The article was prepared by a specialist for informational purposes only. We urge you not to self-medicate. When the first symptoms appear, consult a doctor.
Standard laboratory diagnostics do not detect many intestinal diseases. Some serious pathological processes occurring in the organ require colonoscopy. In the article we will analyze why this procedure is needed and whether there is any alternative to it.
What is a colonoscopy?
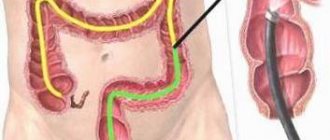
Colonoscopy is a modern diagnostic procedure that is performed using a special probe, an endoscope. This allows the doctor to examine the inside of a person's intestine. The procedure makes it possible to assess the condition of the anus, rectum to the entrance to the cecum, ileocecal canal, and terminal ileum.
A colonoscope is a flexible and long probe. At its end there is an eyepiece and a miniature video camera with backlight. The device comes with forceps, which are used to remove tissue for further examination, as well as a tube for air supply. The probe is inserted through the rectum. It is soft and bends easily, so it delicately moves along the entire length of the intestine without injuring it or causing pain to the patient.
The image from the camera is displayed on the screen, so the doctor can visually assess the condition of the intestines, which are equivalent to 2 meters in length. The camera takes pictures with tenfold magnification. The doctor examines the mucous membranes of the intestines and has the opportunity to evaluate all its pathological changes.
In addition to a routine examination of the intestines, the doctor can perform a number of medical procedures that will allow you to avoid surgery:
- It is possible to expand a certain area of the intestine by removing scar tissue.
- Tissues can be taken for further histological examination.
- Foreign bodies can be removed from the intestines.
- The doctor can remove polyps and other benign tumors.
- It is possible to stop the bleeding.
Colonoscopy is one of the effective modern methods for diagnosing intestinal diseases.
Difference between colonoscopy and MRI
You can do an MRI of the intestines instead of a colonoscopy, but first you need to understand what the features of these procedures are and how they differ.
Magnetic resonance imaging is performed using open and closed tomographs. Tunnel models allow you to get a clearer picture.
Fiberscopes are waterproof devices made of optical fiber that allow you to adjust the angle of rotation of the end part of the device.
MRI of the intestine is a safe technique that does not require intervention in the body. An exception is an intravenous injection of a contrast agent.
In the case of colonoscopy, the instrument is inserted through the anus; in some cases, local anesthesia is used. If required, a biopsy is performed at the same time.
Colonoscopy does not require amplification. The doctor receives a picture of the lumen of the digestive canal in video format.
For MRI, double contrast is used - gadolinium solution is administered orally and intravenously. The procedure allows you to obtain black and white photographs in three projections.
Indications for endoscopic examination of the colon
Indications for colonoscopy are the following diseases and conditions:
- The person is over 50 years old. In this case, the procedure is carried out for preventive purposes, even if the person does not make any complaints about his health. The fact is that the risk of developing cancer of the distal parts of the intestine over the age of 50 increases significantly, and the onset of the disease is asymptomatic. Therefore, all persons over the age of 50 are recommended to undergo a colonoscopy once a year.
- If a person has a hereditary predisposition to the formation of polyps in the intestines, and also in the family history there were people who suffered from cancer of this organ. Provided that there was a relative in the family who suffered intestinal cancer, then for preventive purposes you need to start undergoing this procedure 10 years earlier than the age at which the pathology was discovered in this relative. This is explained by the fact that the likelihood of transmitting the disease at the genetic level is extremely high.
Symptoms that should alert a person and force him to undergo a colonoscopy are:
- The presence of blood in the stool. It looks like scarlet veins. This symptom indicates that there is bleeding from the distal parts of the intestine. A similar situation is often observed with anal fissures and hemorrhoids. In addition, there may be hidden blood in the stool that cannot be seen with the naked eye. To detect it, special rapid tests will be required. Occult blood in the stool may indicate the presence of polyps, intestinal inflammation, tumors, ulcerative colitis and Crohn's disease.
- The appearance of mucus and purulent discharge in the stool. They indicate a serious intestinal pathology that requires emergency medical attention.
- Anemia and high ESR. If a patient suffers from chronic anemia that cannot be corrected with medications, then this is a reason for a colonoscopy.
- Loss of body weight. If a person begins to lose weight for no apparent reason, then the digestive system needs to be examined.
- The presence of polyps in the intestines. All benign neoplasms in the intestine have a tendency to malignant degeneration, and therefore require removal and systematic monitoring in the future.
- Pain along the intestines. Dull and cramping pain, which is localized in various parts of the intestine, requires a colonoscopy.
- Chronic constipation. If a person suffers from constipation, if he has tight stools, which leads to injury to the intestinal walls and anus, then this can cause serious inflammation. In addition, constipation itself may indicate a disease of the organ, so a detailed examination is required.
- Unstable stools, alternating diarrhea and constipation, malabsorption syndrome may be signs of irritable bowel syndrome, so such patients are prescribed a colonoscopy.
Emergency indications for endoscopic examination of the colon
Emergency colonoscopy has a therapeutic rather than a preventive purpose. It is carried out when the patient requires emergency care.
Such situations include:
- Intestinal obstruction, its stenosis. The disorder can develop against the background of various diseases, as well as after surgery.
- Bleeding from the intestines, including with diverticulosis. During the procedure, it is possible to identify the source of inflammation and eliminate it.
- Presence of a foreign body in the intestine.
Execution Goals
Using a colonoscope, the doctor can detect ulcers, polyps, foci of inflammation, tumors, and sources of intestinal bleeding. In addition, during the study it is possible to obtain tissue samples from the intestines for histological and cytological examination, as well as to remove polyps or other formations.
Colonoscopy, diagram
It is recommended to have your first colonoscopy at age 50. Further recommendations are given individually, depending on the results of the study. Unfortunately, most colon tumors are detected at late stages. There is only one reason here - late diagnosis of the tumor. The only way to detect a tumor at an early stage is regular examination of the colon, which allows us to identify pre-tumor pathology and remove it, or carry out other necessary treatment so that it does not degenerate into cancer. The key to curing colon cancer is early diagnosis. Early diagnosis can be achieved using endoscopy. [1]
Contraindications
Colonoscopy is a low-traumatic diagnostic method, but it has a number of contraindications in which the procedure cannot be performed.
These include:
- State of shock with a drop in blood pressure below 70 mm. rt. Art.
- Acute respiratory infections, inflammation of the respiratory system, accompanied by an increase in body temperature.
- Intestinal infections in the acute phase.
- Peritonitis.
- Heart failure.
- Blood clotting disorder.
- Crohn's disease, acute stage of colitis with massive intestinal damage.
- Diverticulitis in the acute phase.
- Severe disturbances in a person’s well-being.
In addition, there are relative contraindications to the procedure:
- Massive anal bleeding.
- Anal fissures.
- Acute stage of hemorrhoids.
- Paraproctitis.
- The period of bearing a child.
- Presence of a large hernia.
- Early recovery period after abdominal surgery.
- Diverticulitis.
- Poorly conducted preparation for cleansing the intestines, etc.
Doctors should seriously evaluate the possible risks of performing a colonoscopy if the patient has the following diseases and conditions:
- Heart diseases.
- Allergy to medications.
- Lung diseases.
- Diabetes.
- Treatment with drugs that affect blood clotting processes.
The doctor must be aware of the medications the patient is receiving. You may have to stop taking them and resume taking them after the procedure.
Video: Live healthy! “Colonoscopy - what is this procedure and who should undergo it?”:
Colonoscopy in a state of medicated sleep
Endoscopic examination of the intestine is usually painless, but the patient may experience discomfort from a feeling of bloating (this goes away immediately after the procedure) and the advancement of the probe through the loops of the intestine. In Euroonco clinics it is possible to carry out the procedure in a state of medicated sleep. In this case, the patient is given a special sedative, under the influence of which he is plunged into deep sleep. After approximately 40 minutes, the effect of the drug ends, and within 5-10 minutes after waking up the patient can walk and talk, and after an hour he can go home.
Preparing for a colonoscopy
Preparation for a colonoscopy begins several days before the procedure. The person will have to follow a certain diet and take measures to cleanse the intestines.
2-3 days before the study you need to switch to a slag-free diet. Vegetables, nuts, meat, fruits, baked goods, and cereals are removed from the menu. 20 hours before the procedure, you can only drink water and lightly brewed tea.
To get maximum information, you need to remove feces from the intestines. To do this, the patient is given an enema, or special medications are prescribed, for example, Fortrans, Lavacol, etc. They begin to take them a day before the upcoming colonoscopy.
The more carefully the patient follows the doctor’s recommendations, the more information the doctor will be able to obtain about the condition of the intestines:
- You should stop taking activated carbon, iron supplements, and blood thinning medications 10 days before the procedure.
- If the patient has an artificial heart valve, then before the study he needs to take an antibacterial drug. This will reduce the likelihood of developing endocarditis.
- On the eve of the study, you can take an antispasmodic, for example, No-shpu or Dicetel. However, this can only be done after medical consultation.
- Doctors recommend stopping taking NSAIDs and medications to stop diarrhea, such as Imodium or Lopedium.
When can I get my colonoscopy results?
A description of the intestinal condition can be obtained a couple of days after the procedure. If a biopsy was performed during colonoscopy, the time period increases until the histological examination data is obtained. In the conclusion, the compliance of the patient’s intestinal tube with certain criteria is indicated, as well as additional manipulations performed (if any). In addition to documents, you will be given a disc with a photograph or a reproduction of the colonoscopy process. Patients pass on the information received to the attending physician to determine further tactics for patient management.
Procedure for performing a colonoscopy
A person undergoing a colonoscopy for the first time will be interested in the steps involved in the procedure.
Having this information at your disposal, you can set yourself up to carry out the research as easily as possible:
- The patient lies on the couch on his left side and presses his knees to his stomach.
- The doctor treats the anus with an antiseptic drug and inserts a probe into it. Anesthesia is not used. If the patient has a high pain threshold, local anesthetics can be used for pain relief. Sedation can also be performed, but this reduces the diagnostic value of the procedure. Severe pain can only occur if a person has acute inflammation of the intestines or there are adhesions in it. In this case, anesthesia is indicated for a period of half an hour.
- After anesthesia, the doctor inserts a probe into the anus and slowly moves it forward. To straighten the folds of the intestines, air is supplied through the tube.
- The probe is advanced deep into the intestine 2 meters. All this time, the doctor will evaluate the condition of the internal walls of the organ.
The procedure continues for 20-30 minutes. The examination cannot be called pleasant, so it is often practiced under anesthesia.
Additional Research
During the procedure, the doctor can detect pathological changes in the mucous membrane of the organ, polyps and neoplasms. In this case, he performs a biopsy. Using special forceps, which are part of the endoscope, the doctor removes tissue.
Before the biopsy is performed, a local anesthetic is administered through the endoscope tube. Then, using forceps, the doctor cuts off a small section of diseased tissue and removes it out. In addition, during a colonoscopy, the doctor can remove small polyps, as well as single tumors. In this case, the doctor does not use forceps, but a special device that resembles a loop. With its help, the doctor grabs the growth at the very base and cuts it off.
Capsule endoscopy
When using this technique, the study is carried out in a special capsule equipped with cameras and other sensors, which the patient must swallow. It scans the digestive tube as it naturally progresses and transmits data via wireless communication systems. This technique is one of the options for examining the intestines for diseases without the use of colonoscopy.
Main advantages:
- Simplicity and painlessness.
- Extensive data on the state of the digestive tract.
- High quality images and a lot of additional data.
Capsule endoscopy also has disadvantages, the main one being the inability to take a biopsy and perform other manipulations. The movement of the capsule cannot be controlled, so the suspicious area cannot be examined in more detail.
Possible complications and undesirable consequences
Colonoscopy is a safe diagnostic method, but the procedure must be performed by a professional.
Complications are rare, but they are possible.
These include:
- Perforation of the intestinal wall. This is observed no more often than in 1% of cases.
- Bloating that goes away after a short period of time.
- Intestinal bleeding, which develops in 0.1% of cases.
- Respiratory arrest during the administration of anesthesia. Happens in about 0.5% of cases.
- After excision of polyps, the patient’s body temperature may rise to subfebrile levels. Abdominal pain may occur for 1-2 days.
If a person develops the following symptoms after a colonoscopy, they should contact their doctor immediately:
- Weakness appears.
- Performance decreases.
- My head is spinning.
- I have a stomachache.
- Vomiting begins.
- Diarrhea develops, in which blood impurities are observed.
- Body temperature rises to 38 °C or more.
Diagnosis of the large intestine
A blood test provides a lot of information about a person's health status.
To determine diseases of the colon, doctors prescribe a number of required examinations and tests.
Initially, a blood test is performed for clinical and biochemical composition. To determine dysbiosis, the patient submits stool to the laboratory. Five main techniques for examining the rectum:
- anoscopy;
- sigmoidoscopy;
- fibrocolonoscopy;
- laboratory diagnostics of stool for dysbacteriosis;
- blood analysis.
A digital rectal examination is necessary, which should be performed at any hint of pelvic organ disease. This procedure is carried out by a doctor using special devices.
To begin with, the condition of the anus muscles is analyzed, which will help identify a number of diseases: hemorrhoids, anal fissures, narrowing in the intestinal lumen, tumor formations, scars, and so on. In some cases, a rectoscope is used, which is necessary for diagnosing more deeply removed areas of the colon.
Colonoscopy and disease diagnosis
Colonoscopy makes it possible to assess the condition of the intestines from the inside, examine its mucous membranes, assess tone and other indicators. In some cases, the procedure allows you to avoid abdominal surgery. During its implementation, polyps can be removed, and a biopsy of altered tissues can be performed for further examination.
Diseases that require a colonoscopy:
- Diverticular disease.
With diverticulosis, there is a protrusion of the intestinal wall. The diverticula themselves resemble “sacs”. Translated from Latin, this term means “road to the side.” Feces accumulate and stagnate in these bags, which leads to the development of inflammation. Over time, the intestinal wall becomes thinner and becomes damaged, which leads to bleeding and even perforation. At first, the disease occurs without obvious symptoms; more than 80% of patients are not even aware of its development. Ultrasound for diverticulosis does not provide the necessary information. Pathology can be detected using colonoscopy, CT or irrigoscopy.
- Polyps and polyposis.
Polyps are benign neoplasms that have the ability to degenerate. Such tumors must be removed and further studied. Polyps most often do not show themselves, although they may bleed. When they reach large sizes, a person experiences abdominal pain.
If a patient is diagnosed with familial polyposis, accompanied by the appearance of a large number of tumors, resection of part of the intestine may be required. Polyps can be visualized during an MRI or CT scan. However, only with the help of colonoscopy the doctor has the opportunity to remove them, or take part of the tumor for further histological examination.
- Ulcers.
Colonoscopy can detect even the smallest areas of damage to the intestinal mucosa.
- Colon cancer.
Colon cancer is the third leading cause of death among other cancers. The causes of tumors can be identified only in 1/4 of the patients. Patients with a hereditary predisposition are at risk. If the cancer has an advanced course and metastases to the liver, then no more than 0.1% of patients survive over the next 5 years. When a tumor is detected at stage 3 of development, no more than 1/4 of people reach the five-year survival threshold.
If a tumor is detected at an early stage of development, the prognosis is most often favorable. Thus, detecting first-degree cancer can save the lives of 93% of patients. Colonoscopy can detect adenocarcinomas and other cancers in the early stages of development, perform a biopsy, and even remove some of them. The procedure is performed using a loop electrode.
- Nonspecific ulcerative colitis.
With this disease, inflammation of the intestinal wall occurs. It becomes covered with ulcers that bleed and secrete pus. The mild course of the pathology is characterized by redness of the intestinal mucosa, erosion and isolated areas of ulceration are visible on it. The vascular pattern is poorly expressed.
The severe course of the pathology is characterized by the presence of a large number of ulcers and areas of necrosis. A lot of pus and mucus are found in the intestinal lumen, there are areas of hemorrhage, and pseudopolyps and abscesses can form. All pathological changes can be detected during colonoscopy.
- Crohn's disease.
The disease is characterized by abdominal pain, severe diarrhea, and the appearance of anal fissures. The intestinal wall is thickened, reminiscent of a “cobblestone” appearance. These areas alternate with areas of ulceration, scar tissue, and fistulas. Crohn's disease can be diagnosed using a colonoscopy.
- Intestinal tuberculosis.
Intestinal tuberculosis develops in 70% of patients with pulmonary tuberculosis. Mycobacteria enter the intestines from the respiratory system. Diagnosis comes down to laboratory tests with a test for tuberculosis, X-rays of the intestine and colonoscopy with a biopsy of its tissue.
- Intestinal obstruction.
Colonoscopy allows you to clarify the nature of developing intestinal obstruction. Using a colonoscope, foreign bodies can be removed from the organ.
- Chronic colitis.
In chronic colitis, inflammation of the inner lining of the large intestine occurs. It undergoes degenerative processes. If the disease is advanced, then the walls of the organ suffer from atrophy.
Patients complain of abdominal pain, stool upset, nausea and loss of appetite.
Colonoscopy can detect the following types of disease:
- Typhlitis is a lesion of the cecum.
- Sigmoiditis is a lesion of the sigmoid colon.
- Proctosigmoiditis is a lesion of the rectum and sigmoid colon.
- Transversitis is a lesion of the transverse colon.
- Total colitis is a global lesion of the colon.
- Ischemic intestinal disease.
Ischemia and necrosis of intestinal tissue can develop in various diseases. This includes atherosclerotic vascular lesions, vasculitis, and vascular pathologies. Colonoscopy can be performed only according to strict medical indications, when the acute stage of the disease has passed. During the procedure, the doctor will find purplish-red areas, ulcers, hemorrhages, and strictures on the intestinal wall.
- Amyloidosis.
With amyloidosis, amyloid accumulates in the intestinal walls. This is expressed by abdominal pain, intestinal obstruction, constipation, and bleeding may develop. If the distal parts of the organ are affected, a colonoscopy with a biopsy of the changed tissue is required. Amyloid will be found in them.
- Pseudomembranous colitis.
Pseudomembranous colitis develops during long-term treatment with antibiotics. In this case, convex plaques with a yellowish tint will be visible in the intestines. They are an accumulation of fibrin, leukocytes and dead epithelium.
- Diverticula.
Saccular formations can form in a person throughout life, or be present from birth due to weakness of the connective tissue. When sick, a person complains of abdominal pain, diarrhea and increased gas formation. Colonoscopy is performed only after the disease has passed the acute stage.
Alternative diagnostic methods
Other tests can also be used for the early diagnosis of malignant tumors of the colon:
- Fecal occult blood test (annually). The accuracy of the study is 62–79%. Out of 10 people with colon cancer, only 6-8 will test positive. False-positive results are possible if the patient has recently eaten red meat, foods rich in vitamin C, or is taking drugs from the group of non-steroidal anti-inflammatory drugs. If the test shows a positive result, endoscopy is required to clarify the diagnosis.
- Flexible sigmoidoscopy (every 5 years) is an endoscopic examination of the rectum and lower third of the colon. It is performed in the same way as a colonoscopy, but during it, a smaller part of the intestine is examined. Helps identify 70–80% of polyps and malignant tumors in the rectum and lower colon.
- Fecal DNA testing combined with stool occult blood testing (every 3 years). Can detect up to 92% of malignant tumors and up to 42% of precancerous conditions.
- Virtual colonoscopy (CT colonography) (every 5 years) - multislice computed tomography (MSCT), during which the colon is filled with air. The detection rate of tumors larger than 1 cm using this study is 94%, polyps measuring 6–9 mm is 65%. Polyps smaller than 6 mm are not detected. If a polyp is found during CT colonography, endoscopy will still have to be performed to remove it. [9,10]
An image taken during CT colonography
Thus, colonoscopy is the most accurate and informative method of screening for colon cancer, while it makes it possible to immediately carry out a biopsy and some therapeutic manipulations.
Alternative to colonoscopy
Diagnosticians have a number of techniques that, in some cases, make it possible to refuse a colonoscopy. They are available for sale and do not cause discomfort in patients, but their information content varies.
- Irrigoscopy.
This method began to be used back in the 60s of the last century. During the procedure, the intestines are filled with air or a contrast agent, which is visible under X-rays (barium is used for this purpose). The doctor then takes a picture using an X-ray machine.
The preparation stage for irrigoscopy does not differ from the preparatory measures carried out during colonoscopy. Most often, such a study is prescribed to patients who are suspected of congenital elongation of the sigmoid colon (dolichosigmoid colon).
A person will need to cleanse the intestines and follow a diet so that the study is as informative as possible. During the procedure, a special device that resembles an enema is inserted into the patient's intestines. With its help, the lumen of the organ is filled with a contrast agent, after which the first image is taken. The patient will need to change body position several times to clear the intestines from all sides.
- MRI.
MRI can be performed as an auxiliary examination method, since it is difficult to assess the internal state of the intestine with its help.
MRI using a contrast agent makes it possible to qualitatively study the condition of the small intestine, detect tumors, polyps and areas of inflammation present in it. However, small lesions in the walls of the organ cannot be visualized.
- Sigmoidoscopy.
This procedure allows you to examine the lower part of your large intestine. To do this, use a device in the form of a metal tube that supplies air and has a flashlight. It is inserted into the rectum, just like a colonoscope.
Using this tube, you can not only examine the condition of the intestines, but also cauterize existing tumors, collect altered tissues, remove polyps, and stop minor bleeding.
Contraindications to sigmoidoscopy are similar to those for colonoscopy. Before the procedure, you need to follow a diet and perform intestinal cleansing.
- CT scan.
Computed tomography is one of the most informative alternatives to colonoscopy. The procedure allows you to assess the condition of the intestines without introducing additional devices into the patient’s body.
With a CT scan, the doctor takes a series of layer-by-layer photographs of an organ, which allows the doctor to identify a pathological area or tumor. However, the doctor will not be able to do a biopsy. Therefore, if a cancerous process is suspected, a colonoscopy will be required.
During the procedure, the patient is placed on a table, and the tomograph rotates around him. The device detects x-rays that pass through the body's tissues. The received data is processed and converted into a picture, which the doctor studies.
- Virtual colonoscopy.
This study is a modern alternative to CT. Using a special program, a 3D image of the intestines is displayed on the monitor. In this case, the patient will not require anesthesia or sedation.
This method has a significant drawback - during its implementation, the doctor cannot perform a biopsy of low-lying tissues or perform any manipulations with the organ.
In addition, the tomograph will not detect small polyps (up to 5 mm in diameter), as well as flat tumors.
- Endoscopic examination (esophagogastroduodenoscopy, endoscopy).
This hardware procedure is implemented using a probe. The method makes it possible to assess the condition of the small intestine, esophagus and stomach. It is prescribed for suspected ulcerative processes in the gastrointestinal tract. If polyps or tumors are found, a biopsy can be performed.
- Capsule study of the intestines.
This is a modern diagnostic method for examining the intestines, which was developed in Israel. On an empty stomach, the patient is asked to take a capsule that has a video camera. Before the procedure, the patient is assigned a special device that will record. The capsule naturally moves through the digestive organs, after which it is excreted along with the feces. If the intestines contract weakly, or there are areas of narrowing in it, use a capsule with a microchip.
After entering a narrow area, the capsule dissolves and the microchip is fixed in the problem area. It is then eliminated from the body.
This is a simple and informative, but expensive method of examining the intestines. It does not require the patient to make any lifestyle changes.
- Ultrasound.
Ultrasound is the most comfortable examination method. Assessment of the condition of the intestine is carried out using ultrasonic waves.
The patient will have to lie on the table, while the doctor moves the sensor over the skin of the abdomen.
Sometimes the procedure is performed using contrast. First, an ultrasound is performed without a contrast agent, then with it, and the third time after it is removed.
Ultrasound can be performed using an endorectal probe, which is inserted into the rectum. The method is indicated for suspected intestinal cancer.
Video: Maryana Abritsova, a coloproctologist surgeon, will tell you how you can replace a colonoscopy:
Irrigoscopy
The procedure consists of injecting a contrast agent into the large intestine (barium enema) and taking x-rays in several projections.
This allows you to accurately localize pathological areas of the intestine, detect peristalsis disorders, diverticulosis and other diseases. Irrigoscopy is safe, painless and does not take much time.
The main disadvantage of irrigoscopy is its low information content. There is also a fairly high probability of receiving false data when part of the intestinal contents is mistaken for a tumor or other pathology. As a result, a colonoscopy will still be required to clarify the diagnosis.
Colonoscopy during pregnancy
Sometimes colonoscopy is recommended for pregnant women. Pregnancy is not an absolute contraindication to the study, but the reason for prescribing it must be compelling.
The fact is that the procedure can cause some complications, including:
- Increased uterine tone.
- Dilatation of the cervix.
- Oxygen starvation of the fetus, etc.
Therefore, experts insist on undergoing a colonoscopy only if there are vital indications for this and there is no other alternative other than abdominal surgery.
For example, a colonoscopy may be prescribed for women who had Crohn's disease or ulcerative colitis before pregnancy, and who developed diarrhea in the early stages of pregnancy. Doctors may perform a colonoscopy to distinguish between a functional bowel disorder and a relapse.
In order not to harm the health of the child and not to provoke an abortion, the woman is not given intravenous anesthesia, limiting herself to local anesthesia.
Features and advantages of MRI technology
MRI examinations are actively used to identify pathologies in the retroperitoneal space, malfunctions of the gallbladder, pancreas, and intestines.
When considering whether to have a colonoscopy or whether to opt for an MRI, consult with your doctor. Magnetic resonance imaging has a lot of advantages; it is based on the phenomenon of magnetic resonance. The force field changes the position of hydrogen atoms in water molecules. Complex circuits are used to process the signal, resulting in their transformation into a series of layer-by-layer images.
Which type of diagnosis is better?
It is impossible to unequivocally answer the question of which type of diagnosis is better: intestinal ultrasound or colonoscopy, for the simple reason that these two examination methods simply cannot be compared in terms of effectiveness and significance. They have completely different purposes. Each of the methods can be used only if there are certain indications, and the final decision on prescribing one or another diagnostic method can only be made by a doctor.
However, most often, patients are initially prescribed ultrasound diagnostics, and if it turns out to be uninformative, then after this the patient is sent for a colonoscopy.
Small bowel cancer
Small intestinal cancer causes pain and problems with intestinal patency that disappear.
Colorectal cancer (cancer of the small intestine) is often very difficult to identify. This disease may be hidden behind the mask of another pathology; doctors need to work hard to identify it.
The main signs of small intestine cancer are persistent pain in the abdomen and problems with intestinal patency. Especially if the pain is increasing in nature, then it is necessary to schedule one or more examinations.
Bowel cancer may be present even if the ultrasound is negative. Since cancers are often hidden, doctors often fail to see them the first time.
Many, in order to unambiguously determine the presence of the disease, turn to specialists in Israel and Germany for help, since they have the most modern techniques and equipment. If there is even the slightest suspicion of a cancerous tumor, then examinations will have to be continued until a definite diagnosis is known.
In addition to the diagnostic methods already mentioned, there is a procedure called enteroscopy. This procedure involves an endoscopic examination, sometimes accompanied by a biopsy.