Insufficiency (incontinence) of the sphincter is a complete or partial violation of voluntary retention of feces. An increasing number of people are encountering a similar phenomenon: there is an increase in requests from patients with both congenital and acquired disorders.
1
Treatment of sphincter incontinence in MedicCity
2 Treatment of sphincter incontinence in MedicCity
3 Treatment of sphincter incontinence in MedicCity
Sphincter incontinence is a very serious problem that can lead to disability. It is very difficult for a patient with this disease to be in a social environment, to work, to build relationships. However, many are still embarrassed to consult a proctologist with similar problems. In cases where the patient has partial or complete sphincter incontinence, plastic surgery is indicated. If you have any symptoms of proctological diseases, immediately consult a proctologist. At the MedicCity clinic, your problem will be solved highly professionally and as delicately as possible!
Anal sphincter. Structure
The anal sphincter is a circular muscle; it is the one that is most often in a contracted, compressed form and relaxes during bowel cleansing. A lot depends on its proper operation. For example, with normal functioning of the anal sphincter, a person can restrain the body’s urge to defecate if it happens at an inconvenient time and in an inappropriate place.
The primary task of the anal sphincter is the ability to control and promptly release waste intestinal contents. Sphincter incontinence is associated with an imbalance in the functioning of this organ, consisting of an internal and external part.
The external anal sphincter is a ring structure consisting of striated muscles surrounding the anal canal. Its length is 8-10 cm and its thickness is 2.5 cm. The striated muscles are connected to the puborectalis muscle. The anal sphincter muscles include the subcutaneous, superficial and deep muscles.
There are special receptors in the muscles of the external anal sphincter. Each of us can control the movement of stool and its consistency without any effort. The defecation reaction occurs as a result of a sharp increase in intra-abdominal pressure. This leads to intrarectal pressure and the internal anal sphincter relaxes.
We cannot coordinate the work of the internal anal sphincter at will. The anal sphincter contracts and relaxes as a result of irritation of the rectum by feces. The main function of the internal sphincter is regulatory; it helps to stop the uncontrolled movement of gases and liquid feces.
Rectal sphincteritis
The most common diseases of the rectal sphincter are: spasm and sphincteritis. In the first case, this is a chronic form of the disease, in which a person experiences constant pain and discomfort in the anal area. This disease develops over a long period of time and causes severe discomfort to the patient’s life. Therefore, it is recommended not to delay the treatment of this problem.
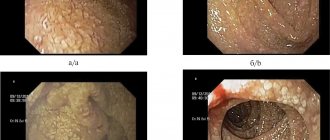
Sphincteritis is an inflammatory process in which its muscles become inflamed. This disease is characterized by wave-like exacerbation; treatment takes a long period of time. Below is a photo of rectal sphincteritis. Other factors that can trigger the development of inflammation of the sphincter muscles include:
- bacterial anal infections;
- disorders of the gastrointestinal tract;
- spicy food;
- tumor formations in the rectum;
- injury to the anus during anal sex;
- frequent spastic constipation (when hard-formed feces pass through the sphincter, the muscles of which are in good shape);
- intestinal disorders that cause severe irritation of the anal mucosa
Rectal sphincteritis is a very common disease. It occurs against the background of existing damage or diseases of the rectum. May have acute or chronic manifestations. In most cases, local treatment with medications is used and a strict diet is prescribed for the patient.
Signs of anal sphincter incontinence
There are 3 degrees of sphincter incontinence:
- gas incontinence;
- incontinence of gases and liquid feces;
- the absolute impossibility of retaining waste gaseous, liquid and solid contents by the sphincter.
Depending on the degree of anal sphincter incontinence or dysfunction, problems with incontinence of gaseous, liquid or solid contents of the colon may occur in the following cases:
- with sudden compression (including involuntary - during a sneeze, for example);
- during active movement;
- during sleep;
- in a sitting position;
- in any position.
Plastic surgery for sphincter incontinence is designed to eliminate these problems that poison the patient’s life.
Skinferitis symptoms
The manifestations of sphincteritis are similar, regardless of the reasons that caused it. The defining symptom is pain, which intensely increases during bowel movements. In addition, the pain can “radiate” to the perineum or neighboring organs. Over time, severe itching and constant burning in the anus are added to the pain.
In addition, sphincteritis is also accompanied by a painful false urge to defecate, which is called tenesmus. Also, a characteristic purulent coating or foaming mucus appears on the stool, and the urine takes on a dark tint. Often the patient notices blood in the stool in the form of streaks.
The onset of the inflammatory process also entails an increase in temperature to 38, which is fraught with severe general malaise (especially with cholangitis).
Often the patient complains of colic attacks, which in intensity resemble liver colic. After eating, the pain is localized under the right hypochondrium and intensifies. Nausea and vomiting may occur. If sphincteritis is accompanied by liver pathologies, jaundice periodically appears, which is also accompanied by severe itching, as well as a bitter taste in the mouth.
The acute course of the disease is distinguished by a vivid symptomatic picture, but with timely and correct treatment, the manifestations quickly stop. The chronic form has mild symptoms, but long-term treatment will be required.
Causes of anal sphincter incontinence
The most common cause of this phenomenon is the traumatic consequences of external influences, including operations on the anal cavity (for example, in the presence of a foreign body in the intestine).
In second place are the consequences of diseases affecting the central and peripheral nervous systems, colon infections and dysbacteriosis, leading to functional disorders of the rectal closure apparatus.
1 KARL STORZ Rectoscope
2 KARL STORZ Rectoscope
3 KARL STORZ Rectoscope
Congenital malformations of anorectal development should also be noted. Their number has increased in recent years due to the fact that modern medicine has learned to care for more premature babies than before.
In addition, injuries or functional disorders of the obturator apparatus of the rectum often occur during pregnancy and childbirth. This group of patients has also increased significantly due to the deterioration of general health statistics among pregnant and postpartum women.
A special place in the development of sphincter incontinence is played by such a disease of our time as hemorrhoids. This disease leads to constant stretching of the anal sphincter, especially with the development of hemorrhoids.
Notes
- Komarov F.I., Grebenev A.L.
Guide to gastroenterology. Volume 1, M.: 1995. - Sax F. F.
Morphological basis of the sphincters of the digestive tract // Physiology and pathology of the sphincter apparatus of the digestive system. - Tomsk. 1984. - Bordin D. S., Valitova E. R.
[gastroscan.ru/gerb/bord08.htm Methodology and clinical significance of esophageal manometry] / Ed. Doctor of Medicine, Prof. L. B. Lazebnik. - M.: Publishing House "MEDPRACTIKA-M", 2009, - 24 p. - Stendal Ch.
Practical Guide to Gastrointestinal Function Testing. Blackwell Science Ltd., 1997, 280 p. ISBN 0-632-04918-9. (English). - Website of the Department of Urology of Moscow State Medical University. [www.urogynecology.ru/index.php?option=com_content&task=view&id=25&Itemid=70 Urodynamic studies].
Diagnosis and treatment of sphincter incontinence
At the MedicCity clinic, highly qualified proctologists, using the latest equipment from the world's leading manufacturers (sigmoidoscope), will determine the degree and form of anal sphincter insufficiency and other disorders of the anal sphincter.
Depending on the results of the examination and the condition of the closure (obturator) apparatus of the rectum, a set of measures is drawn up to improve neuro-reflex functionality using therapeutic methods (diet, massage, electrical stimulation, medication).
This can be considered both as preoperative preparation and postoperative recovery.
In some cases, when the problem of colonic incontinence is associated with a functional disorder, conservative treatment is the main one.
If surgical intervention is necessary, which is usually caused by defects of the anal sphincter, plastic surgery is performed to correct the defects and have a cosmetic effect.
Literature
- Kolesnikov L. L.
Human sphincter apparatus. - St. Petersburg: SpetsLit, 2000. - 183 p. ISBN 5-263-00142-8. - Mayev I.V., Samsonov A.A.
Diseases of the duodenum. M.: MEDpress-inform, 2005—512 p. ISBN 5-98322-092-6
| : Incorrect or missing image | To improve this article it is desirable:
|
Diagnostic measures
Diagnosis begins with collecting the patient’s medical history, in which special attention is paid to chronic ailments of the gastrointestinal tract. A consultation with a proctologist will help identify violations of sphincter contraction (based on the results of a digital examination and/or rectoscopy).
However, it is almost impossible to prescribe effective treatment without first identifying the causes of the disease. Therefore, to make an accurate diagnosis, you will have to conduct some laboratory and instrumental tests and studies.
Complete blood count: an increase in the number of leukocytes, which indicates the development of inflammation.
Coprogram: fecal analysis will help detect blood streaks, the appearance of a purulent fraction, as well as any changes in bowel movements.
Duodenal intubation and duodenoscopy are necessary to assess the functioning of the liver and biliary tract.
Introduction
One of the rare causes of acute intestinal obstruction is intussusception of the small intestine. Intussusception is defined as the penetration of the distal part of the intestine in the proximal direction, while, along with the intestinal wall, compression of the mesentery simultaneously occurs between the internal and middle cylinders of the intussusception [3-5, 22]. This type of intestinal obstruction accounts for 15% of all cases of mechanical intestinal obstruction [7]. Intussusception of the small intestine after operations on the abdominal organs occurs in 1-5% of cases [11, 16, 20]. According to T. Pavlidis et al. [19], intussusception in adults over the past 12 years was diagnosed in 7 (1.9%) of 368 patients operated on for small bowel obstruction.
The mechanism of intussusception is not completely clear. Common causes of intussusception are polyps, circulatory disorders of certain parts of the intestine, primary and metastatic tumors of the small intestine, and Meckel’s diverticulum [1, 2, 20]. In some observations, it is not possible to establish the provoking cause of peristaltic disturbances; it can be difficult to find the trigger that led to intussusception. In this case, it is possible to talk about “primary intussusception,” which occurs in 8-20% of all cases of intussusception [13, 15].
Another reason for the development of intussusception may be small intestinal obstruction due to adhesive disease of the abdominal cavity, when there is a mechanical obstruction with compression of the intestinal lumen. In this case, increased peristalsis occurs in the proximal small intestine, which leads to intussusception in the aboral direction [10].
The clinical picture of intussusception corresponds to that of intestinal obstruction. In patients with adhesive disease of the abdominal cavity and after repeated surgical interventions, diagnosis is extremely difficult; the diagnosis is often made on the operating table. The classic triad (cramping pain, stool with blood “raspberry jelly” and a palpable tumor - intussusception), described in the clinical picture of intussusception in children, practically does not occur in adults [13, 18].
Diagnosis of intussusception according to X-ray, ultrasound, and multislice computed tomography (MSCT) is based on identifying signs of high or low (distal or proximal) small bowel obstruction in combination with typical signs of intussusception [6, 12, 14, 15, 19, 21]. It should be noted that echographic examination of the abdominal organs and MSCT are methods of equivalent sensitivity [13-16]. On ultrasound, signs of intussusception are a “hyperechoic center”; weak or absent concentricity of layers in the intestinal conglomerate; vagueness, blurring of the contour and the presence of fluid between the cylinders of the intussusception, which are direct ultrasound signs of pronounced circulatory disorders in the wall of the strangulated intestine. The maximum accuracy of the study was established when identifying the symptoms of “target” (100%), “pseudorenal” (98.9%), and “forceps” (68.8%). All of these signs have high specificity and sensitivity [6, 14, 15].
MSCT also makes it possible to assess circulatory disorders inside the intussusception with determination of blood flow in the mesentery segment compressed between the intestinal walls [6, 12, 14].
The operation of choice for secondary intussusceptions is disinvagination (if possible), assessment of the viability of the intestinal segment and adhesiolysis [8, 9, 15, 17, 21].
We present 2 clinical examples of small intestinal intussusception in the early postoperative period in adult patients.
Patient L.
, 72 years old, was admitted 6 hours after the onset of the disease with complaints of cramping pain in the lower left abdomen, nausea, repeated vomiting, delayed passage of stool and gas, and general weakness.
History: in 2012 - panhysterectomy for an ovarian tumor, 2013 - nephrectomy for a kidney tumor. After the last operation in the early postoperative period, the patient experienced an episode of adhesive intestinal obstruction, and conservative treatment was performed.
Upon examination in the emergency department, the patient's condition was moderate. The tongue is moist, covered with a whitish coating. The abdomen is swollen, soft, painful on palpation in the mesogastric and hypogastric region, more on the left. There are no peritoneal symptoms. The sound of splashing is detected. Peristalsis is audible and sluggish. After the cleansing enema, there was a small amount of stool, and some gases passed. Rectal examination: the sphincter is tonic, no pathological changes were detected at the height of the finger, the ampoule is empty.
X-ray examination: in the abdominal cavity there is dense content along the colon to the level of the descending intestine. Many pneumotized loops of the small intestine, dilated to 3.5-4 cm, with fluid levels in the form of high arches in the left half of the abdomen. No free gas was detected.
Ultrasound of the abdominal cavity: signs of free fluid in the abdominal cavity, dilation of small intestinal loops up to 4 cm with wall thickening up to 1 cm in the left abdomen - signs of small intestinal obstruction.
The patient was hospitalized in the surgical department, where conservative treatment was performed - nasogastric intubation, infusion and antispasmodic therapy, cleansing enemas.
X-ray control: contents and gas in the right half of the colon with a fluid level in the sigmoid colon, no contents were detected in the left half of the colon; the number of pneumatized loops of the small intestine has increased, the diameter is up to 4-5 cm, the folds are smoothed, the walls are thickened, the interloop spaces are widened; no free gas was detected.
Taking into account the negative dynamics of the clinical and instrumental picture of the disease, indications for emergency surgery were established 32 hours after admission. An upper-mid-median laparotomy was performed. An inspection at a distance of 1.5 m from the ligament of Treitz revealed a rod compressing the intestinal lumen and its mesentery, as well as multiple planar adhesions in other parts of the abdominal cavity. Intraoperative diagnosis: strangulation small bowel obstruction. Adhesive disease of the abdominal cavity. Strang dissection and adhesiolysis, nasoenteral and nasogastric intubation, lavage of the small intestine, sanitation, drainage of the abdominal cavity were performed (see Fig. 1 on the color plate)
.
The postoperative period is smooth. The patient was discharged home in satisfactory condition.
5 weeks after discharge, the patient was admitted to the institute again 3 days after the onset of the disease with complaints of cramping pain in the lower left abdomen, nausea, repeated vomiting, delayed passage of stool and gas, and general weakness. She was treated on her own - she took antispasmodic drugs with a temporary positive effect. On the day of admission, the condition worsened, the abdominal pain intensified, there was vomiting twice mixed with bile, and gases stopped passing.
On admission the condition was of moderate severity. The tongue is moist, covered with a whitish coating. The abdomen is swollen, soft, painful on palpation in the mesogastric and hypogastric region, more on the left. There are no peritoneal symptoms. The sound of splashing is detected. Peristalsis is audible and sluggish. After the enema, there was a small amount of stool, and some gases passed.
An X-ray examination revealed no free gas or fluid levels in the abdominal cavity, and moderate amounts of gas and solid contents along the colon.
Ultrasound of the abdominal cavity: no signs of free fluid in the abdominal cavity were detected; pronounced gastrostasis, the small intestine is dilated to 3.5-4 cm, inflammatory changes in the wall of the small intestine with wall thickening up to 1 cm are signs of small intestinal obstruction.
The patient was hospitalized in the surgical department, where conservative therapy was carried out with simultaneous determination of passage through the gastrointestinal tract using a radiopharmaceutical. Scintigraphy conclusion: the evacuation function of the stomach is sharply slowed down, there is a violation of the passage of the radiopharmaceutical through the small intestine with the absence of distal advancement of the indicator over 7 hours of observation. The data obtained correspond to the signs of small intestinal obstruction (see Fig. 2 on the color plate)
.
Figure 2. Radioisotope scintigrams.
X-ray control: dilation of small intestinal loops up to 4-5 cm, multiple small intestinal “arches” in the left parts of the abdomen - signs of high small intestinal obstruction, impaired passage through the gastrointestinal tract.
Taking into account the clinical and instrumental examination data, indications for emergency surgery were established. An upper-mid-median laparotomy was performed. During inspection in the abdominal cavity, a pronounced adhesive process was revealed, fixation of the loops of the small intestine with each other, with the mesentery, parietal peritoneum, and colon. In this case, there was compression of the intestinal lumen at a distance of 1.5 m and 1.8 m from the ligament of Treitz at the sites of angulation of the small intestine. At a distance of 70 cm from the ligament of Treitz, small intestinal intussusception was found (see Fig. 3 on the color plate)
.
The postoperative period is smooth. The patient was discharged after 2 weeks in satisfactory condition.
Patient T.
, 16 years old, was admitted with a combined injury (fall from the 2nd floor) 3 hours after the injury in serious condition to the intensive care unit. The examination revealed free gas in the abdominal cavity. An upper midline laparotomy was performed urgently. The audit revealed multiple ruptures of the serous membrane of the anterior and posterior walls of the stomach, a rupture of the anterioinferior wall of the descending part of the duodenum penetrating into the lumen, multiple ruptures of the serous membrane of the transverse colon. The ruptures of the serous membrane of the stomach and colon were sutured, the rupture of the duodenal wall was sutured, nasoenteric intubation, sanitation, and drainage of the abdominal cavity were performed.
In the postoperative period, conservative treatment was carried out. However, the patient noted moderate pain in the upper abdomen, nausea, and vomiting of stagnant gastric contents. On palpation, the abdomen is not swollen, soft, moderately painful in the upper sections. Additional space-occupying formations are not palpable. At the same time, the patient heard bowel sounds and passed gases. The clinical picture was interpreted as gastric paresis.
X-ray examination of the abdominal cavity on the 3rd day after surgery: gas and contents along the colon, no pathological changes were detected.
Ultrasound of the abdominal cavity on the 5th day after surgery - signs of a small amount of free fluid in the abdominal cavity, diffuse changes in the liver, edema of the head of the pancreas, tissue infiltration along the hepatoduodenal ligament, inflammatory changes in the wall of the stomach and duodenum, colon, hematoma of the retroperitoneal tissue on the right in the stage of organization, the fluid zone paraduodenally is 5.7×1.8 cm, at the root of the mesentery of the small intestine 7.8×1.9 cm.
Taking into account the clinical and instrumental picture, in order to assess the passage along the gastrointestinal tract, the patient underwent an X-ray examination with a water-soluble contrast agent (Urografin 76% 60 ml per os)
).
When assessing the results of the study after 4 and 10 hours from the start of the study, retention of the contrast agent in the stomach and in the dilated loop of the duodenum with some narrowing of the lumen (up to 1.5 cm) and deformation of the jejunum over 16 cm behind the ligament of Treitz is determined. There is progress of the contrast agent through the loops of the small intestine with its entry into the large intestine 4 hours after the start of the study with deformation of the internal contour of the large intestine at the level of the upper third of the descending colon in the form of “indentation from the outside” for about 5 cm, which was regarded as involvement intestines into an inflammatory infiltrate (Fig. 4)
.
Figure 4. X-ray (study with water-soluble contrast agent) 10 hours after the start of the study.
The clinical picture was interpreted as the development of postoperative infiltrate in the area of the sutured duodenum. However, despite the entire range of conservative therapy, no clinically significant improvement in the patient’s condition was achieved. On the 10th day after surgery, a repeat study of passage through the gastrointestinal tract was performed using barium sulfate. After 5 hours from the start of the study, its main part is determined in the lumen of the stomach and the dilated loop of the duodenum. There is a contrast in the initial sections of the jejunum for up to 6-7 cm with a narrowing of the lumen; in the more distal sections of the jejunum, barium suspension can be traced in the form of individual blots. When examined after 8 and 12 hours, barium suspension in the lumen of the stomach and duodenal loop (Fig. 5)
.
Figure 5. X-ray (study with barium sulfate) 5 hours after the start of the study.
Ultrasound of the abdominal cavity on the 10th day of the postoperative period: a deformed fragment of the small intestine is located in the left mesogastrium in the form of a four-layer structure over 7-10 cm in diameter up to 3.7 cm (a “target” symptom), the wall is sharply thickened, the layers are differentiated, with edematous folds, the contents have increased echogenicity, and peristalsis is enhanced. The blood flow in the intestinal wall is recorded. In other sections, the small intestine is not dilated, the walls are not thickened, and peristalsis can be observed. Severe gastroduodenostasis is noted. The pattern may be consistent with small bowel intussusception (Figure 6)
.
Figure 6. Echograms.
a - “pseudo-renal” symptom; b — “target” symptom. A computed tomography scan of the abdominal cavity was performed (Fig. 7)
.
Figure 7. CT scan.
Arrow – intussusception. When analyzing computed tomograms, there is twisting of intestinal loops in the mesogastrium on the left, edema of the adjacent mesentery and small fluid accumulations around. The picture may correspond to a strangulated intestinal loop (volvulus? intussusception?), minimal accumulation of fluid in the abdominal cavity. On the 10th day of the postoperative period, with suspected intussusception of the small intestine, the patient underwent relaparotomy. It was revealed that at a distance of 30 cm from the ligament of Treitz there is intussusception of the proximal part of the jejunum into the distal part at a distance of 20 cm. The intussusception of the small intestine was eliminated, the intestine was declared viable. Further, during inspection at a distance of 1.3 m from the ligament of Treitz, an infiltrate was revealed, consisting of several loops of the small intestine, fused with the root of the mesentery and the formation of an interintestinal abscess, which caused mechanical compression of the intestine with a violation of passage and the formation of intussusception of the small intestine in the proximal section (see. Fig. 8 on color insert)
.
The postoperative period proceeded smoothly. The patient was discharged from the hospital in satisfactory condition on the 10th day after the second operation.
Thus, an uncharacteristic clinical picture with the absence of the classical triad may occur with postoperative intussusception of the small intestine. Ultrasound and MSCT play a leading role in the diagnosis of intussusception. The cause of intussusception may be adhesive intestinal obstruction. Therefore, in addition to eliminating intussusception, it is necessary to inspect the intestine and, in the presence of a mechanical obstruction (adhesion, strain, infiltrate), restore passage through the small intestine.
Introduction
Small intestine intussusception is one of the rare causes of acute intestinal obstruction. Intussusception is defined as introduction of the distal part of intestine in proximal direction. There is mesentery compression between inner and middle cylinders of invaginate [5, 22]. This type of intestinal obstruction consists of 15% of all cases of mechanical intestinal obstruction [7]. Small intestine intussusception after abdominal surgery is diagnosed in 1-5% of observations [11, 16, 20]. T. Pavlidis and colleagues report that intestinal intussusception in adults was diagnosed in 7 of 368 (1.9%) patients who underwent surgery for small intestine obstruction for the last 12 years [19].
The mechanism of intussusception isn't clear completely. Polyps, disorders of blood supply, primary and metastatic tumors of small intestine, Meckel's diverticulum are frequent causes of intussusception [1, 2, 20]. In some cases it is not possible to establish the cause and triggering mechanism of motility disorders. It is possible to talk about the “primary intussusception” in this case which is revealed in 8-20% of cases of intestinal intussusception [13, 15].
Another cause of intussusception may be abdominal adhesive disease with small intestine obstruction. There is mechanical obstruction with intestinal lumen compression in this case. It is associated with increased peristalsis in the proximal intestinal part which provides intussusception in aboral direction [10].
Intussusception symptoms correspond to those in case of intestinal obstruction. Diagnostics is very difficult in patients with abdominal adhesive disease after repeated surgical interventions. Thus the diagnosis is often confirmed in operating theater. Classic triad including cramp-like abdominal pain, bloody stool and palpable tumor (invaginate) aren’t practically described in adults in contrast with children [13, 18].
Intussusception diagnostics according to X-ray, ultrasonic and multislice CT data is based on identification of signs of high or low (distal or proximal) intestinal obstruction in combination with typical intussusception signs [6, 12, 14, 15, 19, 21]. It should be noted that echographic examination of abdominal abdominal organs and multislice CT are equivalent sensitive methods [13, 16]. Ultrasonic signs of intussusception are “hyperechoic center”, feebly marked or absentee layers of concentricity in intestinal conglomeration, profile blurring and presence of liquid between cylinders of invaginate. It is direct signs of pronounced circulatory disorders in the wall of strangulated intestine. "Target", "pseudo-kidney" and "forceps" signs provide accurate diagnosis in 100%, 98.9% and 68.8% respectively. All mentioned symptoms have high specificity and sensitivity [6, 14, 15].
Additionally, multislice CT estimates circulatory disorders inside of invaginate with detection of blood flow in mesenteric segment compressed between walls of intestine [6, 12, 14].
Desinvagination, assessment of bowel segment viability, adhesiolysis are chosen for secondary intussusception surgical treatment [8, 9, 15, 17, 21].
We present clinical cases of small intestine intussusception in the early postoperative period in adults.
Patient L.
, 72 years old, admitted with complaints for cramp-like pain in lower left sections of abdomen, nausea, multiple vomiting, delay of stool and flatus passage, general weakness.
Anamnesis included panhysterectomy for ovarian tumor in 2012, nephrectomy for renal tumor in 2013. It was revealed episode of adhesive intestinal obstruction in the early postoperative period after last surgery. Patient received drug therapy.
It was diagnosed patient's moderate severity in the front office. Tongue is moist and coated. Belly is swollen, soft and painful in mainly left mesogastric and hypogastric areas. There weren't peritoneal symptoms. Splashing sound was diagnosed. Sluggish peristalsis is auscultated. Small amount of stool and flatus was detected after cleansing enema. Sphincter tonicity, empty ampulla of the rectum were revealed during rectal investigation. There weren't abnormalities at the height of finger.
X-ray study has demonstrated dense contents in the abdominal cavity along the colon to the level of descending colon. A lot of pneumatized, enlarged to 3.5-4 cm loops of small intestine with liquid levels as high arch in left abdominal part were diagnosed. Free gas wasn't revealed.
Abdominal ultrasonic scanning showed signs of free fluid in the abdominal cavity, small intestine enlargement up to 4 cm with wall thickening up to 1 cm in left abdominal part. It was recognized as symptoms of small intestine obstruction.
Patient was hospitalized into surgical department where nasogastric intubation, infusion and antispasmodic therapy, cleansing enema were performed.
X-ray control revealed contents and flatus in right half of colon with liquid levels in sigmoid colon. Contents in left half of large bowel was not found. The number of pneumatized loops of small intestine was increased. Diameter increased up to 4-5 cm. Folds are smoothed. Walls are thickened. Inter-looping spaces were enlarged. Free gas wasn't revealed.
Emergency operation has been indicated in view of negative clinical and instrumental dynamics in 32 hours after admission. Upper-middle-median laparotomy was performed. Extrusion at a distance of 1 m from the Treitz ligament was found during surgery. It compressed bowel lumen and its mesentery. Also multiple commissures in other parts of the abdominal cavity were found. Intraoperative diagnosis was defined as strangulation small intestine obstruction, adhesive disease of abdominal cavity. Extrusion intersection, adhesiolysis, naso-enteral and nasogastric intubation, small intestine lavage, sanitation, abdominal cavity drainage were performed (fig. 1)
.
Figure 1. Intraoperative photographs.
a — strangulation of the small intestine; b — strangulated area of the intestine; c - demarcation line; d — nasoenteric intubation was performed. Postoperative period is smooth. Patient was discharged in satisfactory condition.
In 5 weeks after discharge the patient was admitted iteratively in 3 days after symptoms appearance. There were complaints for cramp-like pain in lower left sections of abdomen, nausea, multiple vomiting and delay of stool and flatus passage, general weakness. Patient used spasmolytic drugs on one's own with temporary positive effect.
In admission day patient's condition has been deteriorated. Abdominal pain is increased. There was vomiting with a bile impurity twice. There wasn't passage of flatus.
It was diagnosed patient's moderate severity in the front office. Tongue is moist and coated. Belly is swollen, soft and painful in mainly left mesogastric and hypogastric areas. There weren't peritoneal symptoms. Splashing sound was diagnosed. Sluggish peristalsis is auscultated. Small amount of stool and flatus was detected after cleansing enema. Partially passage of flatus was observed.
X-ray investigation didn't reveal free gas and liquid levels in the abdominal cavity. There were moderate amounts of gas and dense content along colon.
Abdominal ultrasonic scanning didn't show signs of free fluid in the abdominal cavity. There was pronounced gastrostasis. Small intestine was enlarged up to 3.5-4 cm. It was observed inflammatory changes in intestinal wall with thickening up to 1 cm. It was recognized as symptoms of small intestine obstruction.
Patient was hospitalized into surgical department where she had drug therapy with passage through the GI tract defining by using of scintigraphy. It was concluded that gastric evacuation function is slowed down. It was diagnosed absence of radiopharmaceutical promotion through small intestine during 7 hours. Received data confirm signs of small intestine obstruction (fig. 2)
.
Figure 2. Radioisotope scintigrams.
X-ray control revealed signs of high intestinal obstruction such as enlargement of small intestine loops up to 4-5 cm, multiple small intestinal arches in left abdominal parts.
Emergency surgery was indicated in view of clinical and instrumental data. Upper-middle-median laparotomy was performed. Revision of the abdominal cavity revealed adhesive process, fusion of intestinal loops among themselves, with mesentery, parietal peritoneum and colon. Also there was compression of intestinal lumen at a distance of 1.5 and 1.8 m from the Treitz ligament in angulation sites. Small intestinal intussusception was diagnosed at a distance of 70 cm from the Treitz ligament (fig. 3)
.
Figure 3. Intraoperative photographs.
a — type of intussusception (arrow); b, c, d — stages of disinvagination. Intraoperative diagnosis: small intestine intussusception, adhesive intestinal obstruction. Adhesiolysis, small intestine desinvagination with elimination of obstruction, naso-enteral intubation, intestinal lavage, sanitation and abdominal drainage were performed. Postoperative period is smooth. The patient was discharged in 2 weeks in satisfactory condition.
Clinical observation No. 2. Patient T.
, 16 years old, admitted with combined trauma in 3 hours after injury in severe condition in intensive care unit. Fall from the second floor caused trauma. Free gas in abdominal cavity was diagnosed. Emergency upper-middle laparotomy was performed. Multiple ruptures of serous tunic of anterior and posterior stomach walls, through rupture of the anteroinferior wall of descending part of duodenum, multiple ruptures of serous tunic of transverse colon were revealed. It was done suturing of ruptures of stomach and colon serous tunic, wall of duodenum, naso-enteral intubation, sanitation and abdominal drainage.
Drug therapy was performed postoperatively. Nevertheless the patient had moderate pain in the upper abdomen, nausea, vomiting with stagnant gastric contents. Belly isn't swollen, soft and moderately painful in the upper part. There weren't additional space-occupying lesions. Herewith intestinal murmur was auscultated. Passage of flatus was diagnosed. Symptoms were recognized as gastroparesis.
X-ray investigation on the third day after surgery found gas and content along colon. Abnormalities weren't found.
Abdominal ultrasonic scanning on the fifth day after surgery revealed a small amount of free liquid, diffuse liver changes, edema of pancreatic head, tissues infiltration along hepatoduodenal ligament, inflammatory changes in stomach and duodenum walls, colon. Also it was found retroperitoneal hematoma on the right in organization stage, paraduodenal fluid area 5.7×1.8 cm, in root of mesentery 7.8×1.9 cm.
In view of clinical and instrumental data X-ray investigation with water-soluble contrast on the seventh day after surgery was performed. Urografinum 76% 60 ml per oral was used. Assessment of the results in 4 and 10 hours after investigation revealed delayed passage of contrast in stomach and extended duodenum with some luminal narrowing (up to 1.5 cm) and jejunal deformation for a 16 cm behind Treitz ligament. It was diagnosed the arrival of contrast into colon in 4 hours after investigation start. There was deformation of interior contour at the level of upper third of the descending colon as “impression from the outside” for about 5 cm. It was recognized as involvement of bowel in the inflammatory process (fig. 4)
.
Fig.
4. X-ray photograph (investigation with water-soluble contrast) in 10 hours after start of the study Clinical symptoms were interpreted as development of postoperative infiltrate in the area of sutured duodenum. There wasn't significant improvement of the patient's condition although complex drug therapy was performed. On the 10th day after surgery repeated investigation of gastrointestinal transit with barium sulfate was done. In 5 hours after start of investigation the most of contrast agent is located in stomach and extended duodenum. Initial parts of the jejunum for 6-7 cm are contrasted with luminal narrowing. In more distal parts barium sulfate is detected as single touches. In 8 and 12 hours barium meal is in the lumen of the stomach and in loop of duodenum (fig. 5)
.
Fig.
5. X-ray photograph (investigation with barium sulfate) in 5 hours after start of the research Abdominal ultrasonic scanning on the 10th day after surgery revealed deformed jejunal fragment in left mesogaster as four-layer structure for 7-10 cm and with diameter up to 3.7 cm (“target” symptom). Its wall is dramatically thickened; layers are differentiated with edematic folds. Content had increased echogenicity. Peristalsis was strengthened. Blood flow in intestinal wall was registered. In other parts small intestine wasn't extended, walls weren't thickened, peristalsis was detected. There was pronounced gastroduodenostasis. Such signs may correspond to small intestine intussusception (fig. 6)
.
Fig.
6 Sonograms. A - pseudo kidney sign. B - target sign. Computed tomography of abdominal cavity was performed (fig. 7)
.
Fig.
7 CT-scan. Arrow - invaginate. Analysis of CT scans revealed torsion of intestinal loops in left mesogaster, edema of adjacent mesentery and small liquid accumulation around. Signs may correspond to strangulation of intestinal loop (volvulus? intussusception?), minimal hydroperitoneum. Relaparotomy was performed for suspicion on small intestine intussusception on the 10th day postoperatively. It was diagnosed intussusception of jejunal proximal part into distal part at a distance of 20 cm. An intussusception was found at a distance of 30 cm from Treitz ligament. Removal of intussusception was done; intestine is recognized as a viable. Further revision found out an infiltrate at a distance of 1.3 m from Treitz ligament. An infiltrate consisted of several intestinal loops bound with root of mesentery and forming of interintestinal abscess. It caused mechanical intestinal compression with disorders of passage and development of small intestine intussusception in proximal part (fig.
.
Fig.
8. Intraoperative photographs. a - expansion of the adductor section of the intestine; b - disinvagination; c - adhesiolysis; d — separation of infiltrate. Adhesiolysis, nasointestinal intubation and drainage of abdominal cavity were performed.
Postoperative period was smooth. The patient was discharged on the 10th day after the second surgery in satisfactory condition.
uncharacteristic symptoms with absence of classic triad may be revealed in case of postoperative intussusception of Thus intestine. Ultrasound and multislice CT have a main role in diagnostics of intussusception. Adhesive intestinal obstruction may be cause of intussusception. Therefore besides intussusception removal it is necessary to revise the intestine and to recover passage through small intestine in case of its mechanical obstruction (commissure, infiltrate).