Gallbladder cancer is a rare oncological disease that is not comparable to the frequency of damage to the gallbladder by a chronic inflammatory process.
There are no separate statistics on bladder cancer; it is included in the group of malignant tumors of the extrahepatic bile ducts, which affected 1,122 men and 2,180 women in Russia in 2013, which accounted for less than 1% of all malignant tumors. In the European Union, this disease accounts for no more than 5 cases per 100 thousand population. The annual increase in incidence is insignificant - just over 1%, but over the last decade, 12% more Russians have become sick with cancer. Isolated cases of cancer occur in children and young people, but the main group consists of patients over 50 years of age.
It’s paradoxical, but oncology statistics, which for half a century have been carefully taking into account all Russian malignant tumors, do not know about the group “gallbladder and extrahepatic bile ducts” mortality and detection by stages of the process.
Despite significant progress in the diagnosis of tumors and in high-tech surgery of the bile ducts, the weak point is precisely the diagnosis of cancer - the disease, as a rule, is detected in an advanced stage, when therapeutic measures are limited by the severity of the patient’s condition.
Causes of gallbladder cancer
Despite many years of study, the exact causes of the development of the disease are unknown. Most often, the development of this form of cancer is preceded by a long-term chronic form of cholelithiasis or cholecystitis.
Scientists also suggest that some chemicals in bile are carcinogens. In addition, the chances of malignant degeneration of cells increase with regular injuries to the mucous membrane from accumulated stones, chronic inflammation of the intrahepatic bile ducts, stagnation of bile, and disruption of the pancreas.
Factors that can trigger the development of the disease include:
- polyps;
- salmonellosis;
- infection of the body with E. coli;
- obesity;
- work in hazardous production;
- unhealthy diet (predominance of sweets, fried and fatty foods in the diet, lack of fiber);
- gallbladder cysts;
- bad habits.
Symptoms of gallbladder cancer
The insidiousness of the disease lies in the fact that in the early stages it is asymptomatic and the patient does not even realize that he has oncology. The first signs of gallbladder cancer are completely nonspecific; as a result, the tumor is often diagnosed too late, when it is already difficult to help the person.
The first symptoms of gallbladder cancer in men and women are as follows:
- flatulence, bloating;
- various stool disorders;
- severe nausea;
- constant feeling of heaviness in the abdomen, on the right;
- general weakness, malaise.
As the tumor grows, other, more specific symptoms of gallbladder cancer in women and men arise:
- severe pain in the abdomen on the right, which can radiate to the neck, back, shoulders;
- yellowing of the sclera of the eyes, skin;
- nausea without vomiting (sometimes vomiting occurs, but after it the patient’s condition does not improve);
- shortness of breath, which can occur even at rest;
- burning and itching of the skin;
- ascites;
- discoloration of feces, darkening of urine;
- general weakness, lethargy;
- sudden, causeless weight loss;
- constantly elevated body temperature.
There have been recorded cases where cancer of this type developed at lightning speed. Clinically, this was manifested by severe intoxication of the body and sepsis.
Gallbladder cancer stages
This type of oncology has five stages of development:
- Zero stage . The tumor is localized in the mucous membrane of the gallbladder. This is the initial stage of the disease, which is asymptomatic, which makes timely diagnosis difficult and worsens the prognosis. Cancer at this stage is usually discovered by chance during diagnostic tests for other diseases.
- First stage . The lesion is located on the mucous membrane, does not spread to the muscle layer, and does not grow into neighboring organs.
- Second stage . The tumor grows into the muscle layer of the gallbladder, but does not extend beyond the organ.
- Third stage . The tumor grows outside the organ or cancer cells enter nearby lymph nodes.
- Fourth stage . Lesions form in neighboring organs, and distant metastases appear.
TNM classification of gallbladder cancer
| Tis | Early asymptomatic stage |
| T1 | The neoplasm grows into the muscular or mucous layer of the gallbladder |
| T2 | The tumor grows into healthy tissue up to the serous layer |
| TK | The neoplasm grows into the serous membrane and begins to spread to the liver or visceral part of the peritoneum |
| T4 | The tumor grows in the liver tissue to a depth of more than two centimeters or begins to affect the digestive organs (extrahepatic bile ducts, stomach, omentum, etc.) |
Metastases:
| N0 | No metastases |
| N1 | Metastases in regional lymph nodes |
| N2 | Metastases in nearby organs |
| M0 | There are no metastases to distant organs |
| M1 | There are metastases to distant organs |
1 day before surgery
Drink only clear liquids
You will be required to follow a zero healing diet the day before surgery. Examples of clear liquids are shown in the table below. While following this diet:
- Don't eat solid foods.
- Drink enough fluids other than water, coffee and tea. Try to drink at least 1 glass (8 ounces (240 ml)) of fluid every hour you are awake.
| Can | It is forbidden | |
| Soups |
| Any food containing dried food particles or seasonings |
| Sweets |
| All other products |
| Beverages |
|
|
If necessary, begin bowel preparation
If your surgeon or nurse has told you that you will need a bowel preparation for surgery, you will need to start it 1 day before surgery. During bowel preparation:
- Don't eat solid foods.
- Drink enough fluids other than water, decaffeinated black coffee, and decaffeinated tea. Try to drink at least 1 glass (8 ounces (240 ml)) every hour while you're awake.
On the morning of surgery, mix all 238 grams of MiraLAX with 64 ounces (1.9 L) of clear liquid until the MiraLAX powder is completely dissolved. Once MiraLAX has dissolved, you can place the mixture in the refrigerator if desired.
MiraLAX will cause frequent bowel movements, so stay near the toilet the night before your surgery or procedure.
At 3:00 pm the day before your surgery, take 1 bisacodyl tablet with a glass of water.
At 5:00 pm the day before your surgery, start drinking MiraLAX Colon Cleanse. Drink 1 cup (8 ounces [240 ml]) of solution every 15 minutes until it runs out. When you finish drinking MiraLAX, drink 4-6 glasses of clear liquid. You can continue drinking clear liquids until midnight, but this is not necessary.
After each bowel movement, apply zinc oxide ointment or Desitin® to the skin around the anus. This will prevent irritation.
Write down the time for which the operation is scheduled
The Admitting Office will call you after 2:00 pm the day before your surgery. You will be told what time you should arrive for your surgery. If your surgery is scheduled for Monday, you will be called on Friday. If no one contacts you by 7:00 p.m., call 212-639-5014.
On the day of surgery, come to:
MSK Presurgical Center (PSC) 1275 York Avenue (between East 67th and East 68th Streets) New York, NY Elevator B, 6th Floor
Shower with Hibiclens
The evening before your surgery, shower with Hibiclens. To use Hibiclens, open the bottle and pour a small amount of solution into your hand or onto a terry cloth. Move away from the stream of water to avoid washing off Hibiclens immediately after application. Gently rub it into your body from neck to waist and rinse.
Do not allow the solution to come into contact with your eyes, ears, mouth or genital area. Do not use any other soap. After showering, dry off with a clean towel.
Eating and drinking before surgery
- Do not eat after midnight before your surgery. This also applies to hard candies and chewing gum.
- Between midnight and two hours before you are scheduled to arrive at the hospital, you can drink no more than 12 ounces (350 ml) of water (see illustration).
- Avoid eating or drinking two hours before your scheduled arrival time at the hospital. This also applies to water.
to come back to the beginning
Diagnosis of gallbladder cancer
If the doctor suspects that the patient has cancer of the gallbladder, the following laboratory and instrumental examinations may be prescribed to confirm the diagnosis:
Tests for gallbladder cancer
With their help, the amount of the main component of bile, bilirubin, and other chemical compounds in the blood that affect the functioning of internal organs, including the liver and gallbladder, are determined. In addition, the patient undergoes a special blood test for tumor markers of gallbladder cancer. These are chemicals that are synthesized by tumor cells. At later stages, the level of CA 19-9 and CEA markers in the patient’s body is significantly increased. An accurate diagnosis cannot be made with a single analysis of tumor markers, since they can be synthesized not only in cancer. Such tests are carried out both during diagnosis and during treatment of the disease to assess its effectiveness.
Duodenal sounding
Using this study, the structure of bile and digestive juices are studied. A probe is inserted into the patient's rectum to collect bile samples. This diagnostic method allows you to obtain quite a lot of information about the development of the tumor.
Ultrasound
Determining gallbladder cancer by ultrasound is an integral part of diagnosing this disease. Using ultrasound, the presence of stones in the gallbladder is detected, and the size and location of the tumor is determined.
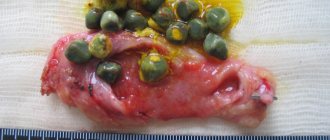
Biopsy
During this manipulation, pieces of gallbladder tissue are taken for subsequent microscopic examination. This diagnostic method allows you to accurately determine the type of tumor (benign or malignant) and the stage of the disease.
X-ray with contrast
Using this instrumental diagnostic method, the exact dimensions of the gallbladder, possible deformation of the organ, and the size of the tumor are determined.
MRI, CT
Highly effective, informative research methods. With their help, it is possible to detect even minor neoplasms at an early stage of development and determine the initial stages of metastasis.
After operation
In the hospital
You will wake up in the Post Anesthesia Care Unit (PACU). In most cases, patients remain in the recovery room overnight for observation.
When you wake up after surgery, you may have the following symptoms:
- IV-dropper for introducing fluids into the body;
- A Foley® catheter placed in the bladder to monitor the amount of urine produced. The Foley catheter should be removed 2 or 3 days after surgery.
- Compression boots on the feet to improve blood circulation. They will be removed when you are able to walk.
- A pain pump called a patient-controlled analgesia (PCA) machine. For more information, see Patient-Controlled Analgesia (PCA).
- A nasogastric (NG) tube that is inserted through the nose into the stomach. It removes gastric juice, which gives the stomach and intestines time to recover. Usually the probe is removed on the first or second day after surgery.
- Drainage tube for the outflow of bile. This drainage tube is usually removed a few days after surgery, but in some patients it may remain in place at discharge. If you still have it on discharge, your case manager will arrange for a visiting nurse to help you care for your drainage tube.
After your stay in the recovery room, you will be transferred to a hospital room on the inpatient unit. Here, your nurse will tell you how to recover from surgery. Below are some tips to help make this process safer.
- It is very important that you walk after surgery. It would be a good idea to set yourself a goal of walking every 2 hours. This will help prevent blood clots in the legs and stimulate bowel movements. Someone from the nursing staff will help you until you are able to walk on your own. You will be taught how to get out of bed without pain from your incisions (surgical cuts).
- Use an incentive spirometer. This will help expand the lungs, which will prevent the development of pneumonia. For more information, see How to Use Your Incentive Spirometer.
In most cases, patients who have this surgery remain in the hospital for 5–7 days.
Anesthesia
After surgery, you may experience pain in the area of the incisions. The doctor and nurse will ask you frequently about your pain and give you medicine as needed. If the pain does not go away, tell your doctor or nurse. Pain relief is essential so that you can clear your throat, breathe deeply, use your incentive spirometer, and get out of bed and walk.
Eating and drinking
You will not be able to eat for one to two days after surgery. You will then need to follow a zero healing diet. After this, you will gradually return to your normal diet.
Many people lose weight before surgery. As your appetite improves, you will gradually regain your previous weight. You may also gain weight immediately after surgery as your body retains water over the next few days.
At home
Before you are discharged, you will receive instructions and prescriptions from your doctor or nurse for the medications you need. Your nurse will review these instructions with you and give you a copy. If you require the assistance of a visiting nurse/health visitor at home, this assistance will be arranged for you before you are discharged.
Weakness
It is very common for patients to feel weak (unusually very tired or tired) for 6 to 8 weeks after surgery. Some of this weakness is due to the surgery you had and also because you may have lost weight before surgery. Over time, this symptom will gradually weaken.
Try to increase your activity level daily, this will help overcome weakness. Get out of bed, get dressed and walk. Gradually increase the distance you walk daily. If necessary, you can sleep during the day. However, try to stay awake as much as possible so that you can sleep at night. Your nurse will give you the resource Managing Cancer-related Fatigue.
Pain relief
You can get a prescription for pain medication. Take the medicine as directed by your doctor and as needed.
Do not drive or drink alcohol while you are taking prescription pain medication. Your doctor will tell you when you can drive again.
As the incision heals, the pain will become less severe and you will need less pain medication. A mild pain reliever such as acetaminophen (Tylenol®) or ibuprofen (Advil®) can be used to relieve pain and discomfort. However, taking acetaminophen in large quantities can harm the liver. Do not take more acetaminophen than is directed on the bottle, or take it as directed by your doctor or nurse.
Constipation
Painkillers may cause constipation (having bowel movements less frequently than usual). To prevent constipation, if possible, drink 8 glasses (8 ounces (240 ml) each, 2 L total) of fluid daily. Gradually increase the fiber content of your meals to 25–35 grams per day. Fiber is found in fruits, vegetables, whole grains and cereals.
You may also be given a prescription for docusate sodium (Colace®) 100 mg. Take _____ capsules _____ times daily. This remedy softens stool and causes few side effects. Do not take it with mineral oil.
If you have constipation, take 2 tablets of Senna (Senokot®) before bed. It is a stimulant laxative that may cause cramping.
If you haven't had a bowel movement in 2 days, call your doctor or nurse.
Caring for the incision
The location of the incision will depend on the type of surgery you had. If the skin around the incision is numb, this is normal because some of the nerve endings were cut off during surgery. Over time, this feeling will pass.
- If there is discharge from the incision, you should record the amount and color. Call your doctor's office and talk to a nurse about discharge from your incision.
- Change the dressing at least once a day and more often if it becomes wet from discharge. If the discharge from the incisions has stopped, you can leave them open.
- If you go home with Steri-StripsTM on your incision, they will come off and fall off on their own. If they don't fall off after 10 days, you can remove them.
- If you go home with glue on the seam, it will also come off on its own, like Steri-Strips.
Physical activity
Exercise will help you gain strength and improve your well-being. Walking and climbing stairs are excellent forms of exercise. Gradually increase the distance you walk. Check with your doctor or nurse before doing more intense exercise.
Check with your doctor before lifting weights. In most cases, you should not lift anything heavier than 10 pounds for at least 6 weeks.
We also recommend that you perform exercises to relieve tightness in the incision area. They also use the muscles that were cut during surgery. To do these exercises:
- Stand up straight and slowly lean back. This will stretch the incision on the abdominal wall.
- Return to the starting position and lean to one side.
- Return to the starting position and bend to the other side.
Repeat this exercise several times a day. It will help reduce discomfort from the surgery.
Follow-up appointment
Typically, the first follow-up visit is scheduled 10 to 14 days after discharge. Call your doctor to make an appointment.
to come back to the beginning
Treatment methods for gallbladder cancer
After receiving the results of all examinations, doctors make a final diagnosis, identifying the type of tumor and stage of the disease. The effectiveness of treatment largely depends on how accurately the diagnosis is made.
Therapy is prescribed individually for each patient, depending on the severity of the disease, age, and the presence of concomitant diseases. The fight against cancer is a complex task that requires the participation of a large number of specialists. In addition to the oncologist, this may include a chemotherapist, surgeon, radiotherapist and others. To achieve the best possible result, specialists constantly contact each other, exchange professional opinions, and decide on the choice of therapy method.
For this type of cancer, the following treatment methods are used:
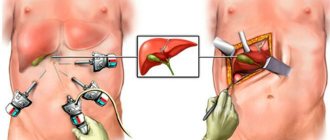
Surgery for gallbladder cancer
There are two main types of surgical procedures. The former help to completely cure cancer (they are usually used in the early stages), the latter alleviate the symptoms of the disease and improve the patient’s quality of life.
In the first case, cholecystectomy (surgical removal of the gallbladder) is usually prescribed. Now this operation is performed laparoscopically through small incisions in the abdominal wall or classically through a large incision. In some cases, if the tumor has grown into neighboring organs, in addition to the gallbladder, part of the liver, lymph nodes, bile duct, duodenum, pancreas, and other tissues are removed.
Radiation therapy
This is the destruction of tumor cells using radiation. This technique is used in the following cases:
- as part of complex therapy for advanced forms of oncology;
- after surgery;
- to reduce the size of the tumor and alleviate the condition of patients in the last stages of the disease.
Palliative care
It is aimed at relieving the main symptoms of the disease in the later stages, when it is no longer possible to cure the patient. The patient is given medications for skin itching, nausea, strong painkillers, and, if necessary, surgery or radiation therapy is performed to reduce the size of the tumor. As a result, it stops putting pressure on organs, blood vessels and nerves, and the patient’s condition temporarily improves.
Before surgery
Preoperative study
You will be scheduled for presurgical testing (PST). The date, time, and location of your preoperative test will be indicated on the reminder you receive from your surgeon's office.
On the day of your preoperative test, you can take food and medications as usual. During this visit, you will meet with an advanced practice nurse who works closely with the anesthesia team (specialized doctors and nurses who will give you medicine to help you sleep during surgery).
A nurse practitioner will review your medical record and surgical history with you. You will need a number of tests, including an electrocardiogram (ECG) to check your heart rhythm, a chest X-ray, blood tests, and other tests needed to plan your treatment. Your advanced practice nurse may also refer you to other health care professionals.
Your nurse practitioner will tell you what medications you will need to take on the morning of your surgery.
When going to preoperative testing, take the following with you:
- a list of all medications you take, including patches and creams;
- results of any tests you had outside of MSK, such as a stress ECG, echocardiogram, or carotid Doppler ultrasound;
- the names and telephone numbers of your doctors.
You will also be given the materials “Getting Ready for Surgery,” “Common Medications Containing Aspirin and Other Nonsteroidal Anti-inflammatory Drugs (NSAIDs),” and “ Herbal Remedies and Cancer Treatment. These resources provide more detailed information about how to prepare for surgery.
Buy Hibiclens® Skin Cleanser
Hibiclens is a skin cleanser that kills infectious agents and prevents their reappearance within 24 hours after use. By showering with Hibiclens before surgery, you will reduce the risk of infection after surgery. You can purchase Hibiclens at your local pharmacy without a prescription.
If necessary, buy everything you need for bowel preparation
If you need to prepare your bowels before surgery, your nurse will tell you how to do it. You will need the following:
- 1 (5 mg) tablet bisacodyl (Dulcolax®). They are usually sold in packs of 10 tablets.
- 1 bottle (238 g) polyethylene glycol (MiraLAX).
- 1 bottle (64 oz or 1.9 L) clear liquid.
to come back to the beginning
Survival prognosis for gallbladder cancer
Unfortunately, the prognosis for this type of cancer is poor. Only 10 out of 100 people will live 5 or more years after diagnosis. The prognosis largely depends on the stage of the disease. In the later stages, this type of cancer cannot be treated, but in the early stages there is a good chance of completely defeating the cancer.
Below is a forecast of five-year survival after this type of cancer by stage:
- stage zero - prognosis 80%, that is, 80 out of 100 people survive;
- first stage - prognosis 50%, the patient undergoes surgery to resect the gallbladder, which avoids the development of relapses of the disease;
- second stage - prognosis 25%;
- third and fourth stages - prognosis less than 10%.
Prevention of gastric cancer
There is no specific prevention for this disease. You can reduce your chances of developing cancer by following these recommendations:
- proper nutrition;
- giving up bad habits (alcohol abuse, smoking);
- giving up a sedentary lifestyle and exercising;
- compliance with safety regulations when working in hazardous industries;
- compliance with the work and rest regime;
- body weight control, preventing the development of obesity;
- timely treatment of diseases that may be complicated by cancer of the head of the gallbladder;
- Regular preventive examinations will help identify possible health problems in the early stages, which will significantly facilitate subsequent treatment and improve the prognosis.
Information verified by an expert
Mikhailov Alexey Gennadievich operating oncologist, doctor of the highest qualification category, Ph.D. experience: 21 years
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
How to make an appointment with a specialist in oncology
To make an appointment with a specialist for a consultation or to carry out a full diagnosis, you can use a special form that is available on the website of the oncology center. You can see a doctor by calling: +. We are located in the central district of Moscow, at the address: 2nd Tverskoy-Yamskaya lane 10 (Mayakovskaya metro station, Belorusskaya metro station, Novoslobodskaya metro station, Tverskaya metro station, Chekhovskaya metro station). When a disease is detected, doctors immediately prescribe treatment and further monitor the patient.