Intestinal infection in children is a group of infectious diseases of various etiologies that occur with primary damage to the digestive tract, toxic reaction and dehydration of the body.
In children, intestinal infection is manifested by increased body temperature, lethargy, lack of appetite, abdominal pain, vomiting, and diarrhea. Diagnosis of intestinal infection in children is based on clinical and laboratory data (history, symptoms, excretion of the pathogen in feces, detection of specific antibodies in the blood). For intestinal infections in children, antimicrobial drugs, bacteriophages, and enterosorbents are prescribed; During the treatment period, it is important to follow a diet and rehydrate.
Intestinal infection in children is an acute bacterial and viral infectious disease accompanied by intestinal syndrome, intoxication and dehydration. In the structure of infectious morbidity in pediatrics, intestinal infections in children occupy second place after ARVI. Susceptibility to intestinal infections in children is 2.5-3 times higher than in adults. About half of the cases of intestinal infection in children occur at an early age (up to 3 years). Intestinal infection in a young child is more severe and may be accompanied by malnutrition, the development of dysbacteriosis and enzymatic deficiency, and decreased immunity. Frequent repetition of episodes of infection causes disruption of the physical and neuropsychic development of children.
Causes of intestinal infection in children
The range of pathogens causing intestinal infections in children is extremely wide. The most common pathogens are gram-negative enterobacteria (Shigella, Salmonella, Campylobacter, Escherichia, Yersinia) and opportunistic flora (Klebsiella, Clostridia, Proteus, Staphylococcus, etc.). In addition, there are intestinal infections caused by viral pathogens (rotaviruses, enteroviruses, adenoviruses), protozoa (giardia, amoebae, coccidia), and fungi. The common properties of all pathogens that cause the development of clinical manifestations are enteropathogenicity and the ability to synthesize endo- and exotoxins.
Infection of children with intestinal infections occurs through the fecal-oral mechanism through nutritional (through food), water, contact and household routes (through dishes, dirty hands, toys, household items, etc.). In weakened children with low immunological reactivity, endogenous infection with opportunistic bacteria is possible. The source of OKI can be a carrier, a patient with an erased or manifest form of the disease, or pets. In the development of intestinal infection in children, a major role is played by violation of the rules of preparation and storage of food, the admission into children's kitchens of persons who are carriers of the infection, patients with tonsillitis, furunculosis, streptoderma, etc.
Sporadic cases of intestinal infection in children are most often recorded, although group and even epidemic outbreaks are possible with food or waterborne infection. The increase in the incidence of some intestinal infections in children has a seasonal dependence: for example, dysentery occurs more often in summer and autumn, rotavirus infection - in winter.
The prevalence of intestinal infections among children is due to epidemiological characteristics (high prevalence and contagiousness of pathogens, their high resistance to environmental factors), anatomical and physiological characteristics of the child’s digestive system (low acidity of gastric juice), and imperfect defense mechanisms (low concentration of IgA). The incidence of acute intestinal infection in children is facilitated by disruption of the normal intestinal microbiota, non-compliance with personal hygiene rules, and poor sanitary and hygienic living conditions.
Description of the disease
Intestinal infection refers to diseases of the gastrointestinal tract caused by bacterial, viral or fungal agents.
The most common pathogens are: enteroviruses, rotaviruses, salmonella, staphylococcus, dysentery bacillus, etc. Intestinal tract infections are widespread in childhood. In terms of incidence, they are second only to respiratory diseases. Infection, as a rule, occurs due to non-compliance by the child and his parents with the rules of personal hygiene, sharing toys and other household items with infected people, and eating unwashed vegetables and fruits. The disease can be identified by impaired bowel movements, nausea, vomiting, a sharp decrease in appetite and an increase in body temperature.
If you suspect that a child has an intestinal infection, you should immediately seek advice from a gastroenterologist. Lack of treatment can provoke the development of serious complications: septic condition, shock due to vascular paralysis due to bacterial intoxication, acute kidney failure, heart failure, etc.
Classification of intestinal infection in children
According to the clinical and etiological principle, among the intestinal infections most often recorded in the pediatric population, there are shigellosis (dysentery), salmonellosis, coli infection (escherichiosis), yersiniosis, campylobacteriosis, cryptosporidiosis, rotavirus infection, staphylococcal intestinal infection, etc.
According to the severity and characteristics of symptoms, the course of intestinal infection in children can be typical (mild, moderate, severe) and atypical (erased, hypertoxic). The severity of the clinic is assessed by the degree of damage to the gastrointestinal tract, dehydration and intoxication.
The nature of local manifestations of intestinal infection in children depends on the damage to one or another part of the gastrointestinal tract, and therefore gastritis, enteritis, colitis, gastroenteritis, gastroenterocolitis, enterocolitis are distinguished. In addition to localized forms, generalized forms of infection can develop in infants and weakened children with the spread of the pathogen beyond the digestive tract.
During an intestinal infection in children, acute (up to 1.5 months), protracted (over 1.5 months) and chronic (over 5-6 months) phases are distinguished.
Dysentery in children
After a short incubation period (1-7 days), the temperature rises sharply (up to 39-40° C), weakness and fatigue increase, appetite decreases, and vomiting is possible. Against the background of fever, there is a headache, chills, and sometimes delirium, convulsions, and loss of consciousness. Intestinal infection in children is accompanied by cramping abdominal pain localized in the left iliac region, symptoms of distal colitis (pain and spasm of the sigmoid colon, tenesmus with rectal prolapse), symptoms of sphincteritis. The frequency of bowel movements can vary from 4-6 to 15-20 times per day. With dysentery, the stool is liquid, containing impurities of cloudy mucus and blood. In severe forms of dysentery, hemorrhagic syndrome may develop, including intestinal bleeding.
In young children with intestinal infection, general intoxication prevails over colitis syndrome; disturbances in hemodynamics, electrolyte and protein metabolism occur more often. The most common intestinal infection in children is caused by Shigella Zona; heavier - Shigella Flexner and Grigoriez-Shig.
Salmonellosis in children
Most often (in 90% of cases) the gastrointestinal form of salmonellosis develops, occurring as gastritis, gastroenteritis, gastroenterocolitis. Characterized by subacute onset, febrile fever, adynamia, vomiting, hepatosplenomegaly. Stool with salmonellosis is liquid, copious, fecal, the color of “swamp mud”, with admixtures of mucus and blood. Typically, this form of intestinal infection ends in recovery, but in infants it can be fatal due to severe intestinal toxicosis.
Influenza-like (respiratory) form of intestinal infection occurs in 4-5% of children. In this form, Salmonella is detected in cultured material from the throat. Its course is characterized by febrile temperature, headache, arthralgia and myalgia, symptoms of rhinitis, pharyngitis, conjunctivitis. From the cardiovascular system, tachycardia and arterial hypotension are noted.
The typhus-like form of salmonellosis in children accounts for 2% of clinical cases. It occurs with a long period of fever (up to 3-4 weeks), severe intoxication, and dysfunction of the cardiovascular system (tachycardia, bradycardia).
The septic form of intestinal infection usually develops in children in the first months of life who have an unfavorable premorbid background. It accounts for about 2-3% of cases of salmonellosis in children. The disease is extremely severe, accompanied by septicemia or septicopyemia, disruption of all types of metabolism, and the development of severe complications (pneumonia, parenchymal hepatitis, otoanthritis, meningitis, osteomyelitis).
Escherichiosis in children
This group of intestinal infections in children is extremely extensive and includes coli infections caused by enteropathogenic, enterotoxigenic, enteroinvasive, and enterohemorrhagic Escherichia.
Intestinal infection in children caused by Escherichia, occurs with low-grade or febrile temperature, weakness, lethargy, decreased appetite, persistent vomiting or regurgitation, flatulence. Characterized by watery diarrhea (copious, splashing yellow stool mixed with mucus), quickly leading to dehydration and the development of exicosis. In Escherichiosis, caused by enterohemorrhagic Escherichia, the diarrhea is bloody.
Due to dehydration, the child develops dry skin and mucous membranes, tissue turgor and elasticity decreases, the large fontanel and eyeballs sink, and diuresis decreases such as oliguria or anuria.
Rotavirus infection in children
It usually occurs as acute gastroenteritis or enteritis. The incubation period lasts on average 1-3 days. All symptoms of intestinal infection in children develop within one day, while damage to the gastrointestinal tract is combined with catarrhal symptoms.
Respiratory syndrome is characterized by hyperemia of the pharynx, rhinitis, sore throat, and coughing. Simultaneously with damage to the nasopharynx, signs of gastroenteritis develop: loose (watery, foamy) stools with a frequency of bowel movements from 4-5 to 15 times a day, vomiting, temperature reaction, general intoxication. The duration of intestinal infection in children is 4-7 days.
Staphylococcal intestinal infection in children
A distinction is made between primary staphylococcal intestinal infection in children, associated with eating food contaminated with staphylococcus, and secondary, caused by the spread of the pathogen from other foci.
The course of intestinal infection in children is characterized by severe exicosis and toxicosis, vomiting, and increased bowel movements up to 10-15 times a day. The stool is liquid, watery, greenish in color, with a small admixture of mucus. With secondary staphylococcal infection in children, intestinal symptoms develop against the background of a leading disease: purulent otitis media, pneumonia, staphyloderma, tonsillitis, etc. In this case, the disease can take a long wave-like course.
Clostridiosis
Severe clostridiosis can occur in three clinical variants: 1. with the manifestation of severe toxicosis and anaerobic sepsis; 2. cholera-like form; 3. with the development of necrotic enteritis, sometimes complicated by intestinal perforation and peritonitis.
Intestinal infections caused by Escherichia and rotasirus occur with secretory diarrhea syndrome. Secretory diarrhea has its own clinical features that allow it to be differentiated from other diseases of the gastrointestinal tract.
Diagnosis of intestinal infection in children
Based on an examination, epidemiological and clinical data, a pediatrician (pediatric infectious disease specialist) can only assume the likelihood of an intestinal infection in children, however, an etiological deciphering is possible only on the basis of laboratory data.
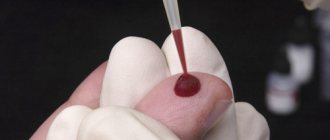
The main role in confirming the diagnosis of intestinal infection in children is played by bacteriological examination of stool, which should be carried out as early as possible, before the start of etiotropic therapy. In case of a generalized form of intestinal infection in children, blood cultures are performed for sterility, bacteriological examination of urine and cerebrospinal fluid.
Serological methods (RPGA, ELISA, RSK), which make it possible to detect the presence of antibodies to the pathogen in the patient’s blood from the 5th day from the onset of the disease, are of certain diagnostic value. The study of the coprogram allows us to clarify the localization of the process in the gastrointestinal tract.
In case of intestinal infection in children, it is necessary to exclude acute appendicitis, pancreatitis, lactase deficiency, biliary dyskinesia and other pathologies. For this purpose, consultations are held with a pediatric surgeon and a pediatric gastroenterologist.
Symptoms
The first signs of rotavirus can appear within 24 hours after infection, but more often they appear 3-5 days after the virus enters the body. The symptoms of the disease are acute and obvious: the temperature rises sharply and strongly (up to 38-390); vomiting occurs several times a day (up to 3-6); the general condition of the child is lethargic, apathetic; frequent watery diarrhea begins with a pronounced light yellow tint and an unpleasant sour odor; redness of the mucous membranes of the eyes and throat occurs. Along with the manifestations of the disease described when rotavirus occurs, in the case of enterovirus infection the following may be observed: fever, convulsions, muscle and head pain. Signs of a bacterial infection are similar to the manifestations of a viral infection - these are the same elevated temperature, but up to 37-380C, vomiting (with viral infections it is always present, and with bacterial infections - in half the cases), diarrhea (if watery yellow diarrhea is observed with viral infections, sometimes with foam, then with a bacterial infection it necessarily contains inclusions of mucus, has a greenish tint, sometimes small blood clots are found in the stool - in an advanced form.
Treatment of intestinal infection in children
Complex treatment of intestinal infections in children involves the organization of therapeutic nutrition; carrying out oral rehydration, etiotropic, pathogenetic and symptomatic therapy.
The diet of children with intestinal infection requires a decrease in the volume of food, an increase in the frequency of feedings, the use of mixtures enriched with protective factors, and the use of pureed, easily digestible food. An important component of the treatment of intestinal infections in children is oral rehydration with glucose-saline solutions and drinking plenty of fluids. It is carried out until fluid loss stops. If oral nutrition and fluid intake are impossible, infusion therapy is prescribed: solutions of glucose, Ringer, albumin, etc. are administered intravenously.
Etiotropic therapy of intestinal infections in children is carried out with antibiotics and intestinal antiseptics (kanamycin, gentamicin, polymyxin, furazolidone, nalidixic acid), enterosorbents. The use of specific bacteriophages and lactoglobulins (salmonella, dysentery, coliproteus, klebsiella, etc.), as well as immunoglobulins (antirotavirus, etc.) is indicated. Pathogenetic therapy involves the administration of enzymes and antihistamines; Symptomatic treatment includes taking antipyretics and antispasmodics. During the period of convalescence, it is necessary to correct dysbiosis, take vitamins and adaptogens.
Diagnostics
Bacteriological cultures of stool and, in some cases, vomit. This is the leading diagnostic method. Determines which microbe is causing the intestinal infection. To analyze the stool, a smear is taken from the child’s anus (it is also called a “VD smear” or “intestinal group smear”). The resulting material is sown on special nutrient media. After a few days (usually 5-7 days), colonies of bacteria grow, which can be examined under a microscope and tested using various methods. Unfortunately, it is not always possible to detect the pathogen. Blood tests to determine the increase in antibody titer to any pathogen. Determine the reaction of the immune system to a suspected infection. If there is an increase in antibodies to a specific pathogen, then we can say with confidence that the person is sick (or has been sick). This method is rarely used in practice. Express diagnostics: enzyme-linked immunosorbent assay (ELISA) and other laboratory tests. They are mainly used in hospital settings. Scatological analysis of stool. In it you can see the degree of digestion of food, blood, mucus and protozoa (amoeba and lamblia).
Forecast and prevention of intestinal infection in children
Early detection and adequate therapy ensure full recovery of children after an intestinal infection. Immunity after ACI is unstable. In severe forms of intestinal infection in children, the development of hypovolemic shock, disseminated intravascular coagulation syndrome, pulmonary edema, acute renal failure, acute heart failure, and infectious-toxic shock is possible.
The basis for the prevention of intestinal infections in children is compliance with sanitary and hygienic standards: proper storage and heat treatment of products, protecting water from contamination, isolating patients, disinfecting toys and utensils in children's institutions, instilling personal hygiene skills in children. When caring for an infant, a mother should not neglect treating the mammary glands before feeding, treating nipples and bottles, washing hands after swaddling and washing the baby.
Children who have been in contact with a patient with an intestinal infection are subject to bacteriological examination and observation for 7 days.
Escherichiosis caused by EPC
Most diseases are caused by 4 serotypes: O18, O111, O55, O26. Mostly infants who are bottle-fed are affected.
Seasonality: winter-spring. Routes of infection: household contact (often hospital-acquired) and food. An endogenous pathway for the development of diarrhea is possible, as evidenced by the frequency of carriage of Escherichia in healthy individuals and the frequent appearance of pathological stools during intercurrent diseases, for example, acute respiratory diseases (ARI). Depending on the route of infection and the age of the children, the disease can occur in three clinical variants.
The first is the “cholera-like variant” of the course of the disease, which is most typical for children in the first year of life. The disease has a gradual onset with the appearance of symptoms: vomiting, diarrhea and the addition of other symptoms of the disease in the next 3-5 days.
The body temperature in most patients is normal or subfebrile, hyperthermia is almost not observed. Vomiting (regurgitation) is the most constant symptom, which appears from the first day of illness and is persistent and long-lasting. The stool is watery, spattering, yellow-orange in color, with a moderate amount of mucus mixed with feces. Its frequency increases and reaches a maximum on the 5-7th day of illness. Cramping abdominal pain is rarely observed.
In terms of the frequency of severe forms of the disease in infants, escherichiosis of the enteropathogenic group ranks third after yersiniosis and salmonellosis (S. thyphimurium). The most severe diseases are those caused by EPEC O55 and O111. The severity of the condition in patients is not due to symptoms of intoxication, but to severe disturbances of water-mineral metabolism and the development of echsicosis of II and III degrees. In some cases, hypovolemic shock is observed; decreased body temperature, cold extremities, acrocyanosis, toxic shortness of breath, darkened consciousness, tachycardia, changes in acid-base state (ABS). The mucous membranes are dry and bright, the skin fold does not straighten out, the large fontanelle sinks. Oligoanuria may develop. Thus, the “cholera-like” form of EPE in young children has specific symptoms and in most cases does not present difficulties in differential diagnosis: gradual onset, watery diarrhea, persistent infrequent vomiting, moderate fever, exicosis in the absence of pronounced symptoms of intoxication.
The second variant of the course of escherichiosis of the EPE group, which occurs in 30% of patients, is mild enteritis that occurs against the background of acute respiratory infections in young children. In this case, one can think about secondary endogenous infection with Escherichia when the body’s immunoreactivity is weakened due to the underlying disease.
The third clinical variant of the disease is foodborne toxic infection (PTI). Its development is caused by the food route of infection, which is typical for children over 1 year of age. This syndrome is characterized by vomiting and watery diarrhea. However, there are also differences from toxic infections of other etiologies (dysenteric, salmonellosis, staphylococcal): 1. in most children, a subacute and gradual onset with the development of all symptoms by the 3-4th day of the disease; 2. predominantly mild course of the disease; 3. absence of symptoms of intoxication, the severity of the disease is determined by the phenomena of exicosis.
Escherichiosis caused by ETC
Despite the diversity of pathogens in this group, most diseases are caused by five of them: O8, O6, O9, O75 and O20. Escherichiosis of this group is widespread among children of all age groups and is the etiological factor of every third laboratory-deciphered gastroenteritis or enteritis. This group of diseases is characterized by a predominantly summer seasonality (July-August).
However, in the clinical course of the disease there is a great similarity with escherichiosis caused by EPKP. In children of the 1st year of life, diseases of the ETE group occur in the form of “cholera-like” diarrhea, and in children over 1 year of age - of the PTI type, which is associated with the action of a “cholera-like” heat-labile enterotoxin, which is found with equal frequency in both groups of Escherichia .