- home
- Treatment of cancer (oncology)
- Cancer metastases
- Intestinal metastases
—
—
—
Metastases in the intestine indicate that the disease is in the later stages, when the cells of the primary lesion move through the lymphatic or blood vessels to other organs and grow into new tumors - metastasize. Treatment can slow down the process, reduce symptoms and prolong the patient’s life.
Hospitalization of cancer patients. Daily. Around the clock
9,500 patients trust us annually.
Call me back!
Typically, neoplasms of the digestive tract are primary, while metastases from intestinal cancer grow in the liver most often, also in the lungs and bone tissue. The risks are increased by poor nutrition, an abundance of meat, processed foods and sausages, refined foods, a lack of vegetables and, accordingly, fiber, as well as heredity and chronic diseases.
How long does it take for bowel cancer to develop?
Colon cancer develops quite slowly. Most often it is a consequence of the malignant transformation of benign adenomatous polyps - neoplasms of the intestinal mucosa. It can take 10-15 years from the moment a polyp forms until it becomes malignant. Subsequently, the clinical course and rate of cancer progression depend on many factors:
- Histological tumor type
- Degree of tumor differentiation
- Type of tumor growth (superficial or invasive) – determines when bowel cancer will metastasize
- Activity of antitumor immunity and the presence of concomitant pathologies
To the greatest extent, it is the degree of differentiation of the tissues from which the tumor is formed that determines how long intestinal cancer develops. Poorly differentiated tumors grow faster than moderately differentiated ones. The best prognosis is for highly differentiated neoplasms that have maximum histological similarity to normal intestinal tissues.
To prevent intestinal cancer, it is important to undergo preventive examinations even in the absence of complaints. This will allow us to identify and remove adenomatous polyps at the stage of their benign growth. It is important for some people to have a colonoscopy (endoscopic examination of the bowel) annually: people with Crohn's disease and ulcerative colitis, and people with a family history of colon cancer. In general, preventive colonoscopy is indicated for all people over 40 years of age, once every 5 years.
Reasons and background
Colorectal cancer can be caused by a variety of factors, from behavioral to hereditary. By far the first place among the reasons belongs to eating habits. All lovers of meat, smoked meats, baked goods, and sweets are at risk. The development of the disease is associated not so much with the consumption of specific foods, but with the fact that people who prefer unhealthy food consume too little plant fiber. As a result, the functional load on the intestines is reduced.
In addition, the development of the disease is promoted by:
- hereditary factors;
- the presence of chronic inflammatory diseases of the gastrointestinal tract;
- advanced age;
- the presence of benign neoplasms in the intestines (polyps).
Colon cancer is considered a polyetiological disease. The list of reasons may be updated as medicine develops.
Prevention of the disease is simple: maintaining a healthy lifestyle, giving up bad habits, monitoring your diet and regular preventive examinations.
Classification of colon cancer
Oncologists have a large number of classifications of malignant intestinal tumors. The most commonly used in clinical practice are:
- TNM classification (determines the stage of the disease)
- Histological classification
- Types of cancer by anatomical location
- Types of cancer according to the degree of tissue differentiation
The growth pattern of intestinal cancer is also determined. It can be endophytic, exophytic or mixed. Endophytic growth is when a tumor grows inside the wall of an organ. It is characterized by a more unfavorable course because it grows faster into neighboring organs, the peritoneum and visceral tissue, and also metastasizes earlier. Exophytic growth is when the neoplasm grows towards the intestinal cavity. The exophytic type of growth is considered more favorable, since to completely remove the tumor it is often enough to excise its “vascular pedicle”.
According to histological classification, intestinal cancer is of the following types:
- Adenocarcinoma (95% of all neoplasms)
- Carcinoid tumors
- Stromal tumors
- Lymphomas
How long colon cancer lasts largely depends on the histotype of the tumor. Adenocarcinoma may be mucoid. Then it has a worse prognosis, since intestinal cancer develops quickly and in this case is less treatable. These types of tumors are divided into mucoid, mucoid and colloid. There are also signet ring cell and mucocellular cancers. The histological type is determined by biopsy. It influences the choice of treatment tactics for the disease.
A biopsy can be a stand-alone medical procedure or part of surgery to remove an intestinal tumor. In the first case, the doctor excises part of the tumor during an endoscopic examination and transfers the material to laboratory technicians for staining and immunohistochemical examination. In the second case, laboratory testing is carried out after complete removal of the tumor. Its results (detection of atypical cells or confirmation of the benign nature of the polyp) determine the tactics of further treatment.
Cancer is classified according to location:
- Sigmoid colon - in half of all cases
- Cecum – 20% of cases
- Appendix
- Ascending, descending or transverse colon
- Hepatic or splenic flexure of the colon
However, the most important from a clinical point of view remains the international TNM classification, where T stands for tumor, N stands for lymph node involvement, and M stands for distant metastases. Before moving on to a more detailed discussion of classification, let's understand how and where intestinal cancer metastasizes.
Causes of small intestine cancer
Small intestinal cancer grows and fills the intestinal lumen.
The origin of cancer cells is still unclear. However, it has been proven that there are some circumstances that can trigger the appearance of a malignant tumor.
In a large number of patients, the pathology in question developed as a result of chronic diseases of the gastrointestinal tract, as well as inflammatory processes that were localized in different parts of the small intestine.
Cancer may develop due to:
- duodenitis;
- celiac disease;
- colitis;
- enteritis;
- ulcerative lesions of the gastrointestinal tract;
- hereditary anomalies;
- Crohn's disease;
- benign tumors in the intestines;
- Peutz-Jeghers syndrome;
- metastasis of malignant neoplasms of other internal organs.
Among the factors that can provoke the occurrence of cancer cells are:
- abuse of fatty, fried foods, smoked foods;
- long-term alcohol consumption, smoking;
- exposure to radioactive radiation on the body.
A malignant tumor most often forms in the tissues of the duodenum, since this section of the small intestine is the initial one and begins to be the first to come into contact with carcinogens that are present in the food consumed.
Where do metastases go in colon cancer?
Metastases are “daughter tumors.” They are formed due to the fact that neoplasm cells spread throughout the body in various ways. Colon cancer with metastases has a much worse prognosis than without them. Daughter tumors appear in the later stages of the disease. Initially, regional metastases of colon cancer form in nearby lymph nodes, in the peritoneum and in visceral fat. Subsequently, distant metastatic foci appear.
Metastases in intestinal cancer have certain characteristics. There are three types of metastasis:
- Lymphogenic – through lymphatic vessels
- Hematogenous - through the blood
- Implantation (contact) – when metastases of intestinal cancer spread across the surface of the peritoneum and abdominal organs
Colon cancer metastases in the liver
Liver metastases in colon cancer are detected in 20–25% of cases during the initial examination and in 40% of cases after surgical treatment of the primary tumor. In this case, symptoms such as jaundice, itching, abdominal enlargement, pain under the right rib, and swelling may occur due to impaired synthesis of albumin proteins , which provide oncotic pressure of the blood plasma.
Treatment of liver metastases in colorectal cancer
Over the past decades, considerable progress has been made in the treatment of liver metastases in colon cancer. The indications for liver resection have expanded: if the tumor is relatively small and does not grow into the vessels, it can be removed. If metastatic lesions cannot be removed surgically, or they have recurred, in some cases they resort to radiofrequency ablation - abbreviated as RFA. Under ultrasound or CT control, a special electrode in the form of a needle is inserted into the node and the tumor tissue is destroyed using high-frequency current. RFA is possible if certain conditions are met:
- The secondary lesion should have a small diameter.
- It should be clearly visible during ultrasound and CT.
- The lesion should be located so that there is no risk of damaging a blood vessel during needle insertion.
- It is desirable that there be no more than 4 lesions.
They resort to chemotherapy - it is prescribed as an addition to surgery, or, if the latter is not possible, as an independent method of treatment. Chemotherapy drugs can be administered not only systemically (intravenously), but also directly into the vessel feeding the tumor, using a catheter passed through the femoral artery through a puncture in the upper thigh. During chemoembolization, not only a chemotherapy drug is injected into the vessel feeding the tumor, but also an embolizing drug - microspheres that block the lumen of the vessel and deprive the tumor tissue of blood flow.
In some cases, a modern technology called CyberKnife . A special apparatus generates many beams of X-ray waves. Each of them individually is weak and cannot harm tissues, but together they converge at one point - where the tumor is located, and a very high dose is created here. It destroys cancer cells.
In combination with chemotherapy drugs or on their own, targeted drugs - antitumor drugs that block molecules that activate the proliferation of cancer cells and the growth of new blood vessels that supply the tumor with necessary substances and oxygen. For intestinal cancer that has metastasized to the liver, targeted drugs are used: cetuximab, panitumumab, aflibercept, bevacizumab, regorafenib.
Where does colon cancer metastasize via the lymphogenous route?
The lymphogenic pathway is implemented first. This usually occurs in stage 3 bowel cancer. The order of appearance of metastatic tumors is determined by the course of the lymphatic vessels and the location of the regional lymph nodes relative to the tumor.
Typically, the sequence in which colon cancer metastasizes is as follows:
- Epicolic (supra-intestinal) and paracolic (peri-intestinal) lymph nodes
- Mesenteric or intermediate lymph nodes
- Lymph nodes at the root of the mesentery of the large intestine, as well as para-aortic (located near the abdominal aorta) lymph nodes
Subsequently, metastases spread through the lymphatic route, entering the lymphatic cistern. It is located at the level of 1-2 lumbar vertebrae. Tumor cells flow through the lymphatic duct into the venous system. They also penetrate the supraclavicular lymph nodes.
Diagnosis
Early detection of the disease is the key to successful treatment. In order to timely identify metastases in the intestines, doctors prescribe the following procedures.
1. Examination of stool to detect blood and mucus impurities. 2. Rectal examination of the lower intestinal sections. 3. Sigmoidoscopy - examination of the large intestine at a depth of 30 cm. 4. Sigmoidoscopy - a technique that allows you to examine the intestine at a depth of half a meter. 5. Colonoscopy - a procedure that allows you to examine the entire intestine: a tube is inserted through the anus, which penetrates into the intestine and detects a cancer focus or metastases there (if any). 6. Biopsies are procedures in which a piece of intestine is removed for analysis. This particle is studied under a microscope. 7. Computed tomography.
Invasive method of metastasis
Another way for metastases to spread is tumor growth into the abdominal cavity. It gradually increases in size. In later stages, the tumor spreads from the intestine to the peritoneum. Fragments of the tumor break off and spread to other organs.
The invasive method of metastasis leads to the development of peritoneal carcinomatosis - secondary involvement in the cancer process of the membrane lining the inner surface of the abdominal cavity and the surface of the internal organs. The peritoneum can also be affected by the spread of atypical cells through its blood and lymphatic vessels. At stage 1 of the process, doctors detect no more than 1-2 nodes measuring up to 5 mm. At stage 2, multiple malignant foci appear on the peritoneum, and at stage 3 they merge and cover most of the surface of the peritoneum.
Detection of peritoneal carcinomatosis requires correction of the treatment protocol, in particular, the HIPEC procedure, which we will consider below.
Send a request for treatment
Symptoms of intestinal cancer
The main danger of intestinal metastases is that the main symptoms are not specific. They are inherent in many diseases of the abdominal cavity. However, there are a number of conditions under which the doctor may order an examination that can detect a metastatic process.
1. First of all, the cancer patient will clearly show signs of the main tumor.
2. An obligatory part of such a pathology is the presence of severe pain. This pain occurs due to damage to the outer intestinal lining, in which nerve fibers are present in abundance.
3. Intestinal patency is impaired (this defect occurs if metastases severely block the intestinal lumen). In this situation, patients may suffer from nausea and vomiting that appears after every meal. Due to poor digestion of food, loss of body weight is observed.
Stages of bowel cancer
The stage of bowel cancer is determined based on three criteria:
- Tumor size
- Presence of regional metastases (damage to lymph nodes)
- Presence of distant metastases
Stage 0 . This is carcinoma in situ or carcinoma in situ. The most favorable stage of oncology with the best prognosis for recovery. There are no metastases of any localization. The tumor does not even spread beyond the intestinal mucosa. Typically, carcinoma in situ is a colon polyp in the early stages of malignant transformation.
Stage 1 . The cancer has already spread beyond the mucous membrane - to the submucosa or into the muscle layer. There are no metastases yet. The tumor is clearly demarcated from healthy tissue.
Stage 2A . The neoplasm grows through all layers of the intestine, but it does not spread to neighboring organs. There are no metastases.
Stage 2B . The tumor has already spread beyond the intestinal wall. But it has not yet metastasized and has not spread to neighboring organs.
Stage 2C . The tumor has grown through all the walls of the intestine, has spread beyond its boundaries, and infiltration of neighboring tissues is already observed. But at stage 2 of intestinal cancer there are no metastases yet.
Stage 3A . Patients often ask at what stage of colon cancer metastases appear. They appear precisely at the third stage. In this case, only local metastases are present in nearby lymph nodes; they are not yet present in distant organs. With grade 3A, the neoplasm grows into the submucosa of the intestinal wall and metastasizes to 4-6 nearby lymph nodes. Or it grows through the entire intestine and affects 1 to 3 lymph nodes. Infiltration of paraorgan fatty tissue is also possible.
Stage 3B . Stage 3 bowel cancer, namely 3B, is diagnosed in one of the following three cases:
- Cancer grows through all layers of the intestine and spreads to the peritoneum, but does not reach the internal organs. The tumor grows into the fatty tissue and affects 4-6 neighboring lymph nodes.
- The neoplasm grows into the muscular layer or through all layers of the intestine and spreads to 4-6 neighboring lymph nodes.
- The tumor penetrates the submucosal layer or the muscular layer of the intestine, and also spreads to 7 or more nearby lymph nodes.
Stage 3C . This diagnosis is made in the following cases:
- Cancer grows through all layers of the intestinal wall, spreads to the visceral layer of the peritoneum (covering the internal organs), but does not grow into the organs themselves, and also spreads to 4-6 nearby lymph nodes.
- The neoplasm grows through all layers of the intestinal wall, and also spreads to 7 or more lymph nodes.
- The tumor has grown through all layers of the intestinal wall, spread to the fatty tissue and at least 1 lymph node.
There are no distant metastases (that is, metastases outside the abdominal cavity) in stage 3 colon cancer. They appear only in the last stage of bowel cancer.
Stage 4A . The presence of metastases characterizes stage 4 colon cancer. It is also divided into three subtypes. Stage 4 colon cancer, subtype A, is characterized by tumor invasion of all layers of the intestine. At least 1 distant metastasis is present (liver or lungs, as well as distant lymph nodes). In this case, regional metastases may be absent.
Stage 4B . The tumor completely or partially invades the intestinal wall. Regional metastases may or may not be present. In this case, there is at least 1 distant metastasis in the internal organs or several distant metastases in the lymph nodes.
Stage 4C . Stage 4 colon cancer, subtype C, is characterized by complete invasion of the organ wall, the presence of local metastases and the spread of the tumor to distant areas of the peritoneum. There may be no distant oncological foci in this subtype of stage 4 colon cancer with metastases.
The most common metastases found in intestinal cancer are liver metastases. They are observed in 50% of patients with this disease. This is caused by late diagnosis of oncological pathology, which is usually detected quite late - at stages 3 or 4.
What are the symptoms of colon cancer with metastases?
Manifestations depend on the organ in which the secondary lesions are located and how much they disrupt their function. But there are some common symptoms:
- Poor health, constant weakness, malaise, increased fatigue.
- Loss of appetite.
- Unexplained weight loss, up to severe exhaustion, cachexia .
There may be no symptoms at all. In this case, metastases are detected only during examination.
Examination for accurate staging of bowel cancer
Staging bowel cancer is not just another line in the diagnosis. This is the basis for the future treatment regimen, which will be developed by an interdisciplinary council of oncologists, surgeons and gastroenterologists. The accuracy of determining the stage of oncological pathology determines how successful the therapy will be and which methods will be most preferable.
As already indicated in the description above, the main factors that determine the stage and preferred treatment regimen are:
- Tumor size
- Localization of the tumor, its growth into the intestinal wall and spread to neighboring organs
- Tumor invasion of major blood vessels
- The presence of metastases in the lymph nodes
- Presence of distant metastases
- Histological type of tumor (in some cases it is established only after surgery, based on the results of examination of removed tissues)
To accurately assess these factors, patients undergo laboratory and imaging tests, including:
- Coprogram and fecal occult blood test. This is the primary test that allows you to suspect bowel cancer, since tumor-related bleeding is the earliest sign of pathology. Blood may not be visible to the naked eye, so it is important to take a stool occult blood test.
- Ultrasound of the abdominal organs (abdominal, endorectal). Ultrasound allows the doctor to see fairly large tumors and/or metastases.
- Endoscopic examination of the large and small intestine. Rectoscopy, flexible sigmoidoscopy and colonoscopy allow the doctor to see the inner surface of the intestine, in particular, to identify neoplasms - benign polyps and tumors.
- CT colonography, or “virtual colonoscopy,” is primarily indicated for people who, for whatever reason, cannot undergo a regular colonoscopy. During a CT colonography, the intestine is filled with gas (for better visualization), after which the doctor takes CT images from different angles.
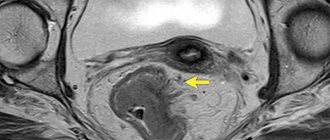
- CT/MRI of the abdominal cavity, and if metastasis is suspected, of the whole body.
- Biopsy with histological examination, most often as one of the stages of endoscopic examination. This type of biopsy is the least traumatic because it does not require incisions within healthy tissue. Small polyps or carcinomas in situ can be completely removed in this way.
- Angiography (examination of blood vessels). Angiography is primarily indicated for patients with colon cancer metastasis to the liver. Visualization of tumor vessels helps to plan surgical treatment of liver metastases or their chemoembolization.
The list of mandatory examinations also includes:
- Clinical blood test (to exclude anemia and active inflammatory process)
- Biochemical blood test with assessment of liver and kidney function, blood test for glucose
- Coagulogram (to exclude blood clotting disorders)
- Blood test for tumor markers
- Electrocardiogram (to rule out serious heart problems)
If there are significant concomitant pathologies, general practitioners and the necessary specialized specialists (cardiologists, neurologists and others) are involved in the development of a treatment regimen.
Intestinal oncology and liver metastases
In intestinal oncology, the liver is most often affected by metastases. This is due to its physiological characteristics. Since the liver is responsible for filtering the blood, all blood mass passes through it. Along with infected blood, metastases also enter the liver. As a result of the lesion, the functioning of this organ is disrupted. After a certain time, in addition to liver problems, other complications appear. In particular, there may be compression of important veins, which leads to obstructive jaundice, which complicates the treatment of cancer pathology.
Clinics and treatment costs
When choosing a clinic for the treatment of intestinal cancer, you should focus, first of all, on its technical capabilities and the experience of doctors (oncologists, surgeons, gastroenterologists). The clinic should use modern diagnostic equipment for accurate cancer staging; all types of operations and modern medications should be available here.
Among the medical institutions that specialize in the treatment of intestinal cancer, it is worth noting:
- University Hospital Dusseldorf, Department of Gastroenterology, Hepatology and Infectology
- University Hospital of the University of Munich. Ludwig Maximilian, Department of Gastroenterology and Hepatology
- University Hospital Ulm, Department of Gastroenterology and Hepatology
- University Clinic named after. Goethe Frankfurt am Main, Department of Gastroenterology, Hepatology, Pulmonology, Allergology, Endocrinology and Diabetology
- University Hospital Würzburg, Department of Gastroenterology, Hematology, Oncology, Hepatology, Infectology, Rheumatology and Clinical Immunology
The cost of treatment for intestinal cancer depends, first of all, on the stage of the oncology and the therapeutic method and is determined individually in each case. Average prices for treatment of intestinal cancer in specialized centers and multidisciplinary university clinics are:
- Laparoscopic resection of intestinal tumor – €18,920
- Resection of intestinal tumor using the da Vinci robot – €32,320
- Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (HIPEC) for colon cancer, including treatment of stage 4 colon cancer with metastases – €51,520
- Treatment of colon cancer with chemotherapy – €7,030
- Treatment of colon cancer using embolization or chemoembolization – €31,620
- Rehabilitation after completion of the main course of treatment – €1,196 per day
The treatment program can be supplemented or adjusted after receiving the examination results. In this case, its value changes. Doctors also recommend spending several weeks of rehabilitation after completing the main course of treatment, since operations and medications often temporarily worsen the patient’s general condition. Rehabilitation is carried out in specialized centers, under the supervision of medical specialists and nursing staff.
Send a request for treatment
Elimination of intestinal metastases
There are often situations in which surgical intervention is ineffective. In such situations, treatment is carried out using a chemotherapy course. Thanks to this approach, it is possible to eliminate pain, reduce the severity of symptoms, improve the patient’s quality of life and prolong it. However, the exact treatment tactics are developed on an individual basis. Here everything depends on the stage of the pathology, the metastatic nature of the cancer focus, as well as a number of other factors. As a rule, the treatment process takes a long time; it is stopped (and then temporarily) only after achieving certain positive results.
Diagnosis and treatment of cancer in Germany
Cancer can be detected at an early stage if diagnosed early. Indeed, in most cases it does not develop “out of nothing.” There are many precancerous diseases that can be detected and treated in a timely manner, preventing malignancy. Or carry out periodic monitoring, which will allow timely detection and removal of the tumor even before the appearance of metastases.
The most common background precancerous diseases of various parts of the intestine:
- Crohn's disease
- Chronic inflammation of the large intestine
- Nonspecific ulcerative colitis (UC)
- Intestinal diverticula
- Polyposis
Polyps can be multiple or single. Singles are more dangerous. In 40-50% of cases, they sooner or later degenerate into cancer.
In Western countries, colon cancer is most common. Therefore, doctors in countries such as Germany have the most experience in treating such pathologies and have achieved the highest success in this. Medicine is well developed in this country. Therefore, this is where you can go to get qualified and high-tech medical care.
To organize examination and treatment in Germany, please contact ]Booking Health[/anchor] for help. We will help you:
- Find a suitable clinic and doctor. This could be a small specialized cancer center or a large university clinic.
- Select the optimal treatment program, including treatment of stage 4 colon cancer with metastases. At the same time, we take into account the results of existing examinations; you do not have to repeat a fresh MRI or biopsy.
- Make an appointment or reserve a place in a hospital.
- Resolve all organizational issues with the administration of the selected clinic.
- Control the cost of medical procedures, eliminate surcharges for foreign patients and overpayments, and thus save up to 50% of the original cost of treatment.
- Monitor examination, treatment and rehabilitation at all stages.
- Obtain insurance that covers additional costs in the event of treatment complications.
- Organize flights and accommodation for the patient and accompanying person, help with the translation of documents and accompanying the translator in the clinic.
We will reduce the waiting time for treatment, which is very important in the case of bowel cancer. After all, this disease develops quickly, and the longer you do not receive medical help, the greater the risk that the tumor will metastasize.
You will also receive a full package of services. We will help with the paperwork, provide an interpreter, meet you at the airport and take you to the clinic by car. Your personal coordinator will be in constant contact with you while you are abroad, and you will also be able to contact him with any questions within 3 months after completion of treatment.
Thanks to ]Booking Health[/anchor] you can completely focus on your health, avoiding the need to resolve organizational issues.
Classification
According to the nature of development, small intestinal cancer is divided into:
- Exophytic - malignant neoplasms of this type of disease provoke a narrowing of the intestinal lumen and the appearance of its obstruction. Similar in appearance to cauliflower or polyp.
- Endophytic - this form of pathology is accompanied by intestinal bleeding, perforation, peritonitis. Endophytic cancer infiltrates into the walls of the small intestine.
The histological structure of a malignant tumor is divided into:
- Adenocarcinoma - occurs more often than others, can affect any intestinal section, with subsequent penetration into nearby internal organs and tissues. Often formed in Crohn's disease.
- Kaposi's sarcoma - can sometimes be combined with other intestinal diseases. Such a tumor can occur in any area of the gastrointestinal tract. The course of this pathology can be either asymptomatic or with pronounced signs of cancer development.
- Carcinoid - in fifty percent of cases, numerous neoplasms are observed. It originates in the appendix, but often infects neighboring organs (mainly the liver). The clinical picture is vivid: intestinal obstruction, severe pain, and bleeding occur.
- Primary lymphoma - promotes damage to the ileum. In most cases, it is observed in patients who are gluten intolerant. At the initial stage, small bowel cancer usually affects the jejunum and ileum.
Modern principles of colorectal cancer diagnosis
Timely detection of colorectal cancer involves diagnosing it in the early, preclinical stages, when there are no clinical manifestations of this disease.
Diagnosis, or early detection of colorectal cancer, is carried out using digital examination, hemoccult test and endoscopic method.
Digital examination of the rectum can detect up to 70% of rectal carcinomas. The basis for performing a hemoccult test is that colorectal adenomas and carcinomas bleed to varying degrees. When screening among a formally healthy population, from 2 to 6% of those examined have a positive hemoccult test. Upon further examination of patients who have a positive hemoccult test, colorectal cancer is detected in 5–10% of cases, and glandular adenomas in 20–40% of cases.
In 50–70% of cases the test is false positive.
Sigmoidoscopy and total colonoscopy are important components of colorectal cancer screening. Using modern flexible sigmoidoscopes 60 cm long, it is possible to detect 55% of adenomas and carcinomas of the sigmoid and rectum that develop de novo. The sensitivity of this method is 85%. (The American Medical Association currently recommends sigmoidoscopy every 3 to 5 years, starting at age 50, in individuals who do not have any complaints of bowel dysfunction).