Gastritis is an inflammatory or inflammatory-dystrophic disease that affects the inner surface of the stomach. Normally, the mucous membrane lines the entire surface of the organ and plays an important role in the digestion process. Its glands are capable of producing hydrochloric acid, bicarbonate, gastric juice, lipase, the enzyme pepsin and other substances responsible for protecting the body from pathogenic microorganisms, activating metabolic processes in the body, and breaking down fats and proteins.
Classification of the disease
There are many types of pathology, but according to the severity of the signs of the disease, the degree of damage to the mucous membrane, and the frequency of symptoms, acute and chronic gastritis are distinguished. In the first case we are talking about a newly diagnosed disease, in the second - about repeated attacks of the disease.
Acute gastritis can be:
- Catarrhal.
- Fibrinous.
- Corrosive.
- Phlegmonous.
Chronic gastritis is divided into the following types:
- Bacterial. The cause of the development of pathology is the bacterium Helicobacter Pylori. The pathogen is resistant to the acidic environment of the organ and lives on its inner surface.
- Chemical. This type of gastritis occurs due to the aggressive effects of substances of endogenous and exogenous origin - bile, alcoholic beverages, some medications, various toxic substances.
- Autoimmune. It develops as a result of the erroneous influence of immune system cells on a person’s own tissues.
In rare cases, types of gastritis such as granulomatous, resection, lymphocytic, and radiation are diagnosed. Considering the degree of damage to the gastric mucosa, superficial, widespread, deep and erosive varieties of chronic gastritis are distinguished. Depending on the amount of hydrochloric acid in gastric juice, pathology may be accompanied by low or high acidity.
Methods for diagnosing and treating gastritis
- Consultation with a gastroenterologist
- Test for Helicobacter pylori
- FGSD (gastroscopy)
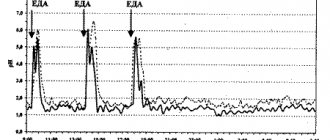
- Daily pH monitoring for gastrointestinal examination
- Colonoscopy
The diagnosis is made exclusively by a gastroenterologist based on the patient’s complaints, as well as data from the gastroscopy required in this case.
When treating gastritis, it is necessary to follow a diet that recommends eating at the same time about five times a day. Excluding alcoholic drinks, fatty meats, smoked meats, and shortcrust pastry products. It is very important to stop smoking and drinking alcohol when gastritis occurs.
Experienced doctors at SM-Clinic are ready to assist you in the treatment of diseases of the gastrointestinal tract. You can make an appointment 24 hours a day.
Sources:
- I'M WITH. Zimmerman, Yu.A. Zakharova. Problematic issues of the doctrine of chronic gastritis // Clinical medicine, 2022, No. 95(1), pp. 8-14.
- Sh.Z. Galiev, N.B. Amirov, O.A. Baranova. Morphological signs of reflux gastritis // Kazan Medical Journal, 2022, v. 98, no. 4, pp. 533-537.
- Coati I, Fassan M, Farinati F, Graham DY, Genta RM, Rugge M. Autoimmune gastritis: Pathologist's viewpoint // World J Gastroenterol. 2015 Nov 14;21(42):12179-89. doi: 10.3748/wjg.v21.i42.12179.
Complications of gastritis
If you do not take into account the doctor’s recommendations, inadequate treatment can cause serious consequences:
- Peptic ulcer disease. Most often it appears in the erosive form of the disease.
- Atrophic gastritis. Due to the low concentration of hydrochloric acid, the glands of the mucous membrane almost completely lose their ability to produce secretions and begin to be replaced by connective tissue. Refers to precancerous conditions.
- Gastric bleeding due to ulcers or erosions. It is characterized by shortness of breath, pale skin, weakness, the presence of blood in the vomit and black liquid stool. Refers to conditions requiring emergency medical care.
- Lack of vitamin B12 and folic acid. It occurs in the autoimmune form of the disease or in the advanced stage of atrophic gastritis, when the stomach glands stop producing the protein responsible for the absorption of vitamin B12.
- Anemia. It develops as a result of acute or chronic blood loss, as well as due to poor absorption of vitamin B12 from food by the body.
What symptoms indicate the presence of chronic atrophic gastritis?
The main evidence of the danger of chronic atrophic gastritis, exacerbation, is the absence of clear signs in the early stages. There is not even any pain that could prompt the patient to go to the doctor. The signs of this form of gastritis in adults are not specific and are considered the same for all types of this disease. The main complaint is a feeling of heaviness in the stomach that occurs after eating. But according to the degree of spread of chronic atrophic gastritis, the patient develops symptoms that help establish the full picture.
chronic focal atrophic gastritis symptoms
For example, dyspeptic syndrome, manifested by:
- heaviness and dull nagging pain in the upper abdomen,
- heartburn,
- burping,
- nausea and vomiting with mucus and bile,
- bloating.
Also, one of the signs of this condition is a decline or loss of appetite.
It should be added that digestive failure also occurs in other places in the gastrointestinal tract. The patient feels discomfort, stomach rumbling, stool becomes irregular: either diarrhea or constipation. There is a gray coating on the tongue with teeth marks, and an unpleasant taste and smell appears in the mouth. Due to the fact that the absorption of iron and vitamins is impaired, anemia syndrome is formed. It is manifested by weakness, fatigue, drowsiness, pallor of the skin and mucous membranes. The patient suffers from pain and tingling in the tongue area, and there is a loss of sensitivity in the limbs. Hair becomes dry, nails begin to break, shortness of breath and heart pain occur.
Causes of the disease
There are many factors that contribute to the development of the disease; they can be divided into two groups: endogenous (internal) and exogenous (external) causes.
Endogenous factors
Among internal causes, duodenal reflux and autoimmune processes in the body are of particular importance. With one pathology or another, a change in pH level is observed, which leads to irritation of the gastric mucosa and the development of an inflammatory process. Also play an important role:
- genetic predisposition of a person;
- the presence of parasites in the body;
- dental problems such as missing teeth, caries, malocclusion;
- endocrine diseases, sarcoidosis
- intolerance to dairy and soy products;
- HIV AIDS.
Exogenous causes
Gastritis can be caused by dietary disturbances, as well as by:
- the predominance of fried, smoked, spicy or fatty foods in the menu with a large number of preservatives and dyes;
- bad habits;
- age-related changes;
- constant use of corticosteroid drugs, NSAIDs, aspirin;
- chronic stress and depression.
University
→ Home → University → University in the media → Variants of the course of chronic gastritis
The photo is for illustrative purposes only. From the MV archive
Ivan Bronovets, Professor of the Department of Cardiology and Internal Medicine of BSMU, Doctor of Medicine. sciences
Chronic gastritis (CG) is a recurrent focal or diffuse inflammation of the mucous and submucosal membrane of the stomach, accompanied by impaired regeneration, with a tendency to progression, the development of atrophy and secretory failure. The main changes occur in the mucous membrane, so the functional morphology of the mucosa, and not the entire stomach, is studied.
Chronic gastritis occupies a leading place among diseases of the digestive system. Various variants of the pathology are diagnosed in 50–75% of patients over 45 years of age.
Classification
The Sydney classification of gastritis (1990), modified in Houston (1994), has received general recognition. It combines etiological, topographical and morphological principles for assessing the disease. According to the etiology, CG is divided into Helicobacter pylori (type B), autoimmune (type A), chemical or reflux gastritis (type C) and special forms (lymphocytic, radiocytic, granulomatous, eosinophilic gastritis, etc.).
Topographically, gastritis is distinguished between the body of the stomach, antrum, fundus and/or all parts of the stomach (pangastritis). Based on morphological characteristics, the presence and degree of inflammation, atrophy, metaplasia, and contamination with Helicobacter pylori (HP) bacteria are assessed. Gastritis is divided into erosive and non-erosive. CG can be superficial and deep (transmural).
In addition to the main etiological factors in the development and progression of chronic hepatitis, poor diet, rough food, abuse of spices, alcohol, smoking, systematic trauma to the gastric mucosa with poorly chopped food, hasty eating, etc. play a role.
Helicobacter pylori gas mainly affects the antrum of the stomach. HP is most often detected on the surface epithelium under a layer of mucus (superficial gastritis) and much less frequently in atrophic gastritis.
The main morphological feature of this type of gastritis is the presence of HP in the bicillary form and in the form of cocci on the mucous membrane. The surface epithelium is affected, and leukocyte infiltration appears. The determination of HP and the degree of contamination of the antrum are important in diagnosis. The gold standard for diagnosis is the examination of biopsy specimens not only from the antrum, but also from the area of the body of the stomach.
Autoimmune CG is much less common than HP-associated. Diagnosed in 16% of patients with macrocytic hyperchromic (pernicious) anemia. A characteristic feature is the localization of changes in the fundus of the stomach, while the antrum remains unaffected.
This leads to a sharp decrease in acidity and internal factor. Intrinsic factor deficiency causes malabsorption of vitamin B12 and the development of pernicious anemia. Severe atrophic gastritis develops with progressive loss of parietal cell mass.
It proceeds unsystematically until one of the complications develops (vitamin B12 deficiency or malignant lesions of the stomach); metaplasia appears. At the final stage, complete metaplastic replacement of the mucous membrane is noted. Antibody titers to parietal cells and intrinsic factor and achlorhydria are detected.
Reflux gastritis is associated with the reflux of duodenal contents into the stomach, damaging its mucous membrane. True reflux gastritis develops in patients who have undergone gastrectomy.
A synonym for reflux gastritis is alkaline gastritis. It is not entirely accurate, since the main role in damage to the gastric mucosa is played not by the alkaline properties of the intestinal contents, but by the characteristics of bile acids. In addition, a necessary condition for the development of gastritis is the presence of hydrochloric acid.
The main component of duodenal contents is bile acids, their salts, pancreatic enzymes and lysolecithin. Bile acids cause damage to the protective gastric mucus barrier by increasing the back diffusion of hydrogen ions, and when gastric secretion is low, pancreatic enzymes can also damage the gastric mucosa.
In case of chronic hepatitis, especially progressive one, metaplasia of the gastric mucosa of the intestinal type often occurs. We are talking about replacing the gastric epithelium with intestinal epithelium. With atrophic gastritis and gastric cancer, metaplasia is observed in almost 100% of cases. Currently, it is customary to distinguish two types of metaplasia: complete, resembling the small intestine, and incomplete (large). The presence of Paneth cells is the most important sign of complete intestinal metaplasia.
Diagnostics
To make a clinical diagnosis, it is necessary to correctly diagnose the type of hCG, assess the degree and prevalence of atrophy and other morphological signs of the disease. Dysregeneration determines the morphogenesis and clinical and morphological picture of chronic hepatitis.
The presence of chronic inflammation can only be discussed when it is detected during a morphological study. Before the biopsy, the clinician has the right to diagnose CG and can only use the syndromological designation “non-ulcer dyspepsia”.
The endoscopic research method makes it possible to determine the diagnosis with great accuracy (or significantly reduce the number of proposed diagnoses), examine all parts of the stomach, and take biopsies for histological examination.
The possibilities of endoscopic examination are not limited only to visual examination of the gastric cavity and taking biopsies; there are a number of additional techniques used in conjunction with endoscopy (chromogastroscopy, transendoscopic pH-metry). Gastroscopy with a complete clinical and morphological examination of biopsy samples of the gastric mucosa (with determination of Hp) is considered the correct method for diagnosing various types of gastric lesions.
The most common cause (70–80%) of chronic gastritis is the bacterium Helicobacter pylori. Autoimmune gastritis is diagnosed in 15–18% of cases, about 10% are due to NSAIDs, less than 5% are reflux gastritis, 1% are rare forms of hCG.
Photo: Evgeniy Krech Medical Bulletin , October 5, 2017
Share
Stages of disease development
The disease occurs in four stages:
- Hyperemic. The gastric mucosa becomes reddish and swollen.
- Hypertrophic. There is a thickening of the mucosa with a simultaneous decrease in the production of hydrochloric acid. Changes in tissues and cells (dysplasia) and accumulation of leukocytes in the wall of the organ (metaplasia) are possible.
- Atrophic. With prolonged inflammation, the gastric mucosa becomes thinner, regeneration worsens, epithelial cells die, and are replaced by scar tissue.
- Erosive and/or ulcerative. On the inner surface of the organ, due to the thinning of the mucous membrane, lesions of varying depths form.
Symptoms
Antral gastritis is accompanied by minor complaints or manifests itself in various variants of dyspepsia - digestive disorders:
- ulcer-like dyspepsia – dull pain in the upper abdomen, heartburn;
- dyskinetic variant of gastric dyspepsia - nausea, rapid satiety, bloating after eating.
As the pathology progresses, the pain syndrome intensifies. The pain becomes cramping, aching, sucking, and can bother you on an empty stomach and at night. It is accompanied by belching, a burning sensation in the chest, often reminiscent of an angina attack.
When you feel (palpate) the abdomen, you can determine moderate pain in the upper abdominal cavity and its swelling. With a chronic course of the process, weight loss, sleep disturbances, and irritability are possible.
Treatment of the disease
In order to get rid of gastritis, the specialist prescribes:
- antibiotics whose action is aimed at Helicobacter pylori;
- antacids to neutralize hydrochloric acid and for pain relief;
- drugs to block the production of hydrochloric acid and heal the gastric mucosa.
In the case of an autoimmune process, immunosuppressants and corticosteroids can be used. In any case, the patient is recommended to give up bad habits, eat a healthy diet, and avoid stressful situations.
At the first signs of gastritis, do not wait for self-healing, make an appointment with a gastroenterologist. Ignoring the symptoms can lead to gastritis becoming chronic and causing serious consequences. Multidisciplinary medical specialists are always ready to help you.
Our clinic is equipped with the necessary medical equipment for diagnosing diseases, and our center employs experienced specialists. Timely prescribed treatment and a completed course of drug therapy will allow you to forget about the disease forever or significantly increase periods of remission.
Diet
Any disease is a reason to think about your lifestyle; superficial gastritis is no exception. Its development directly depends on what we eat and at what time we eat it, how active our lifestyle is, how we take care of our body, what bad habits we have, how calm our family and work relationships are, and whether we enjoy life in general. Of course, this disease is not a reason to eat semolina porridge and pureed soups all your life, but helping to shorten your life by overeating, drinking alcohol and smoking is, to say the least, stupid.
If you have undergone a course of treatment, then you do not have to follow a strict diet, but it is imperative to exclude foods that can lead to an exacerbation of the disease. Spices, herbs, marinades, pickles, spicy foods, carbonated drinks are best forgotten forever. Of course, this is not easy, but try to convince yourself that it is absolutely necessary, since the chain of gastritis->ulcer->oncology is not a horror story, but a completely possible path of development of the disease. try not to eat too hot or, conversely, cold food, it irritates the walls of the stomach. Avoid long breaks in eating and do not overeat.