Quick transition Treatment of gastritis
Gastritis is a general term that combines several pathological conditions characterized by inflammation and degeneration of the gastric mucosa.
The mucous membrane covers the entire surface of the stomach and plays an important role in digestion. Its glands produce gastric juice, the enzyme pepsin, hydrochloric acid, lipase, hormone-like components, mucus and bicarbonate. These substances are responsible for the breakdown of proteins and fats, protect the body from pathogenic bacteria, and activate metabolic processes.
When inflamed, the mucous membrane produces less acid, enzymes, mucus and other substances that are necessary for the proper functioning of the gastrointestinal tract. There is a risk of developing gastritis.
Gastritis can occur in acute and chronic forms. It is important to see a doctor in time to get a diagnosis and treatment, and to prevent complications.
Types of gastritis
The largest division of gastritis is acute and chronic. The first occurs immediately after irritating factors come into contact with the gastric mucosa. In case of improper nutrition, it manifests itself in a catarrhal form, in case of poisoning or infection - in a fibrinous form.
Chronic is often caused by the bacterium Helicobacter pylori. The disease is characterized by a sluggish course with periodic exacerbations. Based on the localization of the inflammatory process, the following forms are distinguished:
- antrum - in the lower part of the stomach;
- fundal - in the middle section (sometimes extends to the bottom of the organ);
- reflux gastritis - in the area of the pylorus of the stomach.
The chronic type of the disease is characterized by dysfunction of gastric secretion. Its excessive activity causes increased acidity (this form is called hyperacid). With secretory insufficiency, acidity is reduced (this form is called anacid).
How is Gastropanel performed?
Blood sampling to determine markers of atrophic gastritis is carried out in the morning on an empty stomach and 20 minutes after a protein breakfast. Blood is collected into serum tubes, which are centrifuged for analysis.
Blood serum analysis determines markers of chronic atrophic gastritis. Markers of atrophy of the mucous membrane of the fundic and antral parts of the stomach are:
- Pepsinogen I, Pepsinogen II and their ratio,
- Gastrin-17 and Gastrin-17 stimulated after a protein breakfast,
- determination of antibodies to Helicobacter pylori Ig G.
The tests are based on enzyme immunoassay technology.
Besides,
- Antibodies to parietal cells of the body of the stomach are determined in autoimmune atrophic gastritis with a high risk of disorders associated with vitamin B12 deficiency, for which the level of vitamin B12 is determined.
- Homocysteine is identified as a risk factor for vascular and thromboembolic diseases.
- To clarify Helicobacter pylori infection, an additional test of the acute phase of infection is performed, Ig A and IgM antibodies are determined.
Types of damage to the mucous membrane
Gastritis can also be classified according to the degree of change in the gastric mucosa. The mildest form is superficial, when the inflammatory process affects only the upper part of the mucosa. More dangerous forms include the following:
Although hyperplastic gastritis is characterized by the appearance of neoplasms, they are predominantly benign.
The atrophic form often leads to stomach cancer. Each of these types can be focal or diffuse: the first covers a small area of the mucous membrane (although there may be several of them), the second spreads over its entire surface.
What bad habits can cause gastritis?
The most common cause of gastritis is the habit of eating poorly and chewing food poorly. Poor nutrition should be understood as: drinking coffee and sweets on an empty stomach, non-compliance with the diet, abuse of smoked, fatty and spicy foods. Surely you have noticed that if you chew your food poorly and quickly “push it down” (seemingly full), then this is self-deception. Then, of course, there will be a feeling of discomfort in the stomach, pain, etc.
Types of gastritis by etiology
The mucous membrane of the stomach can become inflamed for various reasons. Gastroenterologists, according to this criterion, divide diseases into several groups:
There are also mixed types. Thus, AC inflammation means that reflux is caused by autoimmune factors. It happens that autoimmune effects are combined with Helicobacter pylori infection. Then we are talking about AB gastritis.
Diagnostics
In most cases, detecting gastritis is not difficult. To undergo a comprehensive examination, you must make an appointment with a gastroenterologist. The doctor will ask the patient about complaints and examine medical history. A general examination sometimes reveals external manifestations of the disease. The diagnosis is made after analyzing the results of instrumental and laboratory examinations. If acute abdominal pain occurs due to a gastrointestinal disorder, a doctor can be called to your home.
Examination methods used:
- Esophagogastroduodenoscopy is a standard examination method for suspected gastritis or gastric ulcer. The doctor asks the patient to lie on his side and open his mouth wide. The root of the tongue is treated with lidocaine, after which a flexible tube equipped with a camera and a light source is inserted into the gastrointestinal tract. During the examination, the doctor can examine the condition of the mucous membrane of the stomach and intestines by looking at the monitor. This is the most informative type of diagnosis.
- A biopsy of the gastric mucosa is the collection of a small number of organ cells for subsequent histological examination and determination of the cause of the disease. A painless biopsy is usually performed during an esophagogastroduodenoscopy.
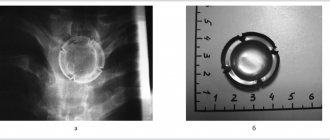
- X-ray of the organ. A contrast agent is first injected into the stomach. The resulting image helps to detect indirect signs of inflammation.
- Study of the acid-base state of the stomach contents (pH-metry). This study helps determine the type of gastritis and evaluate the effectiveness of therapeutic treatment of the disease.
- Breath test to detect bacterial gastritis. Using a special device, the concentration of carbon in exhaled air is assessed. An excess of this substance indicates Helicobacter pylori infection.
If necessary, your doctor may need additional tests, including blood tests and an ultrasound examination of the digestive system. The use of several diagnostic methods allows a specialist to prescribe more effective and safe treatment.
Causes of acute gastritis
This disease appears suddenly. In rare cases, the cause may be the bacteria Helicobacter pylori entering the body. But usually it does not make itself felt instantly, but is the causative agent of sluggish chronic gastritis.
It is usually not difficult for an adult to determine the cause. It is enough to analyze what he ate and drank several hours before the attack. Inflammation can be caused by:
Infections can also cause an attack. Among the most likely, gastroenterologists identify cytomegaloverus, syphilis, and staphylococcus infection. People with weakened immune systems are more likely to become infected. Another reason for the development of an acute inflammatory process is exposure to bile. This only applies to type C gastritis.
Does HP gastritis cause non-ulcer dyspepsia in some patients?
The answer to the question of whether HP associated gastritis causes nonulcer dyspepsia in some patients is probably “yes,” but there is no way to determine the part of them that can respond to irradiation. The available data are inconclusive, partly because nonulcer dyspepsia may represent a group of diseases with different pathogenesis. Many (including myself) agree that HP elimination should be attempted in patients with troublesome non-ulcer dyspepsia who are positive for HP after failure of antisecretory therapy. The question remains whether to confirm active infection or simply treat patients with positive serology. Future research will determine the best algorithm for diagnosing HP among biopsy, breath tests, and serology. We also need data regarding the use of radiation therapy in patients with nonulcer dyspepsia.
Causes of development of chronic gastritis
The second most important cause of chronic inflammation of the gastric mucosa (after the bacterium Helicobacter pylori) is poor nutrition. This includes not only harmful products. Violation of the eating schedule is also detrimental to the stomach. Inflammation can result from:
The influence of other diseases (endocrine, metabolic, infectious, hypoxic) cannot be excluded. External factors (harmful working conditions, stress) also become causes of gastritis.
Directions for treatment in the presence of a chronic disease
When infected with Helicobacter pylori, the only cure is eradication of the infectious agent. The functions performed include preventing the spread of infection, preventing the possibility of bacteria becoming unsusceptible to antibiotics, reducing the duration of the course of therapy and the number of drugs and the risk of side symptoms.
Antibiotics like tetracyclines and penicillins and medications based on metronidazole, proton pump inhibitors, bismuth agents, and the like are used as tools that prevent the spread of bacteria or the exacerbation of chronic moderately atrophic gastritis
General signs of gastritis
Regardless of the type (acute or chronic), it always manifests itself as pain in the epigastric region (only its nature differs). Pain appears after eating or, conversely, from hunger. Other symptoms from the digestive system are possible:
Symptoms in adults are more severe than in children. In children, attacks are often accompanied by weakness, fever, and bruises under the eyes. Parents may confuse the first signs of gastritis with poisoning.
Another noticeable symptom of many types of this disease is a white (less often yellow) coating on the tongue. It is not cleaned during normal hygiene procedures. In most cases, plaque indicates a decrease in acidity.
Other connections and other types of non-erosive gastritis
Pernicytic anemia.
Pernicytosis anemia occurs as a result of severe atrophic gastritis of the acid-producing mucosa with achlorhydria, which impairs the secretion of intrinsic factor, and subsequent malabsorption of vitamin B12.
Most patients have minimal or no associated antral gastritis and therefore have high plasma gastrin levels because gastrin is secreted in response to achlorhydria. In fact, when gastroscopy is performed for unexplained hypergastrinemia, severe atrophic gastritis is the main finding. Many patients with severe atrophic gastritis and achlorhydria still have normal or near-normal levels of vitamin B12 absorption. They are likely to develop vitamin B12 malabsorption over time. An endoscopic biopsy is performed when a diagnosis of severe atrophic gastritis is suspected. If the Schilling
is used to make the diagnosis of pernicytous anemia, endoscopic examination should still be performed to identify the presence of any polypoid lesions, which sometimes occur in severe atrophic gastritis (gastric carcinoid and, less commonly, gastric adenomas or adenocarcinoma).
Reactive gastropathy. The definition of reactive gastropathy was given above. In addition to the fact that reactive gastropathy is a common finding in areas adjacent to the edges of ulcers and erosions, it is also found around anastomoses (stomies) after gastrectomy. With stomal reactive gastropathy, vascular congestion is also usually present.
Lymphocytic gastritis.
Lymphocytic gastritis is a recently recognized histological type characterized by massive lymphocytic infiltration of epithelial cells that is not necessarily present in the lamina propria below the epithelium. Lymphocytic gastritis is not a variant of HP gastritis. Currently, it is of interest because... it is a “new” pathway of injury and also due to associated conditions. Associated conditions include virtually all cases of diffuse pox-like gastritis (rare in North America), some cases of celiac disease, and some cases of Ménétrier's disease. Lymphocytic gastritis can also be found on biopsy in patients without visible pathology.
Specific types of gastritis.
Specific gastritis is associated with more specific histological (and sometimes obvious endoscopic) features that can provide a basis for diagnosis (eg, cytomegalovirus) or, if not, can significantly narrow the differential diagnosis, which is of great therapeutic or prognostic value. Specific types of gastritis are rare. Infectious types are most important, especially in immunocompromised patients in whom cytomegalovirus infection is common. In addition to infectious gastritis, other specific gastritis include lesions limited to the stomach, such as Menetrie
,
gastrointestinal disorders that also involve other parts of the intestine, such as Crohn's disease, and finally, systemic diseases, such as sarcoidosis.
How to treat the disease
Since there are many types of gastritis, and each of them has its own causes, you cannot limit yourself to one treatment method. To combat each provoking factor, appropriate drugs are needed.
The doctor must determine by characteristic signs whether the patient’s acidity is increased or decreased. Depending on this, a suitable treatment regimen is selected.
Treatment of gastritis is usually complex, it is carried out in the following areas:
If the bacterium Helicobacter pylori is detected, it is important to eradicate it (complete destruction) with antibiotics. This is necessary to eliminate ulcerations, accelerate their healing and prevent the development of peptic ulcers and stomach cancer.
Advantages of Gastropanel for diagnosing “atrophic gastritis”
Thus, Gastropanel allows you to answer the following questions:
- does the patient have atrophic gastritis, in which part of the stomach are the changes localized,
- assess the risk of developing stomach cancer and peptic ulcers,
- does the patient suffer from gastritis caused by Helicobacter pylori,
- identify autoimmune gastritis or atrophic gastritis with damage to the body of the stomach, which may determine the risk of developing vitamin B12 deficiency, which can be associated with many diseases (atherosclerosis, vascular damage to the brain and heart, depression, polyneuropathy, dementia, etc.)
What advantages of Gastropanel can be noted: it is a simple non-invasive serological test, high sensitivity, specificity, safety and convenience for the patient, quick results, and meets the principles of evidence-based medicine.
How is acidity level determined?
The main acid found in the stomach and determining its acidity level is hydrochloric acid. It is produced by parietal cells. The alkaline components of gastric juice neutralize hydrochloric acid. They are produced by accessory cells of the mucosa. The two substances interact and the acidity level changes throughout the day.
You can find out its level using intragastric pH-metry. To do this, a thin probe with a measuring electrode is placed into the patient's stomach. It gradually moves deeper and shows the pH in different areas of the organ.
In the part of the stomach where acid is produced, in an adult patient the pH should be from 1.6 to 2.0, and in the zone of alkali production and acid quenching - up to 5.2.
The doctor also pays attention to the symptoms. With high acidity, the patient suffers from heartburn, belching and a burning sensation in the throat; with low acidity, the patient suffers from bloating, flatulence and bad breath.
What to do if you are diagnosed with atrophic gastritis
A few words about the principles of treatment of chronic atrophic gastritis. Treatment approaches are individual, it all depends on the severity of atrophic processes, the presence of Helicobacter, and vitamin B12 deficiency.
The problem will be dealt with by a doctor who will prescribe:
- treatment,
- repeated studies to monitor treatment,
- repeated consultations to assess the clinical manifestations of the disease and adjust treatment.
It is most difficult to eliminate autoimmune mechanisms of damage to the gastric mucosa; the question of prescribing hormonal drugs arises only when gastritis is accompanied by anemia. Helicobacter pylori eradication therapy has its own characteristics. First of all, the question arises about the acidity of gastric juice, and more often treatment is carried out without antisecretory drugs. The study of the acidity of gastric juice using the pH-metric method is now rarely carried out (usually daily monitoring in a hospital setting), but it is possible to orient the acidity according to the level of Pepsinogen I.
A high level of Pepsinogen and periodic heartburn in a patient may indicate preserved gastric secretion. In case of atrophic gastritis in a hypo or anacid state with damage to the body and outlet of the stomach, antisecretory drugs are excluded and Helicobacter pylori eradication is carried out with antibiotics. Effective eradication of infection improves processes in the gastric mucosa, and can be considered as a prevention of the development of gastric cancer.
Treatment of acidity disorders
If there are signs of low acidity, replacement therapy with enzyme preparations is prescribed. Its main task is to normalize the production of pepsin. Preparations containing acedin-pepsin help with this. Drug stimulation of gastric juice secretion is also necessary.
If the diagnostic results reveal increased acidity, the patient is prescribed antacids. They neutralize acid, weaken the activity of pepsin, and in some cases have an enveloping effect. To eliminate symptoms, medications are recommended that stimulate gastrointestinal motility and relieve spasms of smooth muscles. Additionally, you can use folk remedies - herbs, flax seeds, potato juice.
Folk remedies to increase stomach acidity
Low stomach acidity requires very serious attention and treatment. But often very positive results can be achieved by properly selected nutrition.
- A drink made from sea buckthorn berries is very useful.
- A very healthy and tasty habit: half an hour before meals you need to drink a few sips (50–70 grams) of honey water, for which you need to dissolve half a teaspoon of honey in warm water.
- For low stomach acidity, apricots in any form have proven themselves very well - fresh, dried (apricots, dried apricots) - and apricot juice.
- A decoction or infusion of rosehip, which is also very good to drink before meals, perfectly helps regulate low stomach acidity.
- Fresh cucumbers also slightly increase the acidity of gastric juice if they are properly chopped (the finer the better).
- Grapes are useful - it is recommended to eat up to 150 grams of fresh grapes 20 minutes before meals.
- Fresh turnip salad has long been used to increase acidity: fresh turnips must be grated and seasoned with vegetable oil (salt should be taken to taste, but not overused).
- Beans help increase and normalize the acidity of gastric juice.
- Freshly prepared carrot juice is very useful, which should be drunk shortly before meals, a quarter glass.
- With low stomach acidity, the benefits of blueberries are generally recognized, which can be used in pies, dumplings, and compotes.
- A long-term and persistent increase in the acidity of gastric juice ensures the consumption of a variety of meat foods. However, it should be remembered that for any diseases of the gastrointestinal tract, you should choose only lean meat (this could be lean pork, veal, rabbit, skinless poultry).
Also, to normalize the acidity of gastric juice, decoction and juice of plantain, calamus root, trefoil (also known as trifolium or water trefoil), gentian, marsh cudweed, lingonberry, St. John's wort, buckthorn, rhubarb, yarrow, rowan, centaury, immortelle, aloe, thyme are used and many other herbs, fruits and berries that our land is rich in.
Why are gastroprotectors needed?
To prevent complications such as peptic ulcers and malignant tumors, it is important to keep the structure of the mucous membrane intact. Gastroprotectors are used for these purposes:
They should be taken when signs of gastritis appear. The doctor will determine which medications will fit into the selected treatment package. For prevention purposes, you do not need to drink them.
The stomach contains natural gastroprotectors - prostaglandins. They stimulate the formation of mucus, improve microcirculation and protect cells from destruction. If they are not produced enough, the gastroenterologist may prescribe their synthetic analogues. If the patient is being treated with non-steroidal anti-inflammatory drugs, drugs with prostaglandins prevent ulcerative lesions of the mucous membrane.
How to eliminate constipation with gastritis
If you have gastritis, it is very important to follow these rules to prevent or eliminate constipation.
- Normalize drinking regime and diet.
A person should consume at least 1.5–2 liters of liquid per day. The diet for gastritis and constipation should be adjusted by a doctor, taking into account the form of the disease and the patient’s condition. It is important to avoid foods that can cause aggravation of pathology and constipation. For any form of gastritis, including atrophic, fatty, fried, spicy, salty foods should be excluded from the diet. You should not eat canned food, spices and smoked meats, as well as foods that cause increased gas formation and other digestive problems (pears, legumes, cabbage, radishes). It is necessary to introduce into the diet foods that help improve intestinal motility (vegetables, fruits) and have a mild laxative effect (beets, plums, apples, apricots, peaches). Eating prunes has a particularly beneficial effect on digestion. It is also recommended to include in the menu foods that are rich in fiber and promote natural cleansing of the body (bran, buckwheat porridge, oatmeal, some vegetables and fruits).
- To live an active lifestyle.
Walking in the fresh air and simple physical exercises perfectly stimulate the intestines and help eliminate constipation. This is especially true for those who have a sedentary job.
- Follow prescribed drug therapy.
The selection of medications to relieve constipation due to gastritis should only be made by a doctor. He will assess the patient’s condition and recommend a drug that is suitable for a particular case. You should not treat constipation on your own, as it can make the situation worse.
Up to contents
Preventive measures
Since gastritis is now diagnosed not only in adults, but also in children, prevention should begin as early as possible. First of all, you should normalize your diet:
When the first symptoms of inflammation of the gastric mucosa appear, it is important to minimize (or better yet eliminate) the consumption of chocolate, coffee, spicy and fried foods.
Gastroenterologists recommend regularly checking for parasitic infestations. When they are detected, it is important to carry out timely treatment, because they often attack the digestive system.
Helicobacter pylori
The discovery of HP is considered one of the most important discoveries of this century. HP is the most common cause of non-erosive gastritis and most patients with HP remain asymptomatic throughout their lives. However, about 10% develop peptic ulcers, which, along with an increased risk of relapse, makes HP a current problem. The reason for this, which is well known, is that Hp eradication in patients with peptic ulcers reduces the number of relapses so significantly that this therapy can be considered a treatment that provides a very low relapse rate. The presence of HP in patients with duodenal ulcers is greater than or equal to 95%, with gastric ulcers about 80% and in patients with NSAID drugs associated peptic ulcers about 50%. Endoscopic biopsy remains the most common technique for obtaining direct confirmation of active infection. When diagnosis is made on the basis of endoscopic biopsy in clinical practice, some endoscopists take biopathies for histology and for immersion in one of the available color urease tests. If the result of the urease color test is positive, biopaths taken for histological examination become unnecessary. This practice has not led to victory in disputes with pathologists, but is justified if the purpose of the study is simply to determine whether HP is present. If the urease color result is negative, the biopathies may be sent for histological examination to determine whether the indicator test was falsely negative. Urease breath tests, which are approved for clinical use, provide a noninvasive way to diagnose active infection. A positive serological result indicates that the infection has been present for some time, but does not necessarily indicate that the infection is currently active.
Popular questions about hypoacid gastritis
How to determine low stomach acidity?
Only pH-metry can give an accurate determination of acidity. But you can suspect its low level if you can safely eat sour lemon.
How to distinguish gastritis with high and low acidity?
There are certain signs that characterize different types of acidity. If it is heartburn or sour belching, then most likely this indicates increased acidity. Low blood pressure is characterized by belching with the smell of rotten eggs, which indicates poorly digested food.
What should you not eat if you have gastritis with low acidity?
If such gastritis is detected, it is better to forget about smoked, fatty, spicy foods, fermented cheeses, chocolate, coffee and carbonated drinks.
Symptoms and signs of the disease
The symptoms of such gastritis are associated with the severity of the disease. At the very beginning, they may not be noticeable at all. But later complaints with hypoacid gastritis are as follows:
- pain in the upper abdomen (sometimes radiating under the ribs on the left side);
- feeling of discomfort (feeling of heaviness, bloating);
- belching “rotten eggs”, metallic taste in the mouth, tongue with a gray coating;
- poor appetite;
- frequent diarrhea or constipation;
- nausea, excessive salivation;
- chronic fatigue, headaches, low performance;
- weight loss, changes in sleep patterns.
During a severe exacerbation, other signs may be added: rapid heartbeat, fainting.