About colonoscopy and possible consequences
Colonoscopy is an endoscopic diagnostic method. Allows you to examine the inner surface of the colon and make an accurate diagnosis. Sometimes, simultaneously with the detection of pathology, it is possible to eliminate it, for example, by removing a small polyp or foreign body.
Researcher Subbotin calls colonoscopy “the gold standard for diagnosing diseases of the large intestine” (Subbotin A.M., 2010, p. 1754). Other authors and medical practitioners agree with him. Modern equipment opens up wide opportunities for high-precision diagnostics, allowing timely detection of diseases, areas of inflammation and changes in the mucous membranes. However, at the same time, colonoscopy involves a certain intervention in the digestive system, requires careful preparation, and therefore is not without certain risks.
Typically, relatively severe complications are associated with emergency colonoscopy. This is due to the person’s lack of opportunity to prepare thoroughly, as well as the general serious condition of the patient. That is why the diagnostic procedure is often performed as planned.
However, a planned colonoscopy does not guarantee the absence of complications. Among the most common are disorders of the gastrointestinal tract that persist for some time. Constipation as a consequence of colonoscopy, which occurs after the examination, may be associated with both the preparation and the procedure itself.
In addition, there are certain indications for diagnostics: diseases of the gastrointestinal tract, which themselves cause constipation, or suspicions of them. In this case, the problem does not disappear after a colonoscopy.
Preparation for the procedure involves cleansing the intestines using osmotic laxatives. They provide the conditions necessary for examination, but their use, as well as the need for prolonged fasting, can cause disturbances in intestinal function. These disturbances persist for several days after the procedure. In addition, in the vast majority of cases, diagnosis is carried out under anesthesia, usually short-term, which can lead to impaired intestinal muscle tone and stool retention in the first time after the examination.
Mild consequences also include pneumatosis intestinalis, a condition in which air cysts form on the surface of the mucosa. Shaikhiev in his work points out that “pneumatosis of the colon is associated with inadequate evacuation of air from the intestinal lumen at the end of the study. This condition resolves on its own within the next hour” (Shaikhiev Zh. Zh., 2011, p. 29).
Get rid of intestinal problems
The natural British drug is not addictive and works immediately
Find Fitomucil with benefits
Relative contraindications
The list of relative contraindications to FCS is presented below:
- acute inflammatory diseases of the anorectal area (for example, exacerbation of hemorrhoids, anal fissures, paraproctitis, etc.);
- recovery after surgery on the pelvic and abdominal organs;
- hepatosplenomegaly;
- hydropericardium, hydrothorax;
- hemorrhagic vasculitis;
- tense ascites;
- severe bleeding disorders;
- pregnancy in the second and third trimesters.
In addition, menstrual days may be a relative contraindication to intestinal colonoscopy in women - during menstruation, sensitivity usually increases, so the procedure can cause increased discomfort.
Relative contraindications are a temporary limitation to performing FCS; in this case, the procedure is recommended to be postponed until the patient’s condition improves. However, if there are vital indications, emergency colonoscopy can be performed if its diagnostic value outweighs the significance of the risks.
Colonoscopy can also be postponed if bowel cleansing is poor - in this case, it is impossible to ensure the diagnostic accuracy of the procedure.
Preventing constipation after colonoscopy
Prevention of constipation after colonoscopy begins at the preparation stage. So, the doctor will prescribe a suitable laxative for complete cleansing and give recommendations regarding the use of other medications.
It is important to adhere to a special diet some time before the diagnostic procedure. This will help improve visualization of the inner surface of the intestine, eliminate the formation of large amounts of gas and reduce the likelihood of complications. Lack of thorough preparation may lead to the need to repeat the procedure, so you should not neglect preparation.
In order to prevent disturbances in bowel function after endoscopic intervention, it is important to adhere to the recommendations of a specialist. Your doctor may prescribe the following medications:
- analgesics for pain relief;
- defoamers, sorbents to eliminate increased gas formation: with low risks of developing constipation;
- laxatives;
- prebiotics to normalize intestinal microflora.
If there are no contraindications to moderate physical activity, it is important to move. Light exercise and walking are suitable. It is better to avoid heavy loads.
Compliance with the drinking regime is of great importance in the prevention of constipation in general and after colonoscopy in particular. It is important to drink up to 2 liters of water per day to ensure normal bowel function and normal stool consistency. If you take diuretics, ask your doctor how much fluid you need per day.
When determining the required volume of water, we need to take into account all the liquid that we consume per day: tea, soups, vegetables, fruits (they also contain water). But none of the above can completely replace water; it will only reduce the required volume.
After the intervention, it is important to adhere to a special diet. The principles of postoperative diets are suitable, but not with such strict restrictions. So, the daily menu should include cereals, lean meats and fish, and fermented milk products. You need to avoid smoked meats, marinades, spicy foods, fried and fatty foods, as well as ready-to-eat foods - sausages, confectionery, etc.
If constipation may occur due to a disease of the digestive system, seek your doctor's recommendations for prevention.
Diet for constipation after colonoscopy
Nutrition for constipation after colonoscopy is fundamental. A special diet will help normalize intestinal function and restore regular bowel movements.
Doctors highlight several key principles of nutrition after endoscopic interventions:
- Mechanical protection of mucous membranes and intestinal walls. This explains the need to avoid solid food particles. On the first day, it is important to eat pureed foods.
- Reducing gas formation. To eliminate pain associated with stretching of the intestinal walls, it is important to avoid foods that cause increased gas formation.
- Softening of feces. The condition is especially important for elderly patients. This is facilitated by a sufficient amount of fiber in the diet.
- Fractional meals. Portions should be smaller, and you should eat food more often - up to 6 times a day. Thanks to this, food will be better absorbed, and the load on the digestive system will be low.
- Individual approach. When compiling a diet, the individual characteristics and health status of a person are taken into account. Thus, even products approved for consumption if the patient is allergic to them are strictly excluded from the menu. The same applies to fermentopathy.
Allowed products include lean meats, fish, and poultry. Preference should be given to baked or boiled dishes. Steamed cutlets are allowed.
The diet may include steamed omelettes, mashed potatoes, day-old bread, mild cheeses, and cereals - buckwheat and oatmeal.
Salads made from fresh vegetables will provide the body with the necessary amount of plant fiber. You can add herbs to them - dill and parsley. Apples and pears are allowed as fruits. Curd puddings, mousses, sweet jelly, juices, and berries are suitable as desserts. You can drink rosehip decoction, green tea, chamomile decoction, still mineral water, regular drinking water.
The list of prohibited products includes the following:
- soda;
- strong tea and coffee;
- kvass;
- legumes;
- rice, semolina and pearl barley porridge;
- fried foods;
- sauces, including those with the addition of vinegar;
- fresh bakery;
- canned food, marinades;
- peppered dishes;
- grapes, grape juice;
- whole milk, cream;
- spicy types of cheese;
- mushrooms;
- spinach, turnip, horseradish, radish;
- semi-finished products, sausages.
The first food after the procedure should be liquid or puree. For dinner, porridge without butter or mashed potatoes is allowed. Already from the second day, you can restore a full diet, adhering to the rules of nutrition. It is necessary to follow such a diet even if you are feeling well. The doctor will tell you how long it will take to recover.
If a colonoscopy was performed in connection with already diagnosed diseases of the gastrointestinal tract, which required adherence to a certain diet, it is important to consult a doctor and find out whether additional restrictions are imposed.
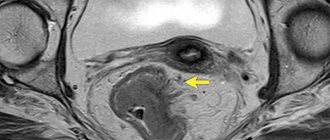
Why is there blood after a colonoscopy?
In the first few days after a colonoscopy, streaks of blood in the stool are a common occurrence that occurs in most patients. If its amount is small, the color is dark, and there are no other negative symptoms (abdominal pain, increased body temperature), then this is normal.
The admixture of blood appears as a result of damage to the intestinal mucosa as a result of exposure to the colonoscope. Another reason is to carry out manipulations, such as removing polyps and taking a biopsy. After them, small lesions remain on the intestinal mucosa, from which blood is released in small quantities for some time.
The intestinal mucosa is restored quite quickly. Therefore, after 2-3 days all the unpleasant consequences of the examination disappear. In some cases, the recovery process may take longer (up to 5-7 days). If bleeding continues after this time, you should consult a doctor and undergo additional diagnostics.
If there is excessive bleeding in the stool, a stomach ache, or other serious ailments occur after a colonoscopy, you should immediately consult a doctor. These symptoms may indicate the development of serious complications, such as intestinal perforation.
How to use fiber correctly
An adult should receive from 25 to 35 grams of fiber per day so that his gastrointestinal tract functions stably and predictably. This amount is quite difficult to obtain from diet alone, even if your diet includes vegetables and legumes - the main sources of dietary fiber. Therefore, you can choose an effective drug for yourself.
One of them is the English drug “Fitomucil Norm”. It does not contain preservatives, flavor enhancers or dyes. It contains only plant components:
- plantain seed shell (psyllium);
- dried home plum fruits.
“Fitomucil Norm” is packaged in portioned packages. The contents of the sachet should be mixed with a glass of liquid at room temperature and drunk. Drink a glass of water. In case of constipation, it is generally important to maintain a drinking regime: at least 1.5–2 liters per day. The product gently stimulates the intestines and does not cause pain or bloating. You will find detailed information about the drug on the website.
What are the complications after colonoscopy?
The incidence of complications after this study is relatively low. Most often they are not severe and go away over time even without special treatment. Such complications include:
- Bloating.
- Constipation or loose stools.
- Small amounts of blood and mucus in the stool.
They do not pose a threat to the patient’s health and life and disappear within 5-7 days after the examination.
More serious complications are much less common:
- Bowel perforation
. When the intestinal wall breaks, the patient notices sharp, acute abdominal pain, fever, bloating and tension in the abdominal muscles. - Massive intraintestinal bleeding
. Manifested by copious bleeding from the rectum, tachycardia, and decreased blood pressure. - Bacteremia
. It is characterized by a sharp increase in body temperature and a deterioration in general condition. - Intestinal obstruction
. Its development is indicated by prolonged stool retention, bloating, vomiting, and general weakness.
These conditions require urgent medical attention as they threaten the patient's life. Therefore, if any of the symptoms of such complications appear, you should immediately seek medical help.