Peptic ulcer
(
ulcus pepticum
; Greek, peptein to digest) is an ulcer of the gastrointestinal anastomosis, sometimes occurring after drainage operations on the stomach or its resection. The term “peptic ulcer” also refers to a kind of ulcerative lesion of the esophagus, which, according to V. X. Vasilenko et al. (1971), according to a number of etiological and pathogenetic factors, resembles peptic ulcer of the stomach and duodenum (see Esophagus, diseases). In addition, in foreign literature the term “peptic ulcer” is used to refer to peptic ulcer disease in general.
Peptic ulcer after gastroenterostomy was first described by Berg (1897), and in Russian literature by K. M. Sapezhko (1901). The occurrence of peptic ulcer after gastric resection was first reported by Haberer (H. Haberer, 1922).
The frequency of peptic ulcers after gastroenterostomy, according to S. S. Yudin, ranges from 5 to 10%; after resection of the stomach, according to the summary data of V. M. Sitenko and V. I. Samokhvalov (1971), - 0.5-5%; after anthrumectomy with vagotomy - 0.5-1%; after gastric drainage operations with vagotomy, according to most authors, 5-10%.
Etiology and pathogenesis
The main cause of peptic ulcer is the high acid-producing function of the stomach, which persists in a number of patients after surgery. Education P. I. after operations that exclude the flow of bile into the stomach, the lack of neutralizing effect of bile on gastric juice contributes. So, according to S.S. Yudin, after gastroenterostomy according to Roux, the frequency of P. i. reaches 80%.
After drainage operations in combination with vagotomy, one of the reasons for the remaining high gastric secretion may be incomplete vagotomy, as well as chronic duodenal obstruction, causing impaired gastric evacuation.
After economical resection of the stomach, the formation of P. i. possibly as a result of leaving the pyloric mucosa in the area of the duodenal stump, which causes gastric hypersecretion due to the permanent release of gastrin or due to increased function of the vagus nerves (incomplete vagotomy). P. I. also develop in Zollinger-Ellison syndrome (see Zollinger-Ellison syndrome).
According to M. M. Levin (1961), 80% of all P. i. refers to marginal ulcers of the anastomosis. P. I. can also be localized in the efferent loop (up to 40 cm from the anastomosis), sometimes in the afferent loop and rarely in the gastric stump.
Peptic ulcer anastomosis
Making a diagnosis of peptic ulcer of the anastomosis is not difficult if there is a characteristic clinical picture and information about the surgical intervention performed. Diagnosis of the disease is aimed at determining the location and size of the defect, identifying complications and concomitant pathologies of the gastrointestinal tract. The most informative are:
- Esophagogastroduodenoscopy
. The introduction of a flexible endoscope into the esophagus and gastric stump allows one to assess the condition of the anastomosis, detect an ulcerative defect, and identify hyperemia and swelling of the mucous membrane. During endoscopy, a biopsy of the affected area is performed for subsequent histological examination. - X-ray of the stomach
. Contrasting the digestive tract using oral administration of barium sulfate helps to detect characteristic signs of a peptic ulcer on an x-ray - the presence of a “niche”, convergence of mucosal folds. The method is also used to assess gastric motor function. - Ultrasound of the abdominal cavity
. During an ultrasound examination, it is possible to study the structure of the organs of the digestive tract and hepatobiliary system, and the consistency of the anastomosis. The technique is complemented by duplex scanning of blood vessels to identify pathology of the celiac trunk and abdominal aorta. - Radionuclide research
. Intravenous administration of a drug labeled with a radioisotope is carried out to determine the secretory function of the gastric stump. With a peptic ulcer, there is an excessive accumulation of the isotope in the area of the anastomosis, which indicates an abandoned area of the antrum. - Histamine test
. The method makes it possible to study the basal and stimulated secretion of the gastric glands. The study is highly informative for the diagnosis of Zollinger-Ellison syndrome, in which there is high activity of basal secretion and a weak response to subcutaneous administration of histamine.
A clinical blood test shows moderate leukocytosis, a slight increase in ESR, and the amount of hemoglobin and red blood cells may decrease, which is a sign of bleeding from a peptic ulcer. A biochemical blood test determines hypoproteinemia, increased gastrin levels (with Zollinger-Ellison disease), and increased levels of calcium and parathyroid hormone (with hyperparathyroidism). To assess the quality of the vagotomy performed, an insulin test is performed, a positive result of which indicates the preservation of the vagus nerve fibers.
Differential diagnosis is carried out with other types of diseases of the operated stomach, malignant gastric neoplasia, primary ulcer of the small intestine, anastomotic leak, acute appendicitis, pancreatitis, cholecystitis. In addition to a gastroenterologist, the patient needs consultations with a surgeon, oncologist, hematologist, and endocrinologist.
Clinical picture
Characterized by intense pain in the upper abdomen. After gastrectomy, they are most often localized in the left hypochondrium. At the onset of the disease, pain occurs on an empty stomach, often at night, and is well relieved after eating and taking antacids (see). Frequent symptoms of P. i. are heartburn, vomiting, weight loss.
With a peptic ulcer, complications such as profuse bleeding, perforation, stenosis of the anastomosis, penetration into the pancreas, root of the mesentery of the small intestine, into the mesentery of the colon, small and transverse colon are possible. Penetration can cause the formation of an inflammatory infiltrate around the ulcer, as well as the occurrence of a gastrointestinal fistula. As the ulcer penetrates and an inflammatory infiltrate forms, the pain increases sharply, becomes constant, and often radiates to the lumbar region. Their intensity can only be reduced with painkillers.
Frequency.
Also on topic:
PATIENT
After a clear increase in the incidence of peptic ulcers from 1900 to 1950, the prevalence of this disease in Western countries for some reason began to decline. However, in some regions, especially South Africa and India, it is still very common.
In the recent past, peptic ulcers affected more than 10% of the US population, with a preponderance of men: it affected approximately 1 in 5 men and only 1 in 10 women. Currently, peptic ulcers are less common, and gender differences in incidence are disappearing. Although ulcers can develop at any age, they most often occur between 45 and 65 years of age.
Treatment
Treatment must be prompt. Conservative treatment, similar to treatment for peptic ulcer (see), is carried out in case of severe concomitant diseases or the patient’s refusal to undergo surgery.
Surgeries for peptic ulcers are very technically complex due to the need to separate numerous adhesions that have arisen in the abdominal cavity after previous interventions. The leading role belongs to vagotomy (see), edges should be an obligatory element of any operation undertaken regarding P. I. In case of P. i., which arose after drainage surgery on the stomach, anthrumectomy with vagotomy is indicated if the latter was not performed during previous operations, or revagotomy if it was performed but turned out to be incomplete. The nature of surgical intervention for P. i. after gastrectomy depends on its cause, which, however, cannot be established in all patients. If P. I. was the result of economical gastrectomy or increased function of the vagus nerves (after incomplete vagotomy), revagotomy is indicated. If a section of the antral wall is left in the so-called. gastric resection to switch off, its removal is indicated. Gastric resection in these cases is useless; it is indicated only for bleeding from an ulcer and stenosis of the gastroenteroanastomosis. With perforation of P. I. the perforation should be sutured and (in the absence of peritonitis and anastomotic stenosis) vagotomy. With P. I. with a large inflammatory infiltrate, palpable through the abdominal wall, as well as with penetration of P. i. It is advisable to perform vagotomy into the abdominal wall transthoracically.
Ulcer
Peptic ulcer or peptic ulcer
Peptic ulcer is a chronic disease in which a long-term non-healing defect forms in the wall of the stomach and/or duodenum. A serious complication of an ulcer can be perforation—the formation of a hole at the site of the defect that communicates with the abdominal cavity. The disease is characterized by seasonality. Exacerbations are more often observed in spring and autumn and practically do not occur at other times of the year.
Causes
The development of the disease can be facilitated by:
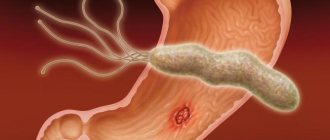
- Helicobacter pylori infection. The bacterium Helicobacter pylori causes inflammation of the mucous membranes of the stomach and duodenum, which leads to their thinning. As a result, hydrochloric acid “burns” ulcers in the walls of organs.
- Smoking. Nicotine causes spasm of the blood vessels that supply the mucous membranes, which also leads to their damage.
- An imbalance between the protective mechanisms of the mucous membranes and external aggressive factors. An imbalance can occur against the background of chronic gastritis, with increased secretion of hydrochloric acid, reflux of bile into the stomach, or taking non-steroidal anti-inflammatory drugs.
- Unfavorable heredity. It has been established that peptic ulcer disease develops 3-4 times more often in those who have blood relatives with the same diagnosis.
- Irregular meals.
- Stress.
- Diseases of the endocrine or cardiovascular system.
Symptoms
The leading complaint of patients is pain. Most often they are dull, moderate in nature and are felt in the epigastric region (sometimes radiating to the lower back, under the shoulder blade, upper abdomen). In case of duodenal ulcer, pain occurs mainly at night, on an empty stomach; in case of gastric ulcer - immediately after eating.
Some patients may experience:
- heartburn,
- nausea,
- vomit,
- loss of appetite,
- rumbling in the stomach,
- constipation
Very rarely, peptic ulcer disease is asymptomatic (so-called “silent” ulcers).
Diagnosis and treatment
The examination of the patient begins with examination and questioning. The doctor clarifies the nature of the pain, collects anamnesis and palpates the abdomen. To clarify the diagnosis you need:
- esophagogastroduodenoscopy (EGD, direct examination of the mucous membranes of the stomach and duodenum using a mini-camera),
- pH-metry (determination of the acidity of gastric juice, carried out during endoscopy),
- X-ray examination (allows you to determine the depth of the ulcer),
- test for Helicobacter pylori.
A supporting role is played by:
- stool occult blood test,
- general blood analysis,
- Ultrasound of the abdominal organs.
Ulcer treatment includes:
- anti-Helicobacter therapy,
- diet,
- taking medications that reduce acid production in the stomach and promote healing of the mucous membranes.
To prevent relapse, the patient is advised to normalize his diet, give up bad habits and observe a work-rest regime.
Timely diagnosis will allow you to avoid dangerous complications of an ulcer. If you are worried about abdominal pain and various digestive disorders, do not waste time - contact the Spectra clinic. In 1-2 visits you will be able to undergo a full examination, including gastroscopy, radiography and a set of laboratory tests. An experienced gastroenterologist will conduct a consultation and select the appropriate treatment.
Forecast
The ability to work with peptic ulcers is usually completely impaired. It often cannot be maintained even with intensive therapeutic measures. The degree of restoration of ability to work after surgery depends on the nature of the surgical intervention performed. After vagotomy, patients return to work much more often and faster than after high gastrectomy.
Bibliography:
Levin M. M. Repeated operations for diseases of the operated stomach, p. 19, Kharkov, 1961; Mayat V.S. et al. Gastric resection and gastrectomy, M., 1975; Pantsyrev Yu. M. Pathological syndromes after gastrectomy and gastrectomy, p. 154, M., 1973; Shalimov A. A. and Saenko V. F. Surgery of the stomach and duodenum, p. 303, Kyiv, 1972; — Yudin S.S. Sketches of gastric surgery, M., 1965; Green WE a. O. Management of recurrent peptic ulceration, Brit. J. Surg., v. 65, p. 422, 1978; Sandsmark M. The prQblems of recurrent gastro-jejunal ulcer, Ann. Chir. Gynaec. Fenn., v. 66, p. 1, 1977.
I. V. Kliminsky.
Symptoms
Ulcer symptoms vary. Many ulcer patients experience minimal or no stomach upset. Some report a burning sensation in the upper abdomen, others report that hunger pain occurs one to three hours after eating and in the middle of the night. Such pain often quickly decreases after eating or neutralizing the acid with special means. Some patients have persistent pain even after the ulcer is completely healed. Others experience no pain at all, even when the ulcers return. Ulcers often occur spontaneously and the person is unaware of their presence, unless serious complications (such as bleeding or perforation) occur.