The intestines, like all organs, require nutrition to ensure their smooth functioning. Not only the cells of the inner layer, but also the “residing” microorganisms need the supply of protein, vitamins, energy and plastic materials. In an adult, they weigh up to two kg.
Intestinal ischemia develops by analogy with changes in the coronary vessels of the heart, often simultaneously. It is not for nothing that it is called “abdominal toad” (angina pectoris - “angina pectoris”). Its result is a violation of the patency of the intestinal arteries with the subsequent formation of necrotic areas in the intestine.
Ischemic intestinal disease is a difficult disease to diagnose. Until now, it is impossible to provide accurate information about the prevalence among the population, since the pathology often occurs under other masks.
What arteries does the intestinal blood supply depend on?
Blood supply in the abdominal cavity depends on three main arterial trunks:
- celiac artery,
- inferior and superior mesenteric (mesenteric).
They “take over” 40% of the body’s total blood flow. Between the vessels there is an extensive network of auxiliary collateral branches, which take on a compensatory role when blood flow through the main arteries is impaired.
The celiac trunk feeds the initial section of the intestine and all the organs of the gastrointestinal tract lying in the upper floor of the abdominal cavity. It extends directly from the abdominal aorta in the area of the diaphragmatic opening of the esophagus, and is only 2 cm in length. The place is known as one of the “favorite” localizations of atherosclerotic plaques.
Both mesenteric arteries branch into numerous branches and form a network of auxiliary vessels
The mesenteric arteries also arise from the abdominal aorta, but below the celiac trunk. The superior mesenteric artery supplies:
- small intestine (except duodenum);
- blind;
- ascending;
- ½ transverse colon.
From the inferior artery, blood flow is directed to:
- left half of the transverse colon;
- descending;
- sigmoid;
- rectum.
Diagnostics
With the correct diagnostic approach, it is possible not only to determine the disorder of the intestinal blood supply itself, but also the reasons that caused it. In this regard, collecting anamnesis and asking the patient about the course of the disease plays an important role. Clarifying the time of onset of pain, its intensity, and the nature of stool can significantly help the doctor in choosing surgical treatment, since there is still no other alternative in the case of mesothrombosis.
Diagnosis of OMAN involves selective angiography, which makes it possible to determine the level and nature of artery blockage, which will also be important for providing emergency care, naturally, in the form of surgical intervention.
The laparoscopic method still remains decisive in any type of acute surgical pathology, where mesothrombosis is no exception. Rather, on the contrary, in case of a decompensated circulatory disorder, the surgeon has only 2 hours at his disposal, so it is clear that there is no need to delay the diagnosis. With the help of laparoscopy, it is possible to clarify the nature of the damage to the intestinal tract within a short time.
Thrombosis of mesenteric veins
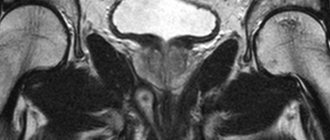
Thrombosis of mesenteric vessels, diagnosed on the basis of acute abdominal symptoms and using medical imaging methods, carries a huge risk to human life. The most commonly used is CT (computed tomography), but sonography or MRI (magnetic resonance imaging) are also used. Mesenteric angiography is an X-ray examination, considered the most informative method, which with a high percentage of probability allows you to determine the location of the blood clot.
Thrombosis of mesenteric arteries
{banner_banstat9}
If the doctor suspects that the intestinal arteries are blocked by a blood clot, or there is a suspicion of thrombosis of the mesenteric vessels, he may prescribe the following research methods:
- CT scan of the abdominal cavity;
- ultrasonography;
- magnetic resonance imaging;
- MRA (magnetic resonance angiography);
- arteriography of abdominal vessels.
Laboratory diagnostics
There are no specific laboratory markers of intestinal ischemia. Any significant changes appear in the stage of necrosis, which makes their detection unsuitable for early diagnosis and screening.
- A complete blood count may be within normal limits initially. Leukocytosis and/or a shift of the leukocyte formula to the left is observed in more than 50% of cases in the final stages, as the disease progresses and complications develop. The hematocrit is initially elevated but quickly decreases as gastrointestinal bleeding develops.
- Biochemistry.
- Amylase levels are moderately elevated in more than 50% of patients, but this sign has low specificity.
- Elevated phosphate levels were initially considered a sensitive sign, but more recent studies have shown the test's sensitivity to be only around 25-33%.
- Metabolic acidosis is observed in the final stages of the disease, but this is also a nonspecific finding.
- A serum bicarbonate level of less than 24 mmol/L has a sensitivity of about 36%.
- The lactate level increases only in the stage of severe ischemia (sensitivity - 90-96%, specificity - 60-87%).
- The increase in LDH levels and the diagnostic value of this test remains a controversial issue.
- High cholesterol levels and other specific laboratory markers of atherosclerosis may indicate it as the underlying cause.
- Coagulogram. Elevated D-dimer levels may indicate acute ischemia, but clinical data are not yet sufficient to assess the sensitivity and specificity of the sign.
How does the peculiarity of the blood supply affect the risk of ischemia in the arterial area?
The location of the inferior celiac artery and a well-developed network of anastomoses between the branches make it less vulnerable to stenosis processes. Therefore, ischemia of the intestine located in the left half of the abdomen occurs quite rarely. This requires concomitant diseases with damage to the superior artery, collaterals or abdominal aorta.
The celiac trunk and superior mesenteric artery arise at right angles. This promotes thrombus formation, sedimentation of emboli, and microorganisms.
Surgeons noted the following patterns:
- Thrombosis and embolism are more common in the area of the superior mesenteric artery, and there are more opportunities for the development of inflammation (arteritis). Anatomically, separate sections of the intestine are identified between the branches of the outgoing small arteries, which represent the most likely areas of necrosis.
- Atherosclerosis often develops in the lower artery.
- The patency of the celiac trunk is more dependent on the anatomical features of the vessel.
The stages of development of intestinal ischemia are sequentially formed at a higher (acute process) or lower speed (chronic form). Morphological changes in tissues made it possible to identify:
- ischemia - the lack of blood flow into the intestinal walls is compensated by collateral vessels, metabolic processes in cells slow down, epithelial degeneration occurs, the production of enzymes and the breakdown of biochemical substances ceases, peristalsis is impaired (the function of promoting and removing waste);
- infarction - irreversible tissue necrosis (gangrene) in the intestinal area with disruption of the activity of the entire intestine;
- peritonitis - the addition of inflammation, thinning and rupture of the necrotic area with the release of contents into the abdominal cavity, a severe form of general damage to the body.
General information
Intestinal infarction is an acute disturbance of mesenteric circulation followed by intestinal necrosis and the development of peritonitis. This pathology is one of the serious problems of abdominal surgery. Most often, embolism, thrombosis, atherosclerosis and non-occlusive ischemia of intestinal vessels occur against the background of severe heart pathology. Due to the increasing percentage of the elderly population and the rejuvenation of cardiovascular pathology, intestinal infarction is becoming more common (0.63% compared to isolated cases at the end of the last century). The average age of patients is 70 years, women predominate (more than 60%). Considering the advanced age of the patients and the mass of underlying diseases, it can be quite difficult to decide on surgical treatment tactics.
Another problem is that it is quite difficult to make a diagnosis, and it is almost impossible to confirm it without angiography before surgery. Due to erroneous diagnosis, preoperative preparation is delayed; During this time, irreversible changes occur in the intestine, leading to the death of the patient. The situation is aggravated by the fact that in recent years, intestinal infarction has become significantly younger (every tenth patient is under 30 years old), and radical resection of the intestine in the late stage of the disease leads to permanent disability.
Intestinal infarction
Why does ischemia occur?
The causes determine the type of ischemia. It is more convenient to divide them into:
- Extravascular (extravasal) - usually this is external pressure on the arteries from the falciform ligament of the diaphragm, enlarged nerve ganglia, tumors located in the area of the arteries. There may be anomalies in the location and origin of blood vessels, kinks, and increased tortuosity.
- Intravascular (intravasal) - depend on atherosclerotic deposits from the inside, obstructing blood flow, or pronounced aorto-arteritis of an inflammatory nature with the accumulation of immune cells, proliferation of the inner membrane, impeding the passage of blood.
A computed tomogram revealed adhesive obstruction as the cause of small intestinal ischemia
Another option classifies intestinal ischemia into the following types.
Occlusive, associated with blocking of the vascular trunk by a thrombus, embolus, inflammatory changes. The main reasons are varied:
- heart defects that form a pathological communication between the atria and ventricles, through which blood clots from the veins of the lower extremities enter the left ventricle, aorta and mesenteric vessels;
- atrial fibrillation - promotes the separation of parietal intracardiac thrombi;
- congestive heart failure;
- pronounced vascular atherosclerosis.
Non-occlusive - independent of the condition of the arteries, occurs in 50% of cases. More often than not, the exact cause cannot be determined. Development is promoted by:
- Heart arythmy;
- low blood pressure in case of shock, fainting;
- irrational use of antihypertensive drugs that cause a sharp decrease in blood pressure;
- dehydration of the body;
- development of heart failure.
Depending on the underlying cause, intestinal ischemia can develop acutely (thromboembolism, shock) or take a chronic form (atherosclerosis, aortoarteritis).
Causes
All causative factors leading to intestinal infarction can be divided into three groups: thrombotic, embolic and non-occlusive. The thrombotic variant of the pathology is characterized by thrombosis of the mesenteric arteries (less often veins) in their proximal sections. Most often, the thrombus is localized at the mouth of the superior mesenteric artery. Thrombosis of the visceral branches of the aorta can be caused by increased blood clotting, polycythemia, heart failure, pancreatitis, trauma, tumors, and taking hormonal contraceptives.
The embolic variant of the disease develops when the mesenteric vessels are blocked by thromboembolism that migrated from the proximal parts of the vascular bed. The reason for this is most often atrial fibrillation, the formation of parietal blood clots against the background of myocardial infarction, aortic aneurysm, and severe coagulation disorders. After vessel occlusion, the embolus may move to the distal portions and branches of the vessel, causing intermittent, migrating ischemia.
The non-occlusive type of intestinal infarction is associated not with obstruction of the visceral vessels, but with a decrease in blood flow through them. The reasons for the limitation of visceral blood flow may be mesenteric thrombosis, decreased cardiac ejection fraction, severe arrhythmia, mesenteric vasospasm, hypovolemia in shock, sepsis, and dehydration. Factors from these three groups are often combined.
Factors contributing to the development of intestinal ischemia
Risk factors that provoke the development of the disease may be:
- age period over fifty years;
- hypertension, causing pathology of the heart and blood vessels;
- diabetes;
- nicotine poisoning, which affects arterial tone, when smoking;
- increased levels of low-density lipids in the blood, which contribute to atherosclerosis;
- obesity;
- the presence of vascular pathology in the form of coronary, cerebral insufficiency, atherosclerosis of the vessels of the extremities;
- diaphragmatic hernia;
- previous abdominal surgeries;
- blood diseases, vasculitis with increased coagulability;
- long bed rest;
- women taking hormonal contraceptives.
Features of diet No. 3 for constipation
The weekly dietary menu is designed taking into account the balance of proteins and carbohydrates in the diet. At the same time, there is an increase in the amount of fat due to the inclusion of vegetable oils. The diet involves consuming 100–120 g of fat, 85–100 g of protein, 450–500 g of carbohydrates.
Table No. 3 does not provide for the obligatory chopping or grinding of food. It is allowed to consume boiled and baked dishes, as well as carbonated mineral water in moderate quantities. You can cook porridge with milk diluted with water in a 1:1 ratio.
Drinks and foods whose temperature is below 15 °C increase peristalsis and reduce the production of gastric juice. Therefore, for constipation, it is recommended to drink chilled drinks. Before breakfast, it is advisable to drink a glass of cold water, and at night - compote or kefir. In addition, to soften the stool, it is useful to take 1-2 tablespoons of unrefined vegetable oil on an empty stomach. The oil coats the intestines and improves the movement of feces.
You can follow the diet for a long time. With this diet, the frequency and consistency of stools are normalized. This diet is indicated for constipation caused by an unbalanced diet and a sedentary lifestyle.
Prohibited Products
Like other diets, “Table No. 3” involves excluding certain foods from the diet. These include:
- flour products from yeast and puff pastry;
- fatty fish and meat, strong meat broths;
- radish, horseradish, garlic and other spicy vegetables;
- spicy sauces, mustard, hot pepper;
- strong tea, coffee and other caffeinated drinks;
- canned foods, fried eggs;
- legumes, mushrooms (mushroom broths are allowed);
- bananas, dogwood, blueberries, nuts;
- drinks with tannins: jelly, cocoa, drinks made from quince, bird cherry and blueberry.
Whole milk, smoked meats, fried and pickled foods are not recommended. You also need to exclude alcoholic drinks, chocolate, pasta, and legumes. Prohibited foods include rice, semolina, sweets with cream, and margarine. There is no need to eat foods that are difficult to digest: mashed potatoes, canned food, hard-boiled eggs, slimy soups.
Types of ischemia
In addition to acute and chronic forms, types of intestinal ischemia are distinguished depending on the severity of the compensatory function of auxiliary vessels. They may reflect the stage of the disease:
- compensation - mesenteric blood flow is not impaired due to the expansion of collateral arteries, intestinal function is not affected;
- subcompensation - blood circulation in the layers of the intestine is supported by the maximum efforts of collaterals, glandular and epithelial cells perform a minimum of their functions;
- decompensation - foci of necrosis form in place of normal cells, the function is impaired.
Clinicians distinguish the following forms:
- Ischemia of the colon - occurs against the background of a cancerous tumor, the diagnosis is made by colonoscopy, surgical removal of the tumor allows all symptoms to be relieved.
- Acute mesenteric ischemia - develops suddenly, treatment requires emergency surgery. The diagnosis is very difficult to make. Even taking into account all the signs from blood tests, ultrasound, and angiography does not show sufficiently reliable symptoms. The final diagnosis is made after opening the abdominal cavity on the operating table. This is where decisions about treatment options are made.
- Chronic mesenteric ischemia - since the disease develops gradually, there is enough time for examination and confirmation of the diagnosis. Often detected in patients with inflammation of the colon, which is regarded as ischemic colitis. Angiography of the peritoneal vessels makes it possible to clarify the nature of the disease.
- Ischemia associated with thrombus formation in the mesenteric vein - stagnation of blood below the thrombus leads to compression of the arterial trunks. Often observed in patients with increased blood clotting.
Non-occlusive mesenteric ischemia
Approximately 20% of mesenteric ischemia is non-occlusive. The pathogenesis of nonocclusive mesenteric ischemia (NMI) is not entirely understood but is often associated with low cardiac output associated with diffuse mesenteric vasoconstriction. Vasoconstriction of splanchnic organs is a response to hypovolemia with decreased cardiac output and hypotension. As a result of insufficient blood flow, intestinal hypoxia occurs, which inevitably leads to intestinal necrosis. Conditions predisposing to NMI include age over 50 years, myocardial infarction, heart failure, liver and kidney disease, and major abdominal or cardiovascular surgery. However, these patients may not have risk factors. This condition often develops in patients in critical condition with a host of concomitant diseases; NMI often begins unexpectedly and results in high mortality.
Clinical picture
Symptoms of intestinal ischemia depend on the form of the disease and the location of the affected branch of the vessel. Different types have their own preferential reasons. Therefore, the clinic is somewhat different.
Acute intestinal ischemia is characterized by:
- sudden development of sharp abdominal pain localized in the upper right and near the navel, quickly spreading throughout the entire abdomen;
- the urge to defecate due to increased intestinal motility;
- diarrhea, blood in stool;
- nausea with vomiting;
- temperature increase.
In the acute form, there is pain when touching the skin and palpation of the abdomen, but there are no peritoneal symptoms
Chronic ischemia occurs gradually, symptoms develop over years. The patient complains of:
- paroxysmal pain in the abdominal cavity, occurring half an hour after eating and lasting up to three hours (“abdominal toad”);
- the pain often does not have a specific localization or is bothersome around the navel, in the area of the large intestine (ischemic colitis);
- over several months the pain becomes more intense;
- at the beginning of the disease, the pain is relieved by antispasmodics, but over time the drugs do not alleviate the patient’s condition;
- you have to refuse food for fear of pain, so you lose weight;
- weight loss is also associated with malabsorption of nutrients;
- the stomach is almost constantly swollen, rumbling, pronounced noises are heard on auscultation;
- tendency to diarrhea followed by constipation;
- frequent nausea and vomiting.
Ischemic bowel disease
Surgical department No. 2 (city center for gastroduodenal bleeding of ulcerative etiology), surgeon Konkin D.K.
Ischemic intestinal disease (abdominal ischemic disease) is an acute or chronic insufficiency of blood supply in the celiac, upper or lower mesenteric (mesenteric) arteries, leading to insufficiency of blood flow in certain areas or in all parts of the intestine.
Etiology and pathogenesis
The main causes of ischemic bowel disease are:
- atherosclerosis, localized at the mouths of the corresponding arteries (the most common cause);
- systemic vasculitis (nonspecific aortoarteritis, Buerger's thromboangiitis obliterans, panarteritis nodosa, etc.);
- systemic connective tissue diseases;
- fibromuscular dysplasia;
- abnormalities of vascular development (hypoplasia);
- compression of blood vessels from the outside (tumor, adhesions, enlarged lymph nodes);
- infective endocarditis;
- sepsis;
- hereditary hemolytic (microspherocytic) anemia;
- polycythemia, etc.
Impaired blood supply to various parts of the intestine leads to pronounced dystrophic, ischemic (various degrees of severity) changes in the intestinal wall and (as the highest degree of ischemia) intestinal necrosis.
Classification
Voleu et al. (1978) propose the following classification of mesenteric circulation disorders:
- Acute mesenteric ischemia.
- Non-occlusive mesenteric ischemia.
- Embolism of the superior mesenteric artery.
- Thrombosis of the superior mesenteric artery.
- Local segmental ischemia.
- Chronic mesenteric ischemia (“abdominal tonsillitis”).
- Colon ischemia:
- reversible ischemic colopathy;
- transient ulcerative ischemic colitis;
- chronic ulcerative ischemic colitis;
- colon stricture;
- gangrene of the colon.
The following describes the diagnosis of the most important forms of ischemic intestinal disease.
- Acute mesenteric ischemia.
1.1 Non-occlusive mesenteric ischemia
One of the main reasons causing the development of non-occlusive mesenteric ischemia is heart failure of various etiologies. The clinical picture of non-occlusive mesenteric ischemia is similar to that of embolism and thrombosis of the superior mesenteric artery. However, all clinical manifestations are much less pronounced, including pain. Characterized by diarrhea, rumbling in the stomach, flatulence, weight loss.
1.2. Embolism of the superior mesenteric artery
The superior mesenteric artery supplies the entire small intestine, the cecum, the ascending colon, and part of the transverse colon.
The most common sources of embolism of the superior mesenteric artery are thrombi in the left atrium, on prosthetic or pathologically altered valves (mitral or aortic), and particles of atheromatous plaques.
The main clinical signs of embolism of the superior mesenteric artery:
- sudden sharp pain in the navel or right upper quadrant of the abdomen;
- cold clammy sweat;
- vomit;
- diarrhea (does not appear immediately, sometimes after a few hours);
- intestinal bleeding (discharge of blood or mucus stained with blood from the anus) is a sign of infarction of the intestinal mucosa; appears after a few hours;
- severe bloating, slight pain in the abdominal wall upon palpation;
- the appearance of symptoms of peritoneal irritation with the progression of the pathological process (pronounced tension of the abdominal wall), which indicates necrosis of all layers of the intestinal wall and the development of peritonitis; during this period, bowel sounds disappear;
- presence of vascular murmur in the epigastrium;
- drop in blood pressure, tachycardia;
- increased body temperature;
- pronounced leukocytosis;
- increased pneumatization of intestinal loops on a plain radiograph of the abdominal cavity;
- occlusion of the superior mesenteric artery detected by percutaneous transfemoral retrograde angiography. There is no consensus on the need to perform it, however, many surgeons consider this diagnostic procedure necessary.
1.3. Thrombosis of the superior mesenteric artery
The most common cause is widespread atherosclerosis. The clinical picture of thrombosis of the superior mesenteric artery is basically similar to the embolism clinic described above, however, thrombosis differs in that the abdominal pain is less intense and is not cramping in nature. Mesenteric thrombosis can be latent for some time. However, in the future, as intestinal ischemia increases, clinical symptoms also increase, intestinal infarction and clinical peritonitis develop, and bowel sounds disappear.
- Chronic mesenteric ischemia (“abdominal tonsillitis”)
The main causes of chronic mesenteric ischemia are obliterating atherosclerosis and nonspecific aortoarteritis.
The celiac trunk and superior mesenteric artery are most often affected; damage to the inferior mesenteric artery is observed less frequently.
The classification of chronic mesenteric ischemia by B.V. Petrovsky et al is of great practical importance. (1985), according to which three stages are distinguished:
- stage - relative compensation. At this stage, the dysfunction of the gastrointestinal tract is insignificant and the disease is detected by chance when examining patients for some other reason;
- stage (subcompensation) - characterized by severe intestinal dysfunction, abdominal pain after eating;
- stage (decompensation) - manifested by intestinal dysfunction, constant abdominal pain, progressive weight loss.
Clinical picture
The first clinical manifestations of chronic mesenteric ischemia appear in stage II according to the classification of B.V. Petrovsky.
The leading clinical symptoms are the following:
- Abdominal pain. Pain during chronic mesenteric ischemia is referred to by many as “abdominal claudication” or “abdominal intermittent claudication.” Its main features:
- clearly associated with food intake, occurs 20-40 minutes after eating;
- does not have a clear localization (can be felt in the epigastrium, around the navel, in the projection of the large intestine);
- has a cramping, spastic nature;
- treated with nitrates and antispasmodics in the initial period;
- significantly increases with the progression of the pathological process in the mesenteric arteries.
- Intestinal dysfunction. Chronic intestinal ischemia leads to its dysfunction, which is manifested by severe flatulence and rumbling in the stomach after eating, constipation; With a long course of the disease, diarrhea appears.
- Auscultatory signs of abdominal ischemia. Characteristic signs of mesenteric ischemia are detected by auscultation of the abdomen:
- systolic murmur at a point located in the middle of the distance between the xiphoid process and the navel (projection of the superior mesenteric artery);
- increased intestinal peristaltic sounds after eating.
- Progressive weight loss of patients. With severe mesenteric ischemia, a decrease in the body weight of patients is noted. This is due to patients’ refusal to eat (since eating causes significant abdominal pain) and a violation of the intestinal absorption capacity.
- Aortoangiography data allows one to verify the diagnosis of mesenteric ischemia (narrowing and prestenotic dilatation, deformation of the upper or lower mesenteric artery are detected).
Ischemic colitis
Ischemic colitis is a chronic inflammation of the large intestine caused by ischemia.
The blood supply to the large intestine is provided by the superior and inferior mesenteric arteries. The superior mesenteric artery supplies the entire small, cecum, ascending and partially transverse colon; inferior mesenteric artery - left half of the colon.
With ischemia of the large intestine, a significant number of microorganisms populating it contributes to the development of inflammation in the intestinal wall (even transient bacterial invasion is possible). The inflammatory process caused by ischemia of the colon wall further leads to the development of connective tissue in it and even the formation of a fibrous stricture. The splenic flexure and left parts of the colon are most commonly affected by ischemic colitis.
Diagnosis of ischemic colitis
The following circumstances help in diagnosing ischemic colitis:
- age over 60-65 years;
- the presence of coronary artery disease, arterial hypertension, diabetes mellitus, obliterating atherosclerosis of peripheral arteries (these diseases significantly increase the risk of developing ischemic colitis);
- episodes of acute abdominal pain followed by intestinal bleeding;
- the corresponding endoscopic picture of the condition of the colon mucosa and the results of histological examination of colon biopsies;
- strictures in the area of the splenic flexure of the colon.
Clinical picture:
- Stomach ache. Pain in the abdomen appears 15-20 minutes after eating (especially a large meal) and lasts from 1 to 3 hours. The intensity of the pain varies, and is often quite severe. As the disease progresses and fibrous strictures of the colon develop, the pain becomes constant.
The most common localization of pain is the left iliac region, the projection of the splenic flexure of the transverse colon, and less commonly the epigastric or periumbilical region.
- Dyspeptic disorders. Almost 50% of patients experience decreased appetite, nausea, bloating, and sometimes belching of air and food.
- Stool disorders. They are observed almost constantly and are manifested by constipation or diarrhea, alternating with constipation. During an exacerbation, diarrhea is more common.
- Weight loss for patients. A decrease in body weight in patients with ischemic colitis is observed quite naturally. This is explained by the limitation of the amount of food and the frequency of its intake (due to increased pain after eating) and a violation of the absorption function of the intestine (quite often, along with ischemia of the colon, there is a deterioration in blood circulation in the small intestine).
- Intestinal bleeding. Observed in 80% of patients. The intensity of bleeding varies - from the admixture of blood in the stool to the release of significant amounts of blood from the rectum. Bleeding is caused by erosive and ulcerative changes in the mucous membrane of the colon.
- Objective abdominal syndrome. Exacerbation of ischemic colitis is characterized by mild signs of irritation of the peritoneum, tension of the abdominal muscles. On palpation of the abdomen, diffuse sensitivity is noted, as well as pain mainly in the left iliac region or the left half of the abdomen.
Symptoms of severe irritation of the peritoneum, especially those that persist for several hours, make one think about transmural necrosis of the intestine.
Laboratory and instrumental data
- CBC: characterized by pronounced leukocytosis, a shift in the leukocyte formula to the left, and an increase in ESR. With repeated intestinal bleeding, anemia develops.
- OAM: no significant changes.
- Coprological analysis: a large number of erythrocytes, leukocytes, and intestinal epithelial cells are found in the stool.
- BAK: decrease in the content of total protein, albumin (with a long course of the disease), iron, sometimes sodium, potassium, calcium.
- Colonoscopy: performed strictly according to indications and only after acute symptoms have subsided. The following changes are revealed: nodular areas of edematous mucous membrane of a blue-purple color, hemorrhagic lesions of the mucous membrane and submucosal layer, ulcerative defects (in the form of points, longitudinal, serpentine), strictures are often found, mainly in the area of the splenic flexure of the transverse colon.
Microscopic examination of colon biopsies reveals edema and thickening, fibrosis of the submucosal layer, its infiltration with lymphocytes, plasma cells, and granulation tissue in the area of the bottom of the ulcers. A characteristic microscopic sign of ischemic colitis is the presence of multiple hemosiderin-containing macrophages.
- Survey radiography of the abdominal cavity: an increased amount of air is determined in the splenic angle of the colon or its other parts.
- Irrigoscopy: performed only after relief of acute manifestations of the disease. At the level of the lesion, narrowing of the colon is determined, above and below - expansion of the intestine; haustra poorly expressed; sometimes nodular, polyp-like thickenings of the mucous membrane and ulcerations are visible. In marginal areas of the intestine, finger-like imprints (the “thumbprint” symptom) are detected, caused by swelling of the mucous membrane; jaggedness and unevenness of the mucous membrane.
- Angiography and Doppler ultrasonography: a decrease in the lumen of the mesenteric arteries is detected.
Differential diagnosis
Ischemic colitis has many common clinical manifestations with Crohn's disease and ulcerative colitis: abdominal pain, dyspeptic syndrome, stool disorders, intestinal bleeding, formation of ulcers of the mucous membrane.
Examination program
- General blood and urine analysis.
- Coprological analysis: coprocytogram, bacteriological examination, protozoa examination.
- BAK: content of total protein, protein fractions, aminotransferases, bilirubin, sodium, potassium, iron, calcium.
- Ultrasound of the abdominal organs and retroperitoneal space.
- Endoscopic examination of the intestine (sigmoidoscopy, colonoscopy), histological examination of biopsy specimens.
- Irrigoscopy.
- Doppler ultrasound of the celiac trunk and mesenteric arteries.
Clinical features for different forms of ischemia
With ischemia of the colon, the symptoms appear moderately, complications are rare. Elderly people get sick more often. Symptoms are expressed in paroxysmal pain in the left half of the abdomen. The following factors take part in the development:
- atherosclerosis of mesenteric vessels;
- condition after surgery on the heart, blood vessels, abdominal organs, and gynecological diseases in women;
- injury in the abdominal area;
- general sepsis;
- artery thrombosis;
- hypotension;
- intestinal obstruction due to tumor, hernia, severe adhesions;
- spastic contraction of blood vessels during treatment with migraine drugs, hormonal agents;
- sports activities, especially running;
- the influence of chronic use of drugs such as cocaine and amphetamine.
A catheter from the femoral artery runs along the spine; a contrast agent injected into the abdominal aorta shows a “stump” of the mesenteric artery with its complete obstruction
Acute mesenteric ischemia most affects the small intestine. Her reasons:
- thromboembolism from the heart into the mesenteric vessels after heart surgery, attacks of paroxysmal fibrillation;
- may manifest itself during exacerbation of chronic ischemia in the vessels.
Ischemia due to a thrombus in the mesenteric veins occurs when:
- acute and chronic pancreatitis (inflammatory process in the pancreas);
- in case of any intestinal infection;
- liver cirrhosis;
- cancerous tumor in the digestive organs;
- intestinal diseases (ulcerative colitis, Crohn's disease);
- increased blood clotting, hormonal therapy;
- abdominal injuries.
Colon ischemia
The condition is also called ischemic colitis. Ischemia of the colon affects elderly people over 60 years of age. There are cases of the disease at a young age. It is not always possible to establish the cause of the pathology. The main etiological factors include:
- Large amounts of fatty tissue inside large arteries or atherosclerosis.
- Chronic pancreatitis.
- Severe hypotension caused by severe blood loss, trauma, surgery, and heart disease.
- Arterial thrombosis. When a blood clot blocks the flow of blood through the arteries supplying an organ.
- Intestinal obstruction, which is often provoked by tissue scarring, hernia, and tumor growths.
- Previously performed surgical interventions to eliminate pathologies of blood vessels, heart, gastrointestinal tract, and genital organs.
- Diseases that increase or decrease coagulability: lupus, hemoglobinopathy, vascular vasculitis.
- Uncontrolled use of drugs to narrow the vascular walls, especially for heart pain, headaches, or hormonal drugs, such as estrogen.
- Use of methamphetamine and cocaine.
Ischemia of the large intestine manifests itself:
- sudden sharp pain on the left in the iliac region;
- modification of blood clots in stool;
- rapid development.
Diagnosis of the disease
For diagnosis, general blood and stool tests play a supporting role. Leukocytosis indicates ongoing inflammation. Increased coagulability indicates the possibility of blood clot formation. In a stool analysis, the mass of undigested food particles, blood cells, and elements of inflammation are determined.
Angiography involves injecting a contrast agent into the femoral artery through a long catheter to the abdominal aorta, followed by a series of images. The technique is very important for quickly making a diagnosis and deciding on treatment.
Magnetic resonance angiography allows for a layer-by-layer study of blood flow in the vessels.
Doppler study is carried out to assess the speed of blood flow and determine the specific location or area of the narrowed vessel, the location of the blood clot, and its size.
Colonoscopy - using a flexible endoscopic tube inserted into the rectum, the condition of the mucous membrane is studied and the extent of intestinal damage is revealed.
Esophagogastroduodenoscopy is performed with an endoscope to identify changes in the initial parts of the small intestine.
Laparoscopy - in an operating room, an endoscope is inserted into the abdominal cavity through a small incision to obtain visual information
Mesenteric venous thrombosis
This condition develops against the background of blockage of a vein by a blood clot. The veins come from the intestinal tissues, therefore, when they are blocked, the blood does not find a way out of the organ. As a result, blood accumulates in the vessels, their walls thicken. Bleeding may occur in this area. Causes:
- infection of the peritoneum;
- severe abdominal injury;
- tumor formation in the gastrointestinal tract;
- certain types of hormonal treatments;
- intestinal inflammation such as Crohn's disease, diverticulitis, ulcerative colitis;
- pathologies that prevent the formation of blood clots.
Treatment methods
If intestinal ischemia is suspected, antibiotics must be prescribed to prevent infection and peritonitis, and drugs that dilate blood vessels.
Treatment of local inflammatory process of the intestine is provided.
If narrowing of the arterial beds is possible due to taking medications, then they are canceled.
When coagulability increases, antiplatelet agents and anticoagulants are prescribed to reduce thrombus formation.
If necrotic areas of the intestine are identified, they must be removed and the ends sutured. If this is not possible, a colostomy is formed with an opening on the skin of the abdomen. The patient will need to wear a colostomy bag.
At the same time, angioplasty of the narrowed artery is performed by inserting a balloon with a stent. Such an operation can be performed immediately after angiography.
For chronic ischemia, surgical treatment consists of creating an artificial vessel to bypass the thrombosed one.
If compression is caused by mechanical tumor growth, strangulation of a hernia, or adhesive obstruction, then the success of restoring arterial patency depends on the timely removal of these obstacles.
Diagnosis
Many signs and symptoms associated with AMI also occur with other intra-abdominal pathologies, such as pancreatitis, acute diverticulitis, acute intestinal obstruction, and acute cholecystitis. In general, patients with SMA embolism or thrombosis have an acute onset of the disease, rapid development of symptoms, and rapid deterioration of the condition, while with MVT and NMI the clinical picture develops more smoothly. With SMA embolism, the increase in symptoms occurs at lightning speed due to the lack of collateral blood supply and manifests itself in the form of severe abdominal pain, nausea, vomiting and diarrhea. Dehydration, impaired consciousness, tachycardia, tachypnea and circulatory collapse are rapidly increasing. Laboratory data show metabolic acidosis, leukocytosis, blood concentration.
AMI can rapidly progress to intestinal infarction; timely diagnosis and treatment are of strategic importance [1, 9]. A high level of suspicion based on history and initial examination data serves as the cornerstone in the diagnosis of acute intestinal ischemia. When diagnosis is made on the first day, survival rate is 50%, and when it is delayed it drops to 30% or lower. Laboratory studies often show hemoconcentration, leukocytosis, and metabolic acidosis. High levels of amylase, aminotransferase, lactate dehydrogenase, and creatinine phosphokinase are often found in test results, but they are not sensitive or specific for diagnosis. Hyperphosphatemia and hyperkalemia occur later and often accompany intestinal infarction.
Radiation examination of the abdominal cavity is also nonspecific. In the initial stage of the disease, 25% of patients may have normal radiological data. Characteristic radiographic changes, such as thickening or compaction of the intestinal wall, are less common than in 40% of patients. Air in the portal vein is a late symptom and is associated with a poor prognosis. At a high level of suspicion for AMI, CT is more likely to clarify specific details. Some authors report a sensitivity of 93.3% and a specificity of 95.9% for CT scans with IV contrast [3, 9].
Thickening of the intestinal wall, intramural hematoma, dilated and fluid-filled intestinal loops, congestion of the mesenteric vessels, pneumatosis, gas in the mesenteric and portal veins, infarction of other organs, arterial and venous thrombosis may be visible on CT scanning. The value of the study increases in the absence of indications for immediate laparotomy for suspected AMI. Early angiography increases the chances of survival.
Mesenteric angiography allows the differentiation of embolism and thrombotic arterial occlusion. An embolus most often occludes the middle colic artery, the first major branch of the SMA. Thrombotic disease most often affects the source of the SMA, and the vessel is not visualized at all. MVT is characterized by a generalized slowing of arterial blood flow. Usually the lesion is segmental in nature, in contrast to NMI, when normal venous outflow is preserved [3, 9].
Possible consequences
The most common are:
- necrosis of the intestinal wall - occurs when there is insufficient compensatory forces, dead tissue undergoes rupture and the contents enter the abdominal cavity, this causes severe peritonitis;
- narrowing of the intestine - let’s assume that as a result of a chronic process, scar tissue appears in small areas as a result of healing; it fuses with other loops of the intestine, with the mesentery.
Scars form a new mechanical obstruction due to narrowing of the intestine
Treatment
Once a diagnosis of AMI is made, treatment should begin immediately. With the exception of NMI, which requires drug therapy, most cases of AMI dictate the need for surgical intervention to restore intestinal blood flow.
The presence of symptoms of peritoneal irritation is more likely to indicate intestinal infarction than ischemia and requires immediate laparotomy. Even in the absence of intestinal necrosis, surgery is usually necessary to exclude irreversible changes in the intestinal wall. Resection of ischemic bowel is the most common surgical procedure for AMI. Satisfactory arterial pulsation, good blood supply to the remaining segment and the absence of peritonitis dictate the indications for primary anastomosis.
Intra-abdominal contamination, questionable blood supply to the preserved segment of the intestine and poor general condition of the patient are contraindications to the imposition of an interintestinal anastomosis. In this situation, removing both ends of the intestine is the safest procedure. In a small number of patients with the occlusive form of AMI, in the presence of reversible changes, an attempt at revascularization is possible. Embolectomy, thrombectomy, endarterectomy, or bypass may prevent bowel resection in the early stages of AMI. Massive extended gangrene of the intestine is not subject to surgical treatment, since it does not lead to an improvement in the patient’s condition [3, 9].
Preventive measures
To take good care of your vessels you need to:
- stick to vegetable dishes, cereals in the menu, eat salads and fruits every day;
- limit the consumption of spicy meat products, fatty and fried meat and fish, legumes, smoked meats, canned food;
- stop smoking;
- fight low mobility, walk more, play sports;
- control and prevent chronic diseases.
Timely consultation with a doctor and examination will help prevent severe ischemia. Acute abdominal pain should not be treated independently under the pretext of food poisoning. If they have not occurred for the first time, or there are other consequences of arterial damage (myocardial infarction, stroke), then one should remember about systemic vascular damage and take measures to prevent complications.
A nutritious diet is possible
The basic principle of a diet for intestinal diseases is the most complete diet with sufficient calorie content. Impaired digestion of food leads to a person sharply losing weight not only due to fat reserves, but also due to muscle mass. Therefore, the amount of complete protein in the menu should be increased to 130-140 g
and higher. It is also necessary to make meals in fractions: five to six meals a day can reduce the load on the digestive tract and improve the absorption of nutrients.
Authorized Products
Diet No. 3 for constipation is aimed at increasing the proportion of foods that enhance colon motility, namely:
- containing organic acids in large quantities: sauerkraut, citrus fruits, fruit drinks from sour berries and fruits, fermented milk drinks;
- with a high content of plant fiber: dried fruits, bran, cereals, wholemeal bread, raw vegetables (spinach, cabbage, radishes, carrots, etc.);
- cold first courses and desserts: okroshka, beetroot soup, ice cream;
- stringy lean meat: veal, rabbit, turkey, beef;
- lean fish: hake, cod, as well as any seafood;
- compotes, weak tea, chicory, rosehip decoction, natural juices.
The diet includes the inclusion in the diet of products with a laxative effect, as well as those that stimulate intestinal motility, such as honey, grapes, sweet apples, peaches, pumpkin, dates. Softening stool is facilitated by eating foods that swell in the digestive tract and facilitate the process of bowel movement.
Dietary fiber contained in cereals, vegetables and fruits is not digested. They absorb toxins and other harmful substances and activate peristalsis. Organic acids inhibit the growth of pathogenic microflora, increase the contractility of the intestinal muscles and normalize stool.
Diet No. 3 involves eating beets, cucumbers, tomatoes, zucchini, cauliflower, and broccoli. For constipation, it is allowed to add green peas and white cabbage to the diet. It is advisable to include fresh cottage cheese, sour cream, as well as fermented milk drinks in the five-day or seven-day menu: yogurt, kumiss, fermented baked milk or drinking yogurt.
If you have problems with bowel movements, you need to eat more berries and fruits containing plant fiber and sugar. For example, nectarines, apricots, plums, melons, watermelons. It is allowed to eat mild cheeses, scrambled eggs, and cream. For sweets, it is better to choose marshmallows, marmalade, jelly, and marshmallows.
You can and should add parsley, dill, cilantro and other greens to your food. Food must be cooked in vegetable or butter. Table No. 3 is quite diverse.