Colonoscopy refers to endoscopic techniques for modern diagnosis of various pathologies of the large intestine.
Thanks to this method, doctors can determine the presence of inflammatory processes, benign and malignant neoplasms, as well as ulcerative lesions of the colon mucosa already at the initial stage of development.
Colonoscopy can examine more than just the intestines. This technique has other advantages. Modern equipment allows doctors to perform a biopsy simultaneously with the examination.
To achieve optimal visualization of the mucosa, it is necessary to properly prepare the patient for the procedure. Cleanse the intestines, relax the intestinal tone as much as possible, and prepare mentally.
Why is an intestinal colonoscopy prescribed?
Colonoscopy allows you to examine the condition of the mucous tissue of the colon, and in 80–90% of patients the colon can be examined along its entire length. The doctor pays attention to the color, surface character, shine, vascular pattern and the overlap of the mucous membrane.
During the examination, it is possible to carry out various medical procedures, for example, collecting material for histological examination, taking smears and scrapings from the mucous membrane, removing benign neoplasms and foreign objects, stopping bleeding, restoring patency (required when the lumen is narrowed).
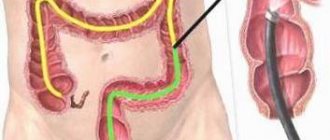
Colonoscopy allows you to detect neoplasms in the colon in the early stages, determine nonspecific ulcerative colitis and Crohn's disease. The examination is carried out using a thin, soft, flexible fiber colonoscope or optical probe. The device is equipped with a video camera, from which an enlarged image is transmitted to the monitor. Recording the procedure makes it possible to re-view the progress of the study and evaluate the dynamics of the pathological process.
Such anatomical characteristics of the structure of the colon, such as its length, the presence of bends and a large number of loops, do not allow the entire colon to be examined in some patients. In addition, before the study, it is necessary to thoroughly cleanse the intestines of feces, otherwise the information content is greatly reduced. During the procedure, patients may experience pain and psychological discomfort. All these factors make intestinal colonoscopy a rather complex and time-consuming study.
No ads 1
An endoscopic examination of the intestine is prescribed if the patient has the following symptoms:
- rapid weight loss;
- pain in the lower abdomen;
- discharge (mucus or blood) from the rectum;
- bright red blood or mucus in the stool;
- chronic inflammation of the lower gastrointestinal tract;
- chronic constipation or diarrhea.
In some countries, screening is mandatory if patients are over 40 years of age or if there is a family history of diagnosed colon cancer.
Contraindications
Like any diagnostic method, colonoscopy has a number of contraindications, and it can cause serious complications.
So, the main contraindications are:
- an acute infectious process that causes an increase in body temperature and intoxication;
- serious diseases of the cardiovascular system (heart failure, myocardial infarction);
- presence of artificial heart valves;
- a sharp and persistent decrease in blood pressure;
- pulmonary dysfunction;
- inflammation of the serous covering of the abdominal cavity of a local or diffuse nature;
- inflammatory processes in the intestines;
- ulcerative colitis;
- umbilical and inguinal hernias;
- violation of the blood clotting process.
Doctors also do not recommend performing the procedure on women during pregnancy.
If the patient has such contraindications, then he is prescribed an alternative diagnostic method.
Indications and contraindications for examination
Colonoscopy can be routine diagnostic, routine therapeutic or emergency. A routine diagnostic examination is carried out to determine the nature, location, extent and extent of changes in the tissues of the colon.
If required, the endoscopist takes samples for histological and cytological examination
The intestinal colonoscopy procedure is prescribed to patients for the purpose of:
- confirmation or establishment of an accurate diagnosis if the patient has signs of a malignant tumor in the colon;
- determining the morphology and degree of the tumor process in oncology;
- determining the nature, degree and extent of disorders in tissues caused by inflammatory processes;
- control and evaluation of the results of therapeutic measures for diseases of the colon, including after surgical treatment.
Examination of the gastrointestinal tract
Diagnostic colonoscopy is not prescribed for patients who:
- severe cardiac or pulmonary failure, hypertension or other somatic diseases in the later stages, in which the procedure may cause deterioration of the condition;
- nonspecific ulcerative colitis, Crohn's disease, diverticulitis and other severe pathologies that can cause serious complications during the procedure (bleeding, rupture of the intestinal wall);
- diffuse purulent peritonitis;
- fistulas that are at the stage of formation.
If the patient has acute inflammatory pathologies of the anal or perianal area (anal fissure, paraproctitis, thrombosis of hemorrhoids), an abscess, limited inflammation of the peritoneum, fistulas or the early postoperative period, then the decision to perform the procedure is made by the doctor, taking into account all the risks and expected benefits.
Therapeutic planned colonoscopy is prescribed in the following cases:
- there is a suspicion of the development of an oncological process in the colon;
- polyps were found in the proximal parts;
- During rectoscopy, polyps were detected in the rectum;
- diffuse polyposis was detected;
- hemorrhage in the rectum (blood in the stool is bright red);
- X-ray showed a colon tumor;
- nonspecific ulcerative colitis, Crohn's disease, which are not severe;
- there is an inflammatory-dystrophic process in the intestines and to clarify the diagnosis it is necessary to conduct a histology of the affected area.
Therapeutic planned colonoscopy is not performed if the patient has an exacerbation of ischemic colitis, acute corrosive lesions (burns) and there is a risk of perforation, severe heart or pulmonary failure, severe Crohn's disease or UC. Relative contraindications are diseases of the anal area with severe pain, the early postoperative period, mental disorders, and large hernias.
In some situations, an emergency colonoscopy is required. An examination is prescribed to determine the causes of obstruction of the large intestine, remove a foreign body, identify the source of bleeding and determine its severity. The doctor decides on an individual basis whether the examination can be carried out.
Is it necessary to do a video colonoscopy?
An examination is prescribed only if there are compelling reasons for conducting this type of diagnosis. This is one of the few procedures that allows you to detect changes in the mucous membranes of the large intestine and rectum at the earliest stages. In addition, simultaneously with the examination, you can remove the detected tumors or take their fragments for analysis. This type of diagnosis is recommended for patients with an increased risk of developing polyps or cancerous tumors of the colon and rectum.
Theoretically, video colonoscopy can be replaced by irrigoscopy (x-ray of the intestines using a contrast solution), capsule endoscopy or virtual colonoscopy (examination of the intestines using a tomograph). The listed procedures are less uncomfortable, but do not make it possible to take a biopsy from colon tumors for subsequent histological examination. They are used when colonoscopy is impossible due to intestinal obstruction or other contraindications, as well as to clarify the diagnosis.
You can find out doctors' opinions about the benefits and effectiveness of video colonoscopy from the following video:
How is polyp removal performed?
During colonoscopy, material can be collected for histological examination. Studying samples allows us to determine the disease and assess the degree of inflammatory changes. Most often, a therapeutic colonoscopy is performed if benign neoplasms (polyps) are detected in the large intestine.
At least 5–6 samples are taken from different parts of the affected intestine for histology
These formations can be seen on an x-ray (they look like a spherical, mushroom-shaped or branched growth on a stalk or on a wide growth). A single polyp is removed by electrocoagulation, mechanical biting, injection of sclerosants into the formation, hot biopsy, electrical excision or photocoagulation.
Whenever possible, it is recommended to use the electroexcision technique as it allows the sample to be viewed under a microscope. Mechanical biting can provoke bleeding, and burning out the polyp (electro- and photocoagulation) excludes histological examination. A diathermic loop is placed over the growth, and then the loop is tightened a little, which provokes ischemia of the tissue of the formation and thrombosis of the vessels of the pedicle.
When the loop is tightened, the polyp is lifted above the intestinal mucosa and a shock is applied to the loop. Electroexcision involves alternately cutting off the stem and cauterizing it. After removing the polyp, the specialist examines the bed of the formation and, if necessary, prevents bleeding, and the neoplasm itself is removed and sent to the laboratory.
Our team of specialists
Block - Doctors.
Do not edit this block, the data will be loaded automatically 4. Surveys
To undergo a colonoscopy under sedation, you need to have in your hands:
- results of blood tests for hepatitis B, C, HIV and RW for a period of no more than 1 month,
- electrocardiogram for a period of no more than 1 month,
- results of previous FCS (if available),
- results of additional examinations prescribed by the doctor (general and/or biochemical blood tests, coagulogram, etc.).
If necessary, all examinations can be completed in the clinic immediately before the FCS.
In general, preparation for an intestinal colonoscopy procedure under sedation is not much different from the classical one. Intravenous sedation, unlike traditional anesthesia, does not imply any additional restrictions and in most cases is easily tolerated by patients.
Read more about how to prepare for a colonoscopy in this article.
Preparation
The information content of a colonoscopy directly depends on the quality of the patient’s preparation for the procedure. In order to prevent flatulence, the patient must exclude from the diet three days before the procedure any foods that lead to flatulence or increase the volume of feces (fresh vegetables, fruits and berries, legumes, black bread, greens, smoked meats, pickles, pearl barley, oatmeal, millet porridge, chocolate, milk, coffee, carbonated and alcoholic drinks).
You can prepare for the test at home. On the eve of the study, the patient can have lunch and dinner, and in order to thoroughly cleanse the intestines of feces, he needs to drink 40–60 g of castor oil or a 25% solution of magnesium sulfate (magnesia) at approximately 16 o'clock, and at 21 and 22 o'clock do 2 cleansing enemas (volume of infused liquid is 1.5 liters).
Magnesia has a laxative effect because it increases osmotic pressure in the intestines, which leads to fluid accumulation, dilution of intestinal contents and increased motility. On the morning of the colonoscopy, the patient is given two more enemas no later than two hours before the procedure. If the cleansing procedure is carried out earlier, then sufficient cleansing is not ensured, and if later, the condition of the mucous membrane changes.
If the patient suffers from constipation, then a diet is prescribed 3-5 days before the examination. Vegetables and fruits, herbs, potatoes, berries, mushrooms, brown bread, legumes are prohibited, and laxatives are also prohibited. On the eve of the study, the intestines are cleaned until clean rinsing water comes out.
Colonoscopy is performed on an empty stomach
If the patient has symptoms of intestinal obstruction, then taking laxatives is contraindicated. The intestines are cleansed using siphon enemas (the procedure requires about 12 liters of water), which are done an hour before the examination. If there are no contraindications, the intestines can be prepared for examination by drinking a laxative.
The following drugs can be used:
- Fortrans. Retains water molecules in the intestines, thereby increasing the volume of intestinal contents and accelerating its movement through the intestines. One sachet of powder is dissolved in a liter of water, this dose is calculated for 15–20 kg of body weight (if your body weight is 60 kg, then you need to drink three liters of solution). It is recommended to use the drug the night before in one dose, or divide the solution into several parts and drink them at intervals of 15 minutes;
- Endofalk. Retains water in the intestines and also prevents gas formation. You need to drink three liters of solution in portions of 200–300 ml at intervals of 10 minutes in the evening before the test. Contains fruit flavor;
- Fleet Phospho-soda. The contents of two bottles (45 ml each) must be dissolved in 240 ml of boiled water. The solution should be washed down with 200–400 ml of water. If you take a laxative the day before the test, you should not eat. Stool occurs between 30 minutes and 6 hours;
- Lavacol. One sachet should be mixed in a glass of warm water. In total, you need to drink three liters of solution, that is, use 15 sachets. You need to start drinking 18–20 hours before the colonoscopy, and drink a glass of prepared liquid every 15–20 minutes.
All laxatives have contraindications for use, so before giving preference to this method of cleansing the intestines, you should consult a doctor. Fortrans and Fleet Phospho-soda are available with a doctor's prescription.
Preparing for video colonoscopy
So that the doctor can visualize the mucous membranes of the colon and rectum, it is necessary to cleanse the intestines. To do this, 3 days before the start of the procedure, solid foods and foods high in fiber are excluded from the menu. Preference is given to boiled chicken, poultry, and lean fish. You can eat weak broth with pasta, cheese, dry biscuits and white bread. Alcohol, carbonated drinks and strong tea should also be avoided.
The evening before the examination, it is advisable to take a laxative (Fortrans, Lavacol, Endofalk). Eating should be stopped at least 12 hours before video colonoscopy is performed.
Important! The laxative and enema should be taken in such a way that the intestines are completely emptied by the beginning of the examination.
On the day of the examination, you should not consume food or any drinks. You are allowed to drink only clean water, but no later than 2 hours before the start of the procedure.
A week before the examination, you should stop taking blood thinning medications (Warfarin, Pradaxa, Clopidogrel, aspirin and others). It is important to inform your coloproctologist about regularly taking medications to normalize blood glucose levels, blood pressure, and medications containing iron. You may need to reduce your medication dosage a week before the test or stop taking it completely.
Technique
Fiber colonoscopes are conventionally divided into diagnostic and operational. Diagnostic tests differ in the length of the tube inserted into the intestine. They range from 65 to 175 cm. Short endoscopes are used if only the left part of the colon is to be examined, and long endoscopes are used to examine the entire colon (total colonoscopy).
There are pediatric colonoscopes with a tube lumen of up to 11 mm; they can be used to carry out the procedure even on small children. The choice of endoscope is influenced by the anatomical and functional characteristics of the colon. If the pathology has caused a decrease in tone and expansion of the intestinal lumen, then long endoscopes are used, whose diameter does not exceed 16 mm (normally, the diameter of the intestinal lumen in its various segments is from 4 to 7 cm).
In case of severe inflammation and after operations, it is recommended to use thin and short endoscopes. The patient is asked to lie on his left side and pull his knees towards his stomach. To ensure a painless procedure, it is recommended to relax as much as possible and breathe through your mouth. The endoscope is inserted into the anus.
To eliminate painful sensations during insertion of the device, anesthesia of the anal area can be performed with dicaine ointment, luan gel, cathegel or xylocaine gel. The active ingredient in anesthetics is lidocaine. When the colonoscope reaches the distal sigmoid colon, the patient is asked to lie on his back and in this position the apparatus continues to be advanced forward.
It is also possible to carry out the procedure under general anesthesia, however, its introduction is not advisable, since colonoscopy is not so painful
Since the sections of the large intestine differ in their anatomy and have characteristic features, the specialist accurately determines the location of the endoscope, as well as the localization and extent of the pathological process. To expand the intestinal lumen and smooth out its folds, air is introduced into the intestines, causing the patient to feel bloated.
After the examination, the gas is removed by the device and the discomfort stops. To control the advancement of the colonoscope in physiological curves, palpation of the abdominal cavity is performed. The duration of the study varies from 15 minutes to an hour, which depends on the anatomical features of the intestine and the need for additional medical procedures.
After the procedure, the patient is under the supervision of medical personnel for three hours so that possible complications can be quickly eliminated.
Possible complications
The information value of the study is reduced if the large intestine is not sufficiently cleansed. If feces remain on the walls, this complicates visual control over the advancement of the apparatus and prevents a thorough examination of the intestines. It is also difficult to examine the intestine due to anatomical congenital or acquired features (megacolon, adhesions, hernias, inflammation).
Some patients may experience severe pain when the mesentery is pulled. After removal of polyps, abdominal pain and fever up to 37.2 0C may appear. Colonoscopy can cause serious complications such as bleeding or perforation of the colon. To exclude the occurrence of such complications, the doctor should carefully monitor the progress of the device and not push the colonoscope through the colon.
To exclude serious bleeding, it is necessary to determine the rate of blood clotting before the planned removal of the polyp. If, after the examination, weakness, dizziness, nausea, vomiting, bloody diarrhea, or low-grade fever appear, then you should urgently seek medical help.
Description of the procedure
Video colonoscopy of the intestine is considered the most informative method for diagnosing diseases of the rectum and colon, which allows real-time visualization of benign and malignant neoplasms, determining their size and location, taking biological material for analysis (biopsy) or removing tumors.
During diagnosis, the endoscopist uses special equipment - a video colonoscope. It consists of a thin flexible tube, at one end of which there is a miniature video camera and a light source. A tube for air supply is also attached to this end (this is required to straighten the folds of the intestines for a better view). In addition, the colonoscope can be equipped with additional parts that are used to take a biopsy for subsequent tissue analysis.
Video colonoscopy is prescribed if there are symptoms indicating pathologies of the colon and rectum:
- chronic constipation and diarrhea;
- rectal bleeding;
- chronic abdominal pain;
- sensation of a foreign object in the rectum;
- discharge of mucus from the rectum;
The examination is also indicated for patients at risk for cancer of the rectum and large intestine: men and women over 50 years of age, as well as those who have previously been diagnosed with polyps of the colon and/or rectum.
Reviews
Many patients ask if a bowel exam is painful. Reviews of the procedure are varied. Some talk about psychological discomfort, some actually feel pain, and some say they experienced more fear than pain. Here are some reviews.
Demetrius84: At first I felt a slight swelling without pain, because apparently they were pumping air. The doctor then began inserting the cord while holding an object that looked like a remote control in his other hand. He used it to pump and deflate air, and also controlled the endoscope (as I understand it). As it turns out, my intestines are very tortuous, especially before the first bowel turn. The doctor struggled with it for a long time, but the cord would not go through. It was unpleasant, even painful, but as soon as the pain became unbearable, the doctor pumped out the air and heavenly relief came. After giving me a little rest, the doctor continued the procedure.
Grigory: I won’t say that it was very painful. More like a couple of painful moments out of about 5-10 minutes (I can’t say more precisely) of this whole procedure, during which you have to turn over several times in different positions until the 1.2-1.5 meters of the endoscope reaches the end of the large intestine. I didn’t even expect, after so many stories, that the intestinal examination procedure would be so easy.
Turambar: It doesn't hurt. At all. The advancement of the colonoscope is not felt at all. But the intestine, as you know, has three turns. It will be a little painful when turning. Nature of pain: stomach twists, as if you haven't been to the toilet for a long time. That's not fatal. And it doesn’t look like the feeling of “being cut with a knife from the inside” (review on the internet). The pain lasts until the colonoscope turns. In my case, the first two turns take 5 seconds, the third - 10 seconds. After about 5-10 minutes, the colonoscope will reach the end.
If intestinal colonoscopy is performed correctly, it is a safe, painless and informative examination. There is no other method to visually assess the condition of the intestinal mucosa without resorting to surgery.
What happens after video colonoscopy
After a video colonoscopy has been performed, the patient may experience abdominal discomfort in the form of bloating or colic for some time. In some cases, a small amount of blood may be released from the anus.
Important! If the bleeding has not stopped within 24 hours, the body temperature has risen, the pain and cramps in the abdomen do not subside, you should contact the doctor who conducted the examination again.
After a video colonoscopy, you should abstain from eating for some time, especially if a biopsy was taken during the procedure or the doctor removed polyps. During the first hours you are allowed to drink a small amount of water or warm tea. For 2-3 days you should follow the following diet:
- eat jelly, slimy porridges and soups, pureed vegetables and cereals;
- drink warm tea without sugar, jelly, fresh (daily) kefir and other fermented milk drinks;
- eat steamed meat (veal, poultry fillet, beef), lean fish;
- as a side dish, cook boiled vegetables or puree them, pureed porridge in water;
- For breakfast and dinner there are steamed omelettes, pureed non-sour cottage cheese, soft unsalted cheeses.
Exclusions from the menu include rich broths with lots of vegetables, fatty meats, fresh vegetables and fruits, pickles and pickled vegetables, jams and preserves, berries with small seeds and seeds, baked goods and rye bread.