Chronic atrophic gastritis is a disease characterized by atrophy of the gastric glands, degeneration of the gastric epithelium into the intestinal epithelium, and a moderately severe inflammatory process. Manifestations depend on the localization and etiology of atrophic processes: mainly, heaviness in the stomach after eating, rapid satiety, belching, nausea, unpleasant taste in the mouth, anemia. The gold standard for diagnosis is endoscopy with mucosal biopsy, intragastric pH-metry, detection of H. pylori; the remaining methods are auxiliary. Treatment consists of the administration of glucocorticoid hormones, natural gastric juice, vitamin B12, and the use of an anti-Helicobacter therapy regimen.
Forms and stages of the disease
There are acute and chronic types of alcoholic gastritis. It can be either hypoacid, that is, a person does not produce enough gastric secretion, or hyperacid, when the patient has high acidity. Constant irritation of the mucous membrane by alcohol often ends in the formation of superficial erosions on the inner wall of the organ. If wounds are found on the membrane, then the person develops erosive alcoholic acute gastritis.
The chronic form of the disease has 2 phases - remission and exacerbation . Each type and phase of alcoholic gastritis differs in its symptoms. The form and stage of the disease determines which medications doctors will use in the treatment regimen.
Risk group for alcoholic gastropathy
The disease causes serious disturbances in the functioning of the stomach. Most often, such gastritis develops in people with alcohol dependence. At risk are women aged 75 to 80 years and 60-65 year old men. Medical statistics indicate that alcoholic gastritis ranks 19th in frequency and danger among gastrointestinal pathologies. For 0.4% of people, this disease resulted in death.
Risk factors and causes of development
The pathology is provoked by the consumption of alcohol-containing drinks. Clinicians have found that the cause of the acute form of alcoholic gastritis is a single consumption of a large dose of ethanol, significantly exceeding the individual norm. It can happen in both alcoholics and alcohol-dependent people. Therefore, patients often confuse such gastritis with alcohol poisoning and do not begin treatment after the attack is over.
Chronic gastropathy develops slowly due to constant drinking of alcoholic beverages. Regular ingestion of alcohol into the stomach first inhibits the secretion and motility of the organ, and then provokes the death of glandular cells without their subsequent rebirth (atrophy of the membrane).
Risk factors include drinking alcohol over 20 proof and not eating snacks. Such drinks take longer to be absorbed by the membrane, which increases the duration of contact of the mucous membrane with ethanol, and refusal to eat increases the degree of intoxication. If a person is stressed, overworked, exhausted, smokes, works with harmful substances, or has other gastrointestinal pathologies, the risk of developing alcoholic gastritis increases.
Causes
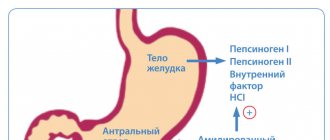
The most significant causes of chronic atrophic gastritis are H. pylori infection and autoimmune processes. Atrophy of the gastric epithelium develops in the late stages of chronic Helicobacter-associated gastritis. The bacteria first colonize the antral mucosa, causing a chronic inflammatory response. As the infection progresses, the process spreads first to the body of the stomach, and then to its remaining parts, initiating pangastritis. At this stage, atrophic changes in the mucous membrane are clearly visualized, and chronic atrophic gastritis is formed. Usually at this stage, Helicobacter pylori ceases to be detected, since the gastric glands atrophy, and the gastric epithelium is replaced with intestinal epithelium, to which H. pylori has no tropism.
In autoimmune gastritis, damage to the main gastric glands is observed at the onset of the disease. Diffuse atrophy of the gastric epithelium progresses very quickly, which is associated with the production of autoantibodies to microsomal antigens of parietal cells, gastrin-binding proteins, and intrinsic factor. Antibodies are directly involved in the destruction of gastric epithelial cells.
The cause of the formation of autoantibodies has not been determined to date, but gastroenterologists do not exclude a hereditary predisposition to chronic atrophic gastritis. It is known that in order to start an autoimmune process in the gastric epithelium, the antibody titer must reach a certain critical figure, individual for each person. Various endogenous and exogenous provoking factors can affect the speed of this process:
- Endogenous factors: genetic characteristics, duodenogastric reflux, endointoxication, oxygen starvation, chronic infections, metabolic and endocrine disorders, vitamin deficiency (hypovitaminosis), visceral reflex reactions in pathologies of other organs.
- Exogenous factors: nutritional disorders, bad habits (alcohol, smoking), taking certain medications, exposure to ionizing radiation, infectious agents (bacteria, fungi, parasites).
Symptoms
The chronic form of the pathology in the remission phase may not manifest itself in anything. Sometimes vague symptoms that are common to all gastritis occur. Most often, patients with chronic alcoholic gastritis experience discomfort in the stomach, nausea, loss of appetite, and indigestion. If there is blood in the vomit, then an erosive type of disease develops.
Chronic alcoholic gastritis - symptoms in the acute stage:
- the degree of pain increases;
- nausea and/or vomiting in the morning (on an empty stomach), which in alcohol-dependent people stops drinking alcohol;
- scanty liquid vomit may contain bile and mucus;
- unquenchable thirst, dry mouth;
- refusal of food due to aversion to it;
- weakness, heaviness in the stomach;
- esophagitis (inflammation of the esophageal mucosa), burning sensation behind the sternum;
- belching with a sour taste, heartburn , constipation predominates ;
- with gastric insufficiency - flatulence , heaviness in the epigastrium, gases escaping through the mouth have a rotten smell.
The pain syndrome becomes aching, the severity of which intensifies after eating. Discomfort in the pit of the stomach can be constant, temporary, or “floating” (occurs periodically in different parts of the gastrointestinal tract). The pain is often relieved after a bout of vomiting.
Symptoms of acute alcoholic gastritis:
- signs of poisoning;
- “hungry” cutting pains;
- repeated vomiting ;
- frequent heartburn ;
- constant regurgitation (stomach contents entering the larynx) and belching ;
- regular constipation (less often diarrhea ).
For alcohol addicts, the main confirmation of gastropathy is that after drinking alcohol, all signs of the disease become blurred or disappear altogether. But if such gastritis did not occur in an alcoholic, then drinking an alcohol-containing drink will exacerbate the symptoms.
A laboratory sign of alcoholic gastropathy is an increase in the blood levels of immunoglobulins (Ig) A, red blood cells, transferrin and the activity of aspartate aminotransferase, gamma-glutamyl transpeptidase. On palpation, sagging abdominal muscles (muscle atrophy) and pain in the epigastric region (in the pit of the stomach) are felt. A diagnostic sign of the chronic form of alcoholic gastritis is also the presence of tachycardia, shortness of breath, and polyneuropathy.
General information
Chronic atrophic gastritis is a morphological diagnosis, for verification of which the results of endoscopy are required. The clinical manifestations of this pathology do not always correspond to the changes detected during a biopsy. Chronic atrophic gastritis can develop both in the late stages of Helicobacter pylori gastritis (due to long-term persistence of the infection, a significant number of gastric glands gradually die) and as a result of autoimmune disorders in the body (antibodies to the epithelial cells of the stomach cause their death, achlorhydria gradually develops).
H.pylori is detected in more than 80% of the Russian population, while chronic inflammation of the gastric mucosa is found in approximately 50%. Autoimmune gastritis is diagnosed in women three times more often than in men, but is a fairly rare disease. Research in the field of gastroenterology confirms that the incidence of chronic gastritis is increasing by 1.5% annually.
Chronic atrophic gastritis
Nutrition
In the acute form of reactive alcoholic gastropathy, for the first 2 days after admission to the hospital, a person is prescribed a strict diet ( table No. 1-a according to Pevzner ). During this period, you can only drink boiled or still mineral water and weak tea in small portions. The liquid is heated to a temperature of about 37° C before use.
For gastritis with high acidity, you need to drink alkaline (hydrocarbonate) mineral water ( Borjomi , Smirnovskaya and others), and for gastric insufficiency - sodium chloride ( Narzan , Mirgorodskaya , Essentuki No. 4 or 17 ).
On day 3, boiled pureed foods are introduced into the diet. You are allowed to eat only jelly, porridge, and soup. After an attack of gastric insufficiency is relieved, diluted milk and low-fat dairy products, boiled dietary meat, fish, vegetables, and fresh tomatoes are gradually added to the menu. If a person has been diagnosed with hypersecretion of acid, then cream can be added to dishes. The patient is transferred to gentle nutrition according to Pevzner table No. 1 as the pathology subsides.
People with chronic alcoholic gastropathy follow diet No. 1 until the disease is cured.
If you have gastritis with normal or impaired gastric secretion, you should not eat foods that irritate the mucous membrane of the organ. These are hot, sour, spicy, fried, poorly cooked and fatty foods, raw vegetables or fruits.
Operations to eliminate the disease
If alcoholic gastritis is confirmed without the presence of malignant neoplasms, surgical treatment is not used. Therapy for this disease is carried out only by conservative methods.
Drug therapy
In case of acute alcoholic gastritis, drugs are prescribed for detoxification (cleansing the body of decay products and other harmful substances), rehydration (restoration of water and electrolyte balance) and medications, the action of which is aimed at restoring the tissues of the gastric mucosa.
The following medications are included in the treatment regimen:
- Gastroprotectors ( Sucralfate , Solcoseryl , other agents). The use of the cytoprotector “ De-nol ”, which has a complex effect on the gastric mucosa, is effective. It promotes the regeneration of damaged membranes, contains bismuth, reduces secretion, suppresses H. Pylori bacteria, and relieves inflammation.
- Acidity regulators. For hypoacid gastritis, secretion stimulants are prescribed ( Eufillin , Plantaglucid , herbal and other drugs), and people with high stomach acidity are prescribed antacids, a proton pump inhibitor ( Almagel Neo , Ranitidine , Maalox , Phosphalugel , Omeprazole ).
- Enzyme enzymes. Festal , Pepfiz , Abomin , Creon and similar drugs are used in replacement therapy
- Bismuth preparations ( Novobismol ).
- Medications for infusion treatment. Using a dropper or syringe, prescribed medications are infused into the blood vessel for detoxification and rehydration. Regidron , Gidrovit and other solutions that restore water and electrolyte balance can be drunk or administered into the stomach through a nasogastric tube.
For patients diagnosed with alcoholic gastritis, treatment is supplemented with symptomatic therapy. This includes:
- Motilium and Cerucal give good results ;
- carminatives - dill infusion, Espumisan , and other drugs help with flatulence;
- antispasmodics - Papaverine , Drotaverine and No-shpu ;
- prokinetics - to improve motor skills, Metoclopramide , Motorix , and so on are prescribed;
- antihistamines - use Diazolin , other drugs if allergic reactions occur;
- sedatives - also prescribed as needed to calm the nervous system (valerian, Amitriptyline ).
B vitamins or vitamin-mineral complexes are always included in the treatment regimen. They participate in metabolic processes, so timely replenishment of nutrients accelerates the metabolism and nutrition of mucosal cells, as well as the restoration of its tissue.
Supportive treatments
This includes non-drug methods: physiotherapy and traditional medicine. The same physiotherapy procedures and medicinal plants are used as for other types of gastritis.
When selecting traditional medicine, immediately exclude all recipes using alcohol.
infusions with plantain, St. John's wort , aloe juice , honey and butter effectively restore the mucous membrane A decoction of marsh cucumber reduces acidity well, and chamomile with calendula cleanses the body.
Physiotherapy is carried out only to prevent exacerbations. For hyperanacidic gastropathy, UHF and electrophoresis , and if the patient has gastric insufficiency or preserved secretion, then mud and ozokerite applications .
Important
For medical help in case of alcoholic gastritis, you should contact a gastroenterologist. When selecting medications, he takes into account the condition of the liver, pancreas, and kidneys. Such an assessment is mandatory, since many medications for the treatment of this pathology can only be used if the functions of the digestive and urinary organs are preserved.
Considering the cases of death and frequent complications of alcoholic gastritis (ulcers, atrophy of the mucous membrane, stomach cancer, other dangerous pathologies), you cannot refuse medical care and self-medicate.
It is also important to remember that this disease can be eliminated only with the help of medications and diet, and physiotherapy, folk and traditional medicine are used only as auxiliary methods and to prevent exacerbations.
Prognosis and prevention
The prognosis for chronic atrophic gastritis depends on many factors: the degree of H. pylori contamination and mucosal atrophy, etc. Helicobacter pylori infection is the initial link in the pathological process, which in the future can lead to stomach cancer. In the initial stages, mucosal atrophy can be prevented or stopped; it is at this stage that most patients seek medical help.
The eradication of H. pylori before the onset of atrophy of the gastric mucosa, as well as timely initiation of treatment for pernicious anemia, can significantly improve the prognosis. At the stage of intestinal metaplasia, the risk of malignancy is extremely high. Prevention of chronic atrophic gastritis involves timely detection and treatment of H. pylori infection and elimination of other risk factors for this disease.
You can share your medical history, what helped you in the treatment of chronic atrophic gastritis.