, begin with an examination by a therapist or gastroenterologist.
The main task of this stage is to identify signs of oncology and prescribe additional studies, including:
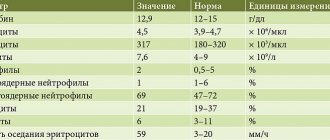
- Blood test, general and biochemical;
- Analysis of urine biomaterial.
If, based on the results of the tests, there is a suspicion of the presence of a tumor, the following is prescribed:
- Ultrasound;
- MRI;
- CT;
- Blood test for tumor markers;
- Biopsy.
After diagnostic measures, the doctor prescribes treatment.
Diagnosis of liver oncology
If the first symptoms of liver cancer appear, the doctor first performs a personal examination using the palpation method. Having noticed an increase in the size of the liver, its surface heterogeneity or compaction, the oncologist comes to the conclusion that the suspicion of a malignant tumor is confirmed. An ultrasound is performed and liver cells are taken for analysis. After this, a conclusion is prepared.
It is extremely important to begin timely treatment for liver cancer, since it is a dangerous and fast-growing disease. And the first symptoms of liver cancer that appear in you should be an important “bell” that it’s time to go to the clinic. Onko has a convenient location. It is located near Mayakovskaya metro station, Belorusskaya metro station, Novoslobodskaya metro station, Tverskaya metro station, Chekhovskaya metro station.
Combined treatment
In patients with chemosensitive liver metastases (breast cancer, testicular cancer, ovarian cancer), it is optimal to use surgery with preliminary chemotherapy and possible chemotherapy after surgery for isolated liver lesions.
Another treatment option may be surgery in combination with local exposure (radiofrequency thermal destruction, cryodestruction, injection of ethanol into the tumor, etc.)
Liver resection in combination with intravascular chemotherapy is another method of treating liver metastases.