The lifestyle followed by most of the world's population does not always mean a healthy lifestyle and nutrition. One of the most common health problems is disorders of the gastrointestinal tract. Discoveries in the medical field in recent years make it possible to painlessly carry out various diagnostics of the human body.
The presence of pathologies can be detected in conditions that are comfortable for the patient and as efficiently as possible. Diseases of the gastrointestinal tract can be detected at any stage and even without obvious clinical signs and symptoms. Only a qualified medical professional can make a correct diagnosis.
Modern scientists offer several types of intestinal diagnostics, differing in the type of problem, severity and characteristics of a particular patient. Bowel examination methods include:
- Capsule examination;
- Endoscopic examination;
- Colonoscopy;
- Irrigoscopy.
Capsule examination and its features
Capsule examination is used for abdominal pain and suspicion of a tumor.
A capsule examination is performed by swallowing an enterocapsule with a video camera built into it. This method came into domestic medicine thanks to the Israeli scientists who invented it.
The big advantage of capsule diagnostics is minimal invasiveness and high information content. The doctor performing the procedure will be able to specifically assess the internal state of the patient’s gastrointestinal tract. A similar diagnostic method is recommended for those patients who have the following symptoms:
- abdominal pain;
- hidden bleeding;
- suspected congenital disease;
- suspicion of a tumor.
The diagnostic process begins with attaching a recording device to a person's body, after which he must swallow a video capsule. The device moves through the gastrointestinal tract due to peristalsis waves.
After these manipulations, the data obtained as a result of the survey is processed by special computer programs. The duration of data processing can reach about 8 hours. The specialist will determine the presence of polyps, tumors, including cancer, as well as all other intestinal pathologies. The capsule is excreted from the body naturally.
In some cases, namely when the patient has weak intestinal motility, a slightly different capsule called Patency is used. Its purpose is to identify narrowed areas of the intestine.
Development mechanisms
Causes of acute gastritis in children:
- Foodborne illness (a gastrointestinal disease that occurs after eating food containing bacteria and their toxins. Often occurs due to the consumption of rotten foods, unwashed fruits or dirty water);
- Long-term use of certain medications (salicylates, sulfonamides, glucocorticoids, digitalis preparations, etc.);
- Poisoning with household poisons;
- Allergy.
When a large number of bacteria enter the gastrointestinal tract, inflammation occurs. Excess fatty, spicy and poorly chewed food slows down the evacuation (removal) of stomach contents and worsens the secretory function of the organ (the secretion of digestive juice for digesting food). The food lump lingers in the stomach, it is saturated with enzymes, after which it disintegrates due to the action of bacteria, and the fermentation process begins.
Which leads to aggravation of the course and chronicity of the process.
Causes of chronic gastritis in children:
- The presence of the bacterial flora Helicobacter pylori (the same bacterium leads to ulcers). In 80-85% of cases it is what causes gastritis;
- Poor nutrition (eating rough, too hot or cold, fatty, spicy or poorly chewed food);
- Dry food;
- Eating 1-2 times a day or less often;
- Lack of vitamins, complete proteins and fats in the diet;
- Endocrine diseases;
- Kidney damage;
- Diseases of the cardiovascular system;
- Long-term use of medications (salicylates, sulfonamides);
- The source of infection in the oral cavity (disease of teeth and gums);
- Burdened heredity;
- Allergies.
The factors that cause acute and chronic gastritis are similar or even coincide. The main difference is the duration of their effect on the body. In acute gastritis, one contact with an irritant (expired cottage cheese or a large portion of fast food) is enough for an attack. In chronic gastritis, an irritating factor acts on the gastric mucosa for a long time and repeatedly, gradually leading to a decrease in the activity of the digestive glands.
Endoscopic examination
Endoscopic examination is used to detect tumors and polyps.
This diagnostic method is used to determine the patient’s hidden pathologies, such as polyps and tumors. The process is safe for the patient and also painless.
Thanks to endoscopy, the condition of the intestinal mucosa can be accurately assessed. The doctor examines the lining of the esophagus, stomach, duodenum, large intestine and small intestine.
The process is carried out on an empty stomach. The patient must first stimulate cleansing with laxative medications. The next stage is the introduction of an ultrasound sensor into the rectum.
Then, when the device reaches the required area of the intestine, the doctor assesses the condition of the formation or other pathology and, based on what he sees, takes further actions and treatment methods.
Contraindications. Endoscopy is not recommended for people with heart or lung disease due to exposure to special medications. But in any case, this issue is resolved individually with each patient, based on the conditions of the particular case.
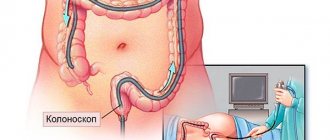
Colonoscopy
Colonoscopy is a method of studying and assessing the condition of the walls of the gastrointestinal tract.
This is a diagnostic method that many patients do not like. You can’t call it painful, rather it’s unpleasant, but its effectiveness is very high.
Colonoscopy is performed using a fiber colonoscope, which is inserted into the patient’s body after cleansing the intestines with a special laxative. The procedure lasts about 30 minutes, during which the patient may feel bloating.
A fiber colonoscope is a medical tourniquet that has a flexible texture and is equipped with an optical system. Thanks to this device the following manipulations are possible:
Irrigoscopy
Irrigoscopy is an examination of the gastrointestinal tract using x-rays.
Irrigoscopy is an examination of the gastrointestinal tract using x-rays. It is first necessary to cleanse the intestines as much as possible, using enemas and laxatives. On the eve of irrigoscopy, the patient should not eat.
Before diagnosis, the patient takes barium sulfate orally, which is a radiopaque substance. The substance fills parts of the intestine and helps the doctor examine its contours and the degree of lumen, which will later help identify the presence of pathologies.
In some cases, it is necessary to carry out a double contrast method. What does it mean? After the intestine is cleared of the radiopaque substance, it is filled with air. Thanks to this, it is also possible to determine the outlines of all parts of the intestine.
Based on the contours seen, the doctor determines the presence of fistulas, tumors, diverticulosis, congenital pathologies, ulcerative formations, scars, and so on. Irrigoscopy is safe and painless, the patient is minimally exposed to radiation. In what cases is irrigoscopy recommended:
- discharge of mucus and pus from the intestines;
- pain in the anus and colon;
- chronic stomach upset (diarrhea, constipation);
- bleeding from the rectum;
- suspicion of a tumor in the gastrointestinal tract;
- inability to perform a colonoscopy to accurately formulate a diagnosis;
- intestinal obstruction (the presence of this diagnosis is confirmed using x-rays and ultrasound examinations).
Treatment
The treatment plan for gastritis in children depends on the form of the disease and its severity.
Therapy for acute gastritis includes:
- Bed rest for 2-3 days;
- Gastric lavage;
- Hunger in the first 8-12 hours after the onset of symptoms, then switching to liquid food (puree soups, low-fat broths, crackers without spices and salt, jelly and porridge), on days 5-7 the child is transferred to normal food;
- Drink plenty of fluids (preferably special solutions for rehydration);
- In case of severe dehydration, saline solution with 5% glucose solution is administered intravenously;
- Laxative for constipation;
- Antiemetics for vomiting;
- Antibiotics for infection;
- Additionally: B vitamins, enzymes for the gastrointestinal tract.
For chronic gastritis, the following is additionally prescribed:
- Eradication therapy (a special treatment regimen for the destruction of Helicobacter pylori (omeprazole + amoxicillin + imidazole/metranidazole/clarithromycin). Duration - 10 days. If ineffective, the regimen is changed.
- M-cholinergic receptor blocker to relax the smooth muscles of internal organs and suppress the secretion of the digestive glands.
- Antacids, histamine H2 receptor blockers to reduce gastric secretion.
Treatment is carried out until remission occurs, the duration of which is variable: from several months to several years.
Diagnosis of the large intestine
A blood test provides a lot of information about a person's health status.
To determine diseases of the colon, doctors prescribe a number of required examinations and tests.
Initially, a blood test is performed for clinical and biochemical composition. To determine dysbiosis, the patient submits stool to the laboratory. Five main techniques for examining the rectum:
- anoscopy;
- sigmoidoscopy;
- fibrocolonoscopy;
- laboratory diagnostics of stool for dysbacteriosis;
- blood analysis.
A digital rectal examination is necessary, which should be performed at any hint of pelvic organ disease. This procedure is carried out by a doctor using special devices.
To begin with, the condition of the anus muscles is analyzed, which will help identify a number of diseases: hemorrhoids, anal fissures, narrowing in the intestinal lumen, tumor formations, scars, and so on. In some cases, a rectoscope is used, which is necessary for diagnosing more deeply removed areas of the colon.
Diagnosis of the small intestine
The examination begins with diagnosing the condition of the duodenum, jejunum and ileum. The localization of these areas of the gastrointestinal tract is between the large intestine and the stomach. A specialist in this field is a gastroenterologist. For diagnostics use:
- fiberoscopy;
- irrigoscopy;
- endoscopy;
- ultrasonography;
- X-ray.
An appointment for a comprehensive examination can only be obtained from a gastroenterologist. Before making a diagnosis, it is important to follow a diet for several days to unload the gastrointestinal tract.
Thanks to endoscopy, it is possible to identify pathologies of varying degrees of severity in a patient. Just as often as endoscopy, to diagnose the small intestine, the rectoscopy method is used (examination of the internal walls of the intestine with a sigmoidoscope). Thanks to endoscopy, the following problems are solved:
- getting rid of polyps;
- stopping bleeding;
- installation of a feeding tube;
- removal of foreign objects.
Another highly effective way to detect diseases of any part of the small intestine is double-balloon enteroscopy, performed on the patient under general anesthesia. It is used if the patient has:
- tumor formations;
- adenomatosis;
- polyps;
- bleeding in the small intestine;
- the presence of foreign bodies in the small intestine.
How to properly prepare for research
Before performing an ultrasound of the intestines or before a colonoscopy, patients will have to follow certain recommendations of a similar nature:
- a few days before the study, patients need to exclude from their diet any foods that cause increased gas formation;
- approximately 24 hours before the examination, food intake should be minimized and dinner should be replaced with a light snack;
- in the evening or early in the morning you need to empty the intestines of feces. If this cannot be done naturally, then you should definitely resort to a cleansing enema.
- In order to fully cleanse the intestines, absorbent drugs can be very effective, such as:
- "Enterosgel";
- "Smecta";
- "Polysorb".
Before the study, experts also advise taking medications to reduce gas formation. Compliance with all preparatory measures will guarantee a highly informative survey.
Small bowel cancer
Small intestinal cancer causes pain and problems with intestinal patency that disappear.
Colorectal cancer (cancer of the small intestine) is often very difficult to identify. This disease may be hidden behind the mask of another pathology; doctors need to work hard to identify it.
The main signs of small intestine cancer are persistent pain in the abdomen and problems with intestinal patency. Especially if the pain is increasing in nature, then it is necessary to schedule one or more examinations.
Bowel cancer may be present even if the ultrasound is negative. Since cancers are often hidden, doctors often fail to see them the first time.
Many, in order to unambiguously determine the presence of the disease, turn to specialists in Israel and Germany for help, since they have the most modern techniques and equipment. If there is even the slightest suspicion of a cancerous tumor, then examinations will have to be continued until a definite diagnosis is known.
In addition to the diagnostic methods already mentioned, there is a procedure called enteroscopy. This procedure involves an endoscopic examination, sometimes accompanied by a biopsy.
Magnetic resonance imaging (MRI)
Magnetic resonance imaging is a painless method for examining the intestines.
Magnetic resonance imaging is a safe method for examining the intestines, without causing pain to the patient.
MRI will allow you to find out whether the patient has chronic diseases of the gastrointestinal tract. Before starting, it is important to cleanse the intestines with an enema. Next, the patient receives the contrast agent. The duration of the procedure is very short (only 10 minutes).
Thanks to the MRI method, a doctor specializing in this problem will be able to accurately determine the severity of the disease, examine each section of the intestine, and find metastases (if any). Also, thanks to magnetic resonance imaging, the presence of malignant tumors can be detected.
Stool tests
How to check in another way is a question that is relevant for most people over 40 years old. Regularly performing this endoscopic procedure is associated with quite a lot of inconvenience for the patient and requires careful preparation and diet. An alternative may be DNA testing of stool. They are aimed at identifying specific DNA molecules belonging to tumor cells.
Stool can also be analyzed for the presence of occult blood and a fecal immunochemical test can be performed. All these laboratory techniques make it possible to accurately detect cancer, even at the earliest stages of development.
Important
Please note that any intestinal examination cannot serve as a complete replacement for colonoscopy. In most cases, they are used as screening, that is, to detect signs of pathology in the early stages of development.