Over the past few decades, the incidence of diseases of the gastrointestinal tract has increased significantly. Stomach pathologies make up a significant part of these alarming statistics. Unfortunately, a number of stomach diseases (some types of ulcerative processes, polyps, and other neoplasms) do not respond to conservative treatment, and then doctors sometimes resort to the only way to save the life and health of the patient - surgical intervention.
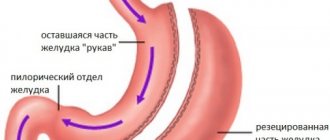
An operation to remove the stomach or part of it is called resection and its purpose is to restore the process of food passage and improve the functioning of the digestive organs. Gastric resection is also used as a treatment for severe forms of obesity. This is a complex and traumatic surgical procedure, the recovery period after which lasts from several months to a year. The patient’s condition and the overall outcome of the disease will depend on how successful the rehabilitation after surgical treatment is. Diet plays a significant role in the recovery process after gastrectomy. The diet after such an operation is quite strict and in order for everything to be successful, you must strictly follow the doctor’s recommendations. Diet plays a significant and hardly dominant role in the recovery process after gastrectomy. The diet after such an operation is quite strict and in order for everything to be successful, you must strictly follow the doctor’s recommendations. Only a qualified specialist will be able to develop an individual nutrition plan taking into account the severity of the disease, the patient’s condition, and the characteristics of his body.
What is a perforated gastric ulcer?
A perforated stomach ulcer belongs to the category of severe, life-threatening diseases. A perforation occurs in the wall of the organ and the contents flow directly into the abdominal cavity. As a result, peritonitis develops, which requires immediate surgical intervention.
Currently, in Russia, perforated ulcers have been diagnosed in almost 3 million people. Relapses occur in 6% of patients. Men are more often affected by the disease. The hormone estrogen produced by the female body has a restraining effect on the activity of the secretory glands of the gastric mucosa.
Medical care for perforation
The patient spends the acute stage with a complication in the form of perforation in a hospital setting. If the operation is not performed in time, perforation is fraught with peritonitis and death. When the surgeon confirms the diagnosis, the patient is immediately prepared for surgery.
There are three types of surgical intervention:
- suturing;
- excision followed by pyloroplasty and vagotomy;
- laser cauterization;
- resection.
A separate point is that laser cauterization is often used as a preventive measure when there is a threat of perforation. In rare cases, a laser is used for perforation. After cauterization of a stomach ulcer, patients begin to eat well earlier than after surgical procedures, but they can only eat what is indicated in the therapeutic diet.
In the postoperative period, antiulcer drug therapy is carried out. After excision of a perforated gastric ulcer, the patient is shown special dietary nutrition according to the varieties of the zero and first tables. In addition, doctors recommend taking a course of physical therapy. After the operation, the patient must remain in bed for at least the first two weeks, semi-bed rest for another month.
Causes of perforated stomach ulcer
People suffering from chronic peptic ulcer disease, as well as those who have suffered an acute form of the disease, are at risk of developing a perforation defect.
Perforation can be initiated by:
- Inflammation that occurs around the main focus of mucosal damage;
- Overeating (the stomach cannot cope with a large amount of food);
- Increased acidity of gastric juice (leads to an aggressive environment);
- Excessive consumption of foods seasoned with spices and alcohol;
- Sudden physical exertion;
Modern research indicates that the causative agent of peptic ulcer disease is the bacterium Helicobacter pylori (which has initially aggressive strains). Almost 50% of all humanity is infected with it. But contamination is not the only cause of peptic ulcer disease. Any violation of the body’s protective functions activates the pathogenic influence of microorganisms.
Factors that increase the risk of peptic ulcer disease:
- Suppressed immune system;
- Impaired quality or duration of sleep, night shift work;
- Prolonged stress;
- Taking certain medications. Long-term treatment with non-steroidal anti-inflammatory drugs (including aspirin) is not allowed; even short-term anticoagulants (warfarin, heparin), corticosteroids (prednisolone), and some chemotherapy drugs can have a pathogenic effect;
- Smoking (has an indirect effect on increasing the content of hydrochloric acid and disrupting microcirculation in the mucous membranes);
- Excessive alcohol consumption (leads to direct damage to the mucous membranes);
- Violation of food intake and nutritional quality. Too low or high temperature of food, foods with high fat content, smoked foods, etc., dry food unnecessarily load the stomach and provoke the occurrence of diseases;
- Hereditary factors;
- The presence of other pathologies of the gastrointestinal tract (for example, gastritis);
General nutrition rules
The main principle of a postoperative strict diet is to eat easily digestible foods that do not irritate the gastric mucosa and do not allow the gastrointestinal tract to work intensively.
Dishes are pureed, homogeneous, with all components thoroughly chopped. Large pieces that could cause complications should not be allowed into the stomach. You need to eat at the same time, in fractions, every 2 hours, which allows gastric juice to be produced at the right time. From the first day of eating regular food, you need to monitor the amount of food consumed.
At one time you can eat no more than 50 grams of pureed food from light, digestible foods. Gradually, the daily amount of food increases and by the 6th postoperative day it reaches 200 grams. Do not overload your stomach by eating at night. At least two hours before going to bed, you should have your last meal of light, quickly digestible foods.
One of the important rules of nutrition in the postoperative period is to eat sufficiently high-calorie food in small portions. Carbohydrates and fiber should enter the body in small quantities, and relapses can be prevented with the help of low-fat milk and herbal decoctions. The diet is followed for a very long time, and some foods must be excluded from the diet of an ulcer patient forever.
Attention: only the attending physician can prescribe a specific diet, taking into account the nature of the disease and the type of surgery performed, and the patient’s condition. After discharge from the hospital, he will be given dietary advice at home.
Early postoperative period
To restore normal functioning of the digestive system in the early postoperative period, many foods are prohibited for the patient. At this stage you can use:
- omelette;
- unsaturated broth;
- porridge;
- soups.
Dishes are steamed (omelettes), porridges are boiled until liquid, soups are prepared from dietary meat without fat. After a few days, the diet is expanded by adding vegetable purees, fish souffles and steamed meat and soft products (cutlets, meatballs, zrazy) to the menu. Subsequently, the diet is expanded by adding low-fat cottage cheese and milk, non-sour kefir, and white bread croutons.
Vegetable puree is prepared from pumpkin or zucchini with carrots, potatoes or beets, porridge is prepared from oatmeal, buckwheat, and rice. For meat products they use turkey, chicken, rabbit, and a little later - lean beef or veal. Mashed potatoes and porridge can be seasoned with natural butter in a small amount. The menu expands as the patient’s body recovers.
Late postoperative period
Gradually, over one and a half to two months after the operation, a transition is made from ground, crushed food to ordinary products that are on the permitted list. The late recovery period lasts about a year, and if the prognosis is favorable and there are no relapses, the diet can be expanded afterward.
Now you can add not too fatty cheese and raw fruits - bananas and apples - to your food. But, still, raw fruits can be eaten no more than two or three fruits per week. It is better to prepare various dishes from fruits using heat treatment.
Raw vegetables are also introduced into the diet, from which you can make salads with fresh herbs and sunflower oil. You should not eat cabbage of any kind raw. Only a few months after the operation can the patient cook borscht or cabbage soup with fresh cabbage in meat broth no more than once a week. The menu is enriched with unsweetened cookies, different types of bread, low-fat sour cream, but not for daily use.
Attention: the late postoperative period is dangerous because the acute symptoms of a peptic ulcer cease to bother you and the person can draw conclusions about a complete recovery. But, for complete restoration of the gastric mucosa it will take a lot of time, during which it is necessary to adhere to a strict diet
Symptoms of a perforated stomach ulcer
The typical form of the disease is accompanied by the entry of stomach contents into the free abdominal area.
There are three periods of development:
- Period of chemical peritonitis. The duration of the course is from 3 to 6 hours. Depends on the diameter of the hole and the volume of secretions from the stomach. Accompanied by acute pain in the stomach. Severe pain is possible in the peri-umbilical segment and in the right hypochondrium. Subsequently, they cover the entire abdomen. Perforation of the anterior wall of the stomach can manifest itself in pain in the area of the left side of the abdomen and left forearm. Painful sensations are characterized by the duration of manifestation. Vomiting occurs rarely. Blood pressure is reduced, but pulse is usually within normal limits. Breathing becomes shallow and rapid. The skin turns pale and sweating increases. The muscles of the front part of the abdomen are tense, and there is an accumulation of gases in the abdominal cavity.
- The period of bacterial peritonitis. It begins 6 hours after perforation. The abdominal muscles relax, breathing becomes deeper and sharp pain disappears. The person feels relieved. During this phase, there is an increase in temperature, an increase in heart rate and a further change in blood pressure. A period of increasing toxicity begins, which leads to an increase in the volume of gases and paralysis of peristalsis. The tongue becomes dry, with a gray coating on the front and side surfaces. The patient's general behavior changes. He experiences euphoria and relief, becomes uncritical of his condition, and does not want to be disturbed. If emergency medical care is not provided during the period of increased intoxication, then the person moves to the third, most severe stage of the disease.
- Period of acute intoxication. It begins, as a rule, after 12 hours from the moment of illness. The main manifestation is uncontrollable vomiting, leading to dehydration. Visually you can notice changes in the skin. They become dry. There is a sharp change in body temperature. An increase to 38°-40° is replaced by a decrease to 36.6°. The pulse reaches 120 beats per minute. Upper blood pressure drops to 100 mmHg. The general condition of the patient is characterized by lethargy, indifference, and a slow reaction to external stimuli. The abdomen becomes enlarged due to the accumulation of free gas and liquid. The process of urination is disrupted and eventually stops completely. If a person has reached this phase of the development of peritonitis, then it is almost impossible to save his life.
Fully or partially limited products
- Dishes that irritate the mucous membrane and stimulate secretion are excluded: strong meat/fish broths, fried and stewed dishes, mushrooms, pickles and pickled vegetables, hot and sour sauces, smoked meat and fish products, canned food, spices and seasonings;
- Fermented milk products with high acidity.
- Rye bread, puff pastry and pastry products.
- White cabbage, radish, sorrel, tomatoes, cucumbers, onions.
- Millet, barley, corn and pearl barley cereals, legumes, pasta.
- Sour fruits/berries.
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
| vegetables | 2,5 | 0,3 | 7,0 | 35 |
| vegetables legumes | 9,1 | 1,6 | 27,0 | 168 |
| swede | 1,2 | 0,1 | 7,7 | 37 |
| cabbage | 1,8 | 0,1 | 4,7 | 27 |
| green onion | 1,3 | 0,0 | 4,6 | 19 |
| bulb onions | 1,4 | 0,0 | 10,4 | 41 |
| white radish | 1,4 | 0,0 | 4,1 | 21 |
| horseradish | 3,2 | 0,4 | 10,5 | 56 |
| spinach | 2,9 | 0,3 | 2,0 | 22 |
| sorrel | 1,5 | 0,3 | 2,9 | 19 |
| mushrooms | 3,5 | 2,0 | 2,5 | 30 |
| corn grits | 8,3 | 1,2 | 75,0 | 337 |
| pearl barley | 9,3 | 1,1 | 73,7 | 320 |
| millet cereal | 11,5 | 3,3 | 69,3 | 348 |
| barley grits | 10,4 | 1,3 | 66,3 | 324 |
| pasta | 10,4 | 1,1 | 69,7 | 337 |
| bagels | 16,0 | 1,0 | 70,0 | 336 |
| wheat bread | 8,1 | 1,0 | 48,8 | 242 |
| jam | 0,3 | 0,2 | 63,0 | 263 |
| candies | 4,3 | 19,8 | 67,5 | 453 |
| pastry cream | 0,2 | 26,0 | 16,5 | 300 |
| ice cream | 3,7 | 6,9 | 22,1 | 189 |
| cake | 4,4 | 23,4 | 45,2 | 407 |
| chocolate | 5,4 | 35,3 | 56,5 | 544 |
| mustard | 5,7 | 6,4 | 22,0 | 162 |
| ginger | 1,8 | 0,8 | 15,8 | 80 |
| ketchup | 1,8 | 1,0 | 22,2 | 93 |
| mayonnaise | 2,4 | 67,0 | 3,9 | 627 |
| ground black pepper | 10,4 | 3,3 | 38,7 | 251 |
| chilli | 2,0 | 0,2 | 9,5 | 40 |
| sour cream | 2,8 | 20,0 | 3,2 | 206 |
| pork | 16,0 | 21,6 | 0,0 | 259 |
| salo | 2,4 | 89,0 | 0,0 | 797 |
| dry-cured sausage | 24,1 | 38,3 | 1,0 | 455 |
| sausages | 12,3 | 25,3 | 0,0 | 277 |
| smoked chicken | 27,5 | 8,2 | 0,0 | 184 |
| duck | 16,5 | 61,2 | 0,0 | 346 |
| smoked duck | 19,0 | 28,4 | 0,0 | 337 |
| goose | 16,1 | 33,3 | 0,0 | 364 |
| dried fish | 17,5 | 4,6 | 0,0 | 139 |
| smoked fish | 26,8 | 9,9 | 0,0 | 196 |
| canned fish | 17,5 | 2,0 | 0,0 | 88 |
| creamy margarine | 0,5 | 82,0 | 0,0 | 745 |
| animal fat | 0,0 | 99,7 | 0,0 | 897 |
| cooking fat | 0,0 | 99,7 | 0,0 | 897 |
| white dessert wine 16% | 0,5 | 0,0 | 16,0 | 153 |
| vodka | 0,0 | 0,0 | 0,1 | 235 |
| cognac | 0,0 | 0,0 | 0,1 | 239 |
| beer | 0,3 | 0,0 | 4,6 | 42 |
| cola | 0,0 | 0,0 | 10,4 | 42 |
| sprite | 0,1 | 0,0 | 7,0 | 29 |
| tonic | 0,0 | 0,0 | 8,3 | 34 |
| black tea | 20,0 | 5,1 | 6,9 | 152 |
| energy drink | 0,0 | 0,0 | 11,3 | 45 |
| * data is per 100 g of product |
Classification of perforated ulcers
- According to the clinical course of the disease:
- Typical form. Characterized by the leakage of stomach contents into the abdominal cavity;
- Atypical form. The contents enter the omentum or omental bursa, possibly leaking into the retroperitoneal tissue or intercommissural area;
- Perforation with bleeding into the abdominal cavity or gastrointestinal tract;
- According to the stages of development of peritonitis:
- Stage of primary pain shock;
- The stage of development of bacterial peritonitis, accompanied by contamination with microorganisms;
- The stage of the inflammatory process, accompanied by feelings of imaginary well-being;
- The stage of severe disease, accompanied by the occurrence of purulent peritonitis;
- According to pathological and anatomical characteristics:
- Perforation of a chronic ulcer (complication of peptic ulcer);
- Perforation of an acute ulcer;
- Perforation when the wall of a hollow organ is damaged by a tumor formation;
- Perforation due to parasitic diseases;
- The occurrence of a defect due to a violation of local blood circulation;
- According to the location of the outbreak:
- Gastric ulcer (anterior, posterior wall, lesser or greater curvature);
- Duodenal ulcer;
- Pyloroduodenal ulcer;
- Combined ulcer (stomach and duodenum);
Postoperative menu
After about five days from the date of surgery, the patient is allowed to drink a small amount of drinks, which not only do not provoke activation of the digestive organs, but also help restore the body’s immune defense.
Among the most useful drinks are, for example, a weak decoction of rose hips, the taste of which can be somewhat improved by adding a small amount of honey, as well as jelly made from sweet berries and fruits. Kissel effectively envelops the walls of the stomach, eliminating negative influences from the outside; you should drink it not only immediately after breaking fast, but also in the following days.
During the postoperative period, you are allowed to drink rosehip decoction.
Five days after starting a drinking diet after a perforated stomach ulcer and surgery, you can gradually introduce into the patient’s diet some types of dietary dishes that are balanced in chemical composition and help restore the digestive function of the body. Among these are:
- soup made from grated vegetables, which contain a minimal amount of fiber;
- viscous rice porridge, which is recommended to be prepared from pre-ground cereals;
- vegetable puree;
- steam omelets made from egg whites;
- cutlets or meat soufflé, prepared using a double boiler.
The patient's diet, of course, is very meager. But including exactly these products in the menu allows you to normalize the functioning of the affected stomach, restore tissue and prevent possible relapses.
Vegetables can be consumed in pureed form
Methods for diagnosing perforated ulcers
Perforation is characterized by an attack of sharp, sudden pain. If there is a history of peptic ulcer, gastritis, etc., then the task becomes easier. As a rule, a differential method is used for diagnosis.
It consists of examining the body, taking into account the presence/absence of the following pathologies:
- Acute appendicitis;
- Acute cholecystitis;
- Perforation of tumor formations;
- Hepatic colic;
- Acute pancreatitis;
- Thrombosis;
- Dissecting abdominal aortic aneurysm;
- Myocardial infarction;
- Lower lobe pneumonia;
- Pleurisy;
- Pneumothorax;
Additional research methods are:
- X-ray. The efficiency of diagnosing air filling of the abdominal cavity reaches 80%. But a similar picture can also be observed in the case of airy intestines or atony of the fallopian tubes;
- Electrogastroenterographic. Allows for a qualitative analysis of the evacuation function of the stomach and duodenum;
- Endoscopy. Used when X-ray results are negative, but perforation is suspected. Allows you to determine the presence of a peptic ulcer and the localization of the lesion. The study is carried out using air pumping, which helps determine the true clinical picture;
- Complete blood count (shows an increased level of leukocytes);
- Laparoscopy. Helps in qualitative and quantitative analysis of abdominal effusion. Has contraindications for use;
Laparoscopy is not used if the patient has:
- Obesity;
- Adhesions in the abdominal area;
- Violation of the integrity of the diaphragm;
- Pathology of blood clotting;
- The presence of large hernias on the anterior wall of the peritoneal region;
- General serious condition;
How to eat
In the first few days, the patient is prohibited from eating or drinking any liquids. The body is maintained through IVs. After three days, you are allowed to drink a small amount of water in small sips. Herbal decoctions and jelly can be gradually given in small doses.
After 3–4 days, weakly concentrated soups with pureed vegetables and semi-liquid pureed porridges are introduced into the menu. After another week, you can start giving the patient vegetable purees, egg omelets, and meat soufflé. As you recover, other dishes are gradually added, taking into account the list of permitted foods.
A diet for duodenal ulcers should be balanced and contain all the microelements a person needs. The diet includes carbohydrates, in an amount of about 400 grams, as well as proteins and fats (approximately 100–130 g). The calorie content of the daily menu can vary between 2800–3200 kcal. Products must contain vitamins of groups B, C, PP, A and others necessary for human health.
https://youtube.com/watch?v=JCFs7fQ-ues
The diet after surgery for a duodenal ulcer is composed of the following products:
- unsatisfying weak vegetable soups;
- porridge of a liquid consistency, with pureed cereals;
- dried white bread, biscuits;
- soft-boiled eggs, omelet;
- milk, sour cream, low-fat cottage cheese, low-fat yogurt, one-day kefir;
- mild soft cheese;
- dietary meat (rabbit, chicken), low-fat fish;
- fine or grated pasta;
- boiled or stewed vegetables, crushed into puree;
- non-acidic fruits and berries, in the form of puree or jam.
From these products you can prepare various pates, jellies, soufflés, cream soups, marmalade and other dishes that have a soft composition. It is recommended to drink herbal infusions, jelly, fruit drinks, compotes.
When preparing dishes from berries, you need to use soft fruits, without seeds or hard skin. Berries such as strawberries, raspberries, currants, etc. are not recommended.
Treatment of perforated gastric ulcer
Perforated ulcers are treated surgically. Preoperative preparation consists of removing gastric contents and restoring blood pressure. Research is also carried out to select further actions.
Evaluated:
- Time elapsed since the onset of the disease;
- Nature of origin, size and localization of the ulcer;
- The severity of peritonitis and the area of its distribution;
- Age characteristics of the patient;
- Presence/absence of additional pathologies;
- Technical features of the hospital and the level of professionalism of doctors;
There are organ-preserving operations (suturing) and radical ones (resection, excision of ulcers, etc.).
Suturing the perforation is indicated in the presence of widespread peritonitis, high surgical risk (associated with the presence of concomitant pathologies or the age of the patient), and the absence of a history of ulcers in young people. The technique consists of excision of the edges of the ulcer and their subsequent stitching with two rows of sutures. With this method of solving the problem, the shape of the organ and the diameter of its lumen are preserved. At the end of the operation, temporary drains are installed. Further treatment with antiulcer drugs is prescribed.
Gastric resection is an operation that leads to the loss of a significant part of the organ. After the transfer, disability is established. Indications are the presence of chronic, large-diameter ulcers, suspicion of the presence of malignant tumors, the patient’s age less than 65 years in the absence of concomitant pathologies during the decompression period, the development of acute inflammation and purulent peritonitis, 6-12 hours after the onset of the disease.
In the absence of peritonitis, suturing of the wall of the perforated hole can be performed in combination with selective proximal vagotomy.
Excision of the ulcer using truncal vagotomy and pyroplasty is used in the presence of an ulcer of the pyloric part of the stomach, a combination of perforation with bleeding, and stenosis.
The absence of surgical intervention necessarily leads to death in the coming weeks after the development of the disease.
Statistics of deaths after surgery show that after 6 hours no more than 4% of patients leave, after a day - no more than 40%.
Sample menu for the week
Therapeutic recovery diets cannot be called hungry, so their competent preparation and the involvement of nutritionists helps to diversify the menu and make it attractive to the whole family.
After a month of the recovery period after major operations, patients are usually sent home for the rest of their lives. This menu is suitable after removal of polyps on the rectum or after resection of the rectal section, after 3-4 months.
Day 1
In the morning: oatmeal with raisins with milk, green tea, crackers.
Lunch time: soup with meatballs and noodles, beetroot salad with prunes, black bread, rosehip infusion.
Afternoon snack: baked apple with cinnamon and honey, a glass of kefir or warm milk.
Evening: fish soufflé with mashed potatoes, peeled cucumber, jelly.
Day 2
In the morning: boiled buckwheat porridge with butter and sugar, green tea, biscuits with cheese.
Lunch time: boiled eggs, chicken broth with herbs and croutons, vinaigrette.
Afternoon snack: cottage cheese casserole, warm milk or a glass of dried fruit compote.
Evening: rice with vegetables, nelma steak with cream sauce.
Day 3
In the morning: a drink made from chicory, rice porridge with milk, a sandwich on dry bread made from cheese and butter.
Lunch time: fresh cabbage borscht with sour cream, chicken breast salad with cucumber, toast with lettuce, jelly.
Afternoon snack: zucchini casserole with cheese crust, lingonberry juice.
Dinner: meatballs with boiled buckwheat, green salad with cucumber, kefir.
Day 4
In the morning: milk soup with noodles, bread with cheese and herbs, green tea.
Lunch time: fish soup, tomato salad with sour cream, croutons, compote.
Afternoon snack: boiled egg, warm green tea.
Evening: meat cutlets with pasta, thick berry jelly.
Day 5
In the morning: steam omelette with onions and herbs, black tea with milk, sandwich with butter.
Lunch: pureed pumpkin soup with celery, dried fruit compote.
Afternoon snack: baked pear with honey, jelly.
Dinner: beef stew with vegetables in a pot, rosehip decoction.
Day 6
In the morning: semolina porridge, sandwich with cheese and butter.
Lunch time: chicken breast soup with homemade noodles, croutons, compote.
Afternoon snack: chicken soufflé with baked vegetables (bell peppers, carrots, eggplants).
Evening: white omelette, grilled chicken breast, kefir.
Day 7
In the morning: boiled rice porridge, compote, croutons.
Lunch time: meatball soup, croutons, beet salad.
Afternoon snack: baked apple with honey.
Evening: boiled meat, mashed potatoes, peeled cucumber, kefir.
Just before going to bed, you can drink kefir, yogurt, green tea, and thick jelly. Food can be divided into several meals and the volume can be changed. The presented menu is an approximate basis for a therapeutic diet.
This diet is based on pureed dishes, low-carbohydrate foods, and drinking plenty of fluids. There are absolutely no raw vegetables and fruits in the diet. The traditional menu for fasting days is diluted with a slag-free diet. Such nutrition cannot be called complete and healthy, so its duration is no more than 5 days. A slag-free diet is prescribed before surgery on the rectum and other parts of the intestine to cleanse the cavities of pathological deposits.
Diet after surgery for perforated gastric ulcer
The first rule for recovery and reducing the risk of relapse is strict adherence to the doctor’s instructions. An exception to the rule “if you can’t, but really want to” doesn’t work. During the postoperative period, a strict diet is established. It can last from 3 to 6 months. The diet becomes more complex gradually.
Basic principles of the diet:
- The daily number of meals is up to 6 times, in small portions.
- All foods taken must be puree or semi-liquid.
- Food should be steamed or boiled
- Salt should be taken in limited quantities
- You should also limit your intake of simple carbohydrates (sugar, chocolate, baked goods) and liquids.
On the 2nd day after the operation, mineral water, fruit jelly, and weak, slightly sweetened tea are allowed.
After 2-3 days, the diet is replenished with rosehip decoction, pureed soups and porridges made from rice and buckwheat. Vegetable puree soups made from boiled carrots, pumpkin, zucchini, potatoes or beets. You are allowed to eat a soft-boiled egg and a steam soufflé made from pureed cottage cheese.
On the 10th day after the operation, puree from boiled carrots, pumpkin, zucchini or potatoes is introduced into the diet. Gradually introduce steamed cutlets, soufflés, purees, quenelles, meatballs or zrazy from lean meats or fish. They add cheesecakes, puddings, and cottage cheese casseroles. You can also use fresh pureed cottage cheese. In addition, whole milk and non-acidic dairy products (acidophilus, yogurt, matsoni) are introduced.
Only after a month does it become possible to consume bread products: dried bread, stale bread, crackers.
After 2 months, it is allowed to add fresh sour cream to food and consume kefir.
On this topic:
Diet for stomach ulcers - what can and cannot be eaten?
Reviews and results
The recovery time depends on proper nutrition after gastric surgery. In addition, proper nutrition is the prevention of exacerbations of stomach diseases, and the basis for the patient’s well-being in the future. Most reviews note the importance and necessity of dietary nutrition after surgery.
- “... We performed an endoscopic operation - they sutured the perforated ulcer. I did not agree to the resection and promised myself that I would constantly monitor my diet and carry out anti-relapse treatment. The doctor warned that without this, the ulcer may recur. Since the operation was not traumatic, I recovered quickly, but my food was pure for a long time (about two months). Now I feel quite healthy, but I stick to a diet - boiled or baked dishes, no hot spices, no vinegar, and I have completely eliminated smoking and alcohol. I understand that my condition depends on nutrition”;
- “... After gastric resection due to perforation of an ulcer, I was on a diet for 8 months. At first it is strict and worn, then not worn. Now I only eat boiled dishes, low-fat and non-fried soups, I have excluded rolls and other baked goods (it makes me very stuffy), everything is spicy and smoked. I noticed that it became easier not only for the stomach, but also for the liver and intestines. I regret that I realized this only when I lost part of my stomach. Now diet for life. I can’t eat such large portions as before, I often refuse meals at work and with friends (everyone knows about my illness and is not offended). Of course, the operation and then the constant diet led to me losing a lot of weight. When I went back to work, following a diet became not very convenient - everything needs to be taken with you from home and warmed up. I don’t experience any other difficulties, since it’s not difficult for me to cook steamed cutlets or boil my own chicken.”