Benign diseases of the colon do not pose a serious threat to the patient's life. Despite this, such diseases require careful treatment. A benign tumor of the rectum, in the absence of proper therapy, often degenerates into oncology.
There are many types of neoplasms, the most common being polyps, lipomas, and leiomyomas. They are formed from mucosal tissue, adipose tissue or smooth muscle fibers of the intestinal wall. There are other rarer types of benign tumors.
Reasons and background
At the moment, experts cannot establish the exact cause of the formation of a benign colon tumor and talk about known risk factors: poor diet, bad habits, and lack of physical activity. Hereditary dependence has been precisely established only for polyposis, however, any of the risk factors can trigger the development of the disease.
At CELT you can get a consultation with a proctologist.
- Initial consultation – 3,000
- Repeated consultation – 2,000
Make an appointment
Types of malignant intestinal tumors by location
Cancers are diagnosed in different parts of the intestine and have an extensive classification. When dividing cancer tumors into types, their histological composition, form of development and localization are taken into account.
Depending on the location, intestinal cancers are classified into:
- ampullary tumors - this type is represented by a crater-shaped bleeding ulcer with an infiltrated base, exophytic adenocarcinoma; occur in 80% of cases of detected malignant neoplasms of the rectum;
- supramullary tumors - represented by scirrhus, which narrows the intestinal lumen in the form of a ring and leads to the development of stenosis; occur in 15% of cases of detected rectal cancers;
- anal tumors - affect the anus, forming a dense ulcer with a squamous structure; occur in 8% of cases of diagnosed rectal tumors.
A detailed classification of intestinal cancer tumors, depending on the location in a particular part of the intestine, is as follows:
Tumors localized in the small intestine are diagnosed quite rarely - 1% of the total number of cases of gastrointestinal tumors. This is due to the rapid passage of food through this section, which contains a lot of immunoglobulin A. Sarcomas, lymphomas, carcinoids, and adenocarcenomas can develop in the small intestine. The prognosis of a small intestinal tumor will depend on the presence of metastases. In the absence of metastatic foci, the patient has a good chance of successful treatment. If the tumor begins to spread and metastasize, then adjacent sections - the large intestine and stomach - are affected. In this case, gastric cancer will be treated abroad, as well as other organs that have metastasized.
Small intestine.- Colon. Frequent localization in which the mucous membrane is affected. As the tumor spreads, layers of the wall grow and adjacent organs are affected. As a rule, adenocarcinomas develop in the colon.
- Duodenum. The main location of tumors is the descending region. In 15% of cases, cancer pathology is accompanied by metastasis. Moreover, metastasis to organs occurs in a certain sequence. The lymph nodes are affected first, then the liver and then the lung tissue. Patients with metastatic bowel cancer often undergo treatment for lung cancer abroad.
- Ascending colon. Cancerous tumors are detected in 18% of cases of the total number of formations of the thick section. Such tumors are characterized by late metastasis.
- Descending colon. Rare localization, accounting for no more than 5% of cases.
- Sigmoid colon. Tumors occur in 25% of cases.
- Transverse colon. The formations are rare - 9% of cases of all identified tumors of the large intestine.
- Rectum. Frequent localization of malignant tumors - 40% of cases (adenocarcinoma). At the same time, the number of detected cases of colorectal cancer increases every year. The tumor can develop in different directions, affecting the lumen of the wall or its thickness.
- Cecum with appendix. A fairly common location is in the cecum. The appendix is less often affected by cancer; as a rule, carcinoid tumors form here, which grow slowly and practically do not affect the serous membrane.
- Colon. Speaking about the localization of tumors in a given intestine, experts generalize the formations that arise in different subsections of the large intestine.
Malignant tumors, regardless of location, pose a serious threat, so measures to combat them must be carried out in a timely manner.
Symptoms and risks
Benign neoplasms of the large intestine can be asymptomatic or characterized by the following symptoms:
- Painful sensations in the intestinal area, in different parts of the abdomen.
- Frequent urge to defecate, often false.
- Slimy stool.
- An admixture of blood in the stool (usually indicates the rapid development of the disease and a significant size of the tumor).
The main difficulty is that symptoms appear only as the tumor grows; in the early stages they are invisible. By the time the patient seeks help, the tumor usually reaches several centimeters.
Doctors evaluate the symptoms, send the patient for examination and prescribe treatment based on the clinical picture. It is important to determine the type of tumor, since some types of benign neoplasms carry a high risk of developing cancer. There are tumors that have virtually no risk of malignancy.
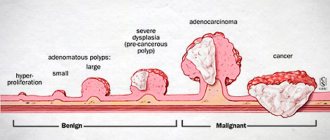
Most often, malignant tumors develop against the background of tubular adenoma. Other forms can also develop into cancer if left untreated. There is a simple rule: the larger the size of the polyp, the higher the risk of developing cancer.
In general, treatment of a benign rectal tumor is aimed at rapid and complete removal of the polyp and minimizing the risk of oncological complications.
Nonepithelial tumors
Nonepithelial benign colorectal tumors are rare and account for approximately 3% of all benign colorectal tumors.
Smooth muscle tumors of the colon (leiomyomas and leiomyosarcoma) account for 0.2-0.4% of benign and malignant neoplasms of this organ.
Pathogenesis and pathological anatomy. The source of development of leiomyoma can be the smooth muscles of internal organs (gastrointestinal tract, bronchi, uterus, ovaries), and vascular walls. Leiomyomas occur at any age in people of both sexes, most often at the age of 30-50 years.
Macroscopically, the tumor is a clearly demarcated node of dense consistency, surrounded by slightly sclerotic tissue, which creates the impression of encapsulation. The size of the tumor is very different, but not more than 5 cm (in the gastrointestinal tract, in the skin), but in the retroperitoneal tissue space, the mediastinum can easily reach 15-20 cm.
Microscopically, leiomyoma consists of spindle-shaped tumor muscle cells that are collected in bundles running in different directions.
The sources of development of leiomyosarcomas are the same as those of leiomyomas. Gender and age do not matter. It is extremely malignant: early hematogenous metastases usually occur, relapses after removal are rare.
Macroscopically, the tumor has the shape of a node with a diameter of 15-20 cm or more. The cut surface is mottled due to the presence of foci of hemorrhage, areas of necrosis and tissue melting.
The microstructure is varied. Typical leiomyosarcomas are characterized by great similarity to leiomyomas. Only when examining the peripheral parts does the infiltrating growth of the tumor become apparent, which does not push back the tissues, like leiomyoma, but infiltrates and destroys them.
The occurrence of leiomyosarcomas due to malignancy of mature tumors is not observed in most cases, but exceptions are possible.
The clinical manifestations of benign and malignant smooth muscle tumors are very similar and differ little from each other. These formations are characterized by the following symptom complex: pain, blood and mucus in the stool, a feeling of discomfort and a foreign body in the rectum and anus, weight loss, and constipation. Thus, the clinical signs of these tumors also differ little from the clinical manifestations of benign and malignant tumors of the colon.
Differential diagnosis of smooth muscle tumors of the colon in the preoperative period is very difficult. Based on a complex of diagnostic methods (digital, endoscopic, x-ray, ultrasound, biopsy), the correct preoperative diagnosis can be established only in a small number of patients.
Most leiomyomas are characterized by a small tumor size (up to 5 cm), dense elastic consistency, quite
clear boundaries and absence of infiltrative growth, mobility in relation to surrounding organs and tissues.
Leiomyosarcoma is characterized by a large tumor size (15-20 cm or more), the boundaries of the formation are not differentiated, the tumor is practically not displaceable due to the pronounced extraintestinal component, the intestinal mucosa is often involved with the formation of areas of ulceration and hyperemia.
The most reliable and informative data for the differential diagnosis of leiomyomas and leiomyosarcomas were obtained by ultrasound, especially when using an endointestinal sensor.
The following radiological signs are characteristic of leiomyomas: a central or marginal filling defect with a mild intraluminal component, round in shape with clear boundaries, the mucous membrane over the formation is not changed.
With leiomyosarcoma, the following radiological signs are revealed: large size (more than 10 cm), a sharp transition of the contour of the filling defect into the unchanged parts of the rectum, uneven or unclear contour of the filling defect and signs of germination into the intestinal mucosa, which is manifested by breakage of folds and loss of elasticity.
Microscopic examination, unfortunately, cannot always give a clear answer about the malignancy of leiomyoma.
Treatment. For small rectal leiomyomas (up to 1.5 cm), the operation of choice is electroexcision of the tumor through an endoscope. For large formations (up to 5 cm) of the lower ampullary rectum, organ-preserving surgery using transanal or perineal-anal access is indicated; if located in the rectovaginal septum, transvaginal surgery is indicated. The presence of large leiomyoma (more than 5 cm) is an indication for abdominal surgery - anterior and abdominal-anal resection of the rectum.
For leiomyosarcoma, the choice of surgical intervention is determined by the degree of malignancy of the tumor and its location. It is possible to perform abdominal-perineal extirpation, abdominal-anal and anterior rectal resections. The presence of high-grade leiomyosarcoma is an indication for rectal extirpation, regardless of the level of tumor location.
The prognosis for leiomyomas is quite favorable. The relapse rate is within 25%, the malignancy index is 20%. The 5-year survival rate of patients averages 85%.
With leiomyosarcoma, the relapse rate is slightly higher - 30% and the 5-year survival rate is significantly lower, which averages 60-70%.
Of nonepithelial tumors, lipomas are the most common. They are recognized during endoscopic examination by the characteristic yellowish translucency through the unchanged mucous membrane. They have a soft consistency with smooth rounded contours. Typically, lipomas do not tend to grow and cannot be treated. However, for large sizes, which can lead to disruption of passage through the colon, surgical treatment is necessary.
Carcinoid is an argentaffinoma, a tumor originating from the diffuse neuroendocrine system of the gastrointestinal tract. The disease is observed very rarely - less than 0.5% of cases. The location of the carcinoid is most often in the appendix, but small formations are found in the distal parts of the colon. With appendicular carcinoid, the carcinoid syndrome typical of other localizations of this tumor (tachycardia and redness of the skin of the upper torso) is almost not observed.
Pathomorphology. Carcinoid consists of the same type of cells with the same type of nucleus. The tumor can be single, rarely multiple. The carcinoid is located in the submucosal layer, has a dense consistency, is yellowish in color when cut, and usually does not exceed 2 cm in diameter. In the appendix, the tumor is usually localized in the apex and middle part. Colon carcinoids can metastasize. Currently, the most common idea is that carcinoid is a developmental defect, the basis of which is accumulation of enterochromaffinocytes (Kulchitsky cells). Carcinoid is of neuroectodermal origin. This is evidenced by the detection in carcinoids of serotonin produced by enterochromaffinocytes, a large amount of which, produced in malignant carcinoids, can cause the so-called carcinoid syndrome, expressed in a rise in blood pressure, hyperemia of the skin of the upper half of the body, and sometimes frequent loose stools.
Clinic. In most cases, there are no clinical manifestations. It is more often a finding during examination of the large intestine (rectoscopy, colonoscopy, irrigoscopy).
Treatment. Most often it is removed by electroexcision during endoscopic examination. The diagnosis is established after histological examination.
The prognosis is good, relapses practically do not develop.
Mesenchymomas of pararectal tissue are tumors of complex structure, consisting of derivatives of several types of tissue of mesenchymal origin. There are benign mesenchymomas, built from mature components of mesenchyme (angiofibrolipoma, rhabdomyofibroangiomyoma, osteofibrolipoma, etc.), and malignant, characterized by the presence of sarcoma in one or more tissue components. Macroscopically, mesenchymomas come in various sizes and shapes, but larger tumors with a capsule are more common. Their consistency is often homogeneous, soft-elastic, less often heterogeneous - alternating dense and soft areas. On a section, the tumor is usually gray-pink or brown in color with various shades. The color of the formation depends on the predominance of one or another tissue in its composition. The microstructure of mesenchymoma is characterized by a multicomponent tissue composition.
The clinical picture is determined by the size of the tumor and its location. These neoplasms are localized in the tissue of the pelvic cavity. The upper pole of the tumor may be located under the pelvic peritoneum, reaching the sacral promontory and paravesical tissue. The lower pole of the tumor can be located under the skin in the perineal area, deforming it, and is visible to the eye. The most common symptom is the formation of a visible or palpable tumor in the perineal area. Sometimes the first symptoms are urinary disturbances or partial colonic obstruction resulting from compression or confusion of the bladder or rectum.
Diagnosis of mesenchymomas of pararectal tissue is difficult. The study of complaints and anamnesis allows one to suspect the presence of a tumor. When palpated through the skin of the perineum, a tumor of soft consistency is determined, less often with areas of compaction. When examining through the anus, the sliding of the tumor along the posterior or posterolateral wall of the rectum is clearly felt. In addition, with mesenchymomas, a positive cough impulse and an increase in the visible part of the tumor when straining are observed.
Radiological research methods, one of which is parietography, are important in recognizing mesenchymomas. The information content of the method increases when supplemented with pneumorectography, tomography and urocystography (according to indications). In this case, it is possible to identify the connection of the tumor with surrounding organs and tissues. A special place in the diagnosis of mesenchymomas of pararectal tissue is occupied by selective angiography, which makes it possible to establish the localization of the tumor, i.e. the nature, sources of blood supply and connection with the iliac vessels. It is also necessary to use sigmoidoscopy and cystoscopy. It is possible to perform a percutaneous puncture biopsy, which often allows one to establish the histological structure of the tumor.
Mesenchymomas of pararectal tissue often have to be differentiated from perineal hernias, teratoid formations, leiomyomas, lipomas, and parasitic cysts.
Treatment. Surgical treatment of mesenchyme is a very complex intervention, since it involves significant disturbances in the topographic-anatomical relationships of the organs and structures of the pelvis. To remove mesenchyme from pararectal tissue, two approaches are used: perineal and abdominal-perineal. The choice of surgical approach depends on the location and size of the tumor. The perineal approach is advisable to use in cases where the upper pole of the pararectal tumor is located no higher than the promontory of the sacrum. The indication for the use of a combined approach is the high location of the upper pole of the formation - above the promontory of the sacrum.
Radiation and chemotherapy treatment of mesenchyme is ineffective.
The prognosis for malignant mesenchymomas is unfavorable.
Malignant lymphoma is a systemic disease that is sometimes localized in one area of the intestine over a relatively limited extent or predominantly affects the lymphatic tissue of large sections or the entire intestine and its mesentery.
This disease is rare and causes great difficulties in differential diagnosis with diseases such as cancer, ulcerative colitis and granulomatous colitis.
Pathological anatomy. Currently, it is generally accepted that malignant lymphoma is not an independent disease, but is a variant of diffuse lymphosarcoma or reticulosarcoma of the corresponding cellular composition. Proof of this is that as a result of the fusion of “follicles” in the same lymph node, one can see areas of both diffuse growth and the formation of follicle-like structures, as well as diffuse growth in one and follicle-like in another lymph node, even within the same group of enlarged lymph nodes. The cellular composition of follicular lymphomas corresponds to that in lympho- and reticulosarcomas with a diffuse growth pattern.
The clinical picture is characterized by nonspecific symptoms: intestinal bleeding, diarrhea, abdominal pain, often without clear localization, weakness, exhaustion, sometimes large tumors with clear boundaries are palpated through the anterior abdominal wall. Endoscopic examination and biopsy do not always make it possible to recognize the disease, especially with diffuse damage to the intestinal wall without damage to its mucous membrane. In this case, pallor and marbling of the mucous membrane, unevenness of the intestinal lumen, the presence of narrowings, lack of haustration, bulging of certain areas into the lumen, and wall rigidity are noted. If the blood supply to the mucous membrane is disrupted, ulcerations and inflammatory changes may occur against this background, accompanied by purulent and bloody discharge, fibrinous deposits and contact bleeding.
With contrast X-ray examination, recognition of this disease is very difficult due to the similarity of symptoms with Crohn's disease and ulcerative colitis, colon cancer.
Treatment. Surgical treatment is rarely indicated and is ineffective. Sometimes surgery is undertaken to establish a definitive diagnosis and justify subsequent chemotherapy and combined chemoradiation treatment.
The prognosis is unfavorable.
- -Crohn's disease
- -Epithelial coccygeal tract
- -Endometriosis of the colon Endometriosis of the colon
- -Irritable bowel syndrome
- - Familial adenomatosis of the colon
- - Rectal fistulas (chronic paraproctitis)
- -Rectocele
- -Rectovaginal fistulas
- -Colon cancer
- -Cancer of the anal canal
Establishing diagnosis
Currently, experts give preference to instrumental high-precision diagnostics. The most commonly used are colonoscopy and sigmoidoscopy, during which a diagnostic biopsy of the identified formation can be performed. To clarify the extent of the process, irrigoscopy (x-ray of the colon) is also used.
In addition to instrumental diagnostics, a number of laboratory tests are required: blood tests; stool tests (coprogram, etc.), as well as ultrasound, MRI (if necessary). After an accurate diagnosis is made, therapy begins.
Reasons for education
The development of tubular adenoma of the colon is promoted by nutritional factors: high fat content and low dietary fiber. Changes in diet affect the likelihood of developing adenoma and adenocarcinoma. Refined fats can disrupt the proliferation of epithelial cells. Nutrient components found in fruits, vegetables and other foods can regulate colon carcinogenesis and influence the progression of adenoma to carcinoma.
The individual risk of developing colon adenoma increases in first-degree relatives of patients with colorectal cancer. The likelihood of developing colorectal carcinomas increases if a person has first-degree relatives diagnosed with colon cancer before the age of 50 years. The risk is especially great if these relatives are brothers or sisters. Environmental factors can interact with the genetic factors of the body, leading to the emergence or progression of “adenoma-carcinoma”.
An increase in the size of the polyp, the number of villi and severe dysplasia increase the risk of malignancy of colon adenoma. According to statistics, 4.8% of tubular, 22.5% of tubular villous and 40.7% of villous adenomas are converted into adenocarcinoma. The risk of transformation of benign neoplasms into malignant tumors increases with the degree of dysplasia. 5.7% of adenomas with mild dysplasia, 18% with moderate dysplasia and 34.5% with severe dysplasia transform into adenocarcinoma of the colon.
Villous, tubulovillous adenomas, and adenomas larger than 1 cm increase the risk of subsequent development of colon adenocarcinoma. This risk is higher in patients with multiple polyps.
Treatment and recommendations
Treatment for a benign colon tumor depends on the size of the polyp. Formations with a diameter of less than 5 mm do not need to be removed, but must be monitored over time. Larger polyps are removed during colonoscopy. If the polyp cannot be removed using a minimally invasive method, surgery is prescribed and the formation is excised along with part of the intestine.
If removal is not required, then therapy is prescribed individually. In some cases, the doctor adheres to observation tactics.
If any disturbing symptoms appear, you should consult a coloproctologist in order to diagnose and begin treatment in a timely manner. The CELT clinic employs leading experts in their field. Tactful and attentive doctors will prescribe all the necessary examinations, make an accurate diagnosis and help you successfully complete the course of treatment.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Types of malignant intestinal tumors by shape
Depending on the form of development, malignant tumors can be exophytic, endophytic and mixed. Different tissues are involved in the formation of tumors, so tumors differ significantly from each other.
- Colorectal formations. Tumors in which the ability to differentiate is almost lost. The cells of the tumor are very different from the cells of the organ in which the tumor is localized.
- Angiosarcoma. The tumor is formed from cells that are located on the internal vascular walls. It is characterized by aggressive growth and metastasis. Late stages of cancer are often accompanied by damage to the pelvic bone tissue, for which bone cancer treatment abroad is indicated.
- Leiomyosarcoma. A rare type of formation, the structure of which includes smooth muscle tissue. Often affects the small intestine.
- Malignant neurilemoma. The source of tumor formation is the neuroectoderm. The second name for such a tumor is schwannoma, since it begins to develop from a nerve root schwannoma. In some cases, schwannoma cells change greatly, making differentiation difficult. Accordingly, treatment in such situations is difficult to select. Specialists develop individual programs that are adjusted during treatment.
- Colorectal lymphoma. This is basically what is called adenocarcinoma, the structure of which contains glandular particles.
Other types of malignant tumors are also detected in the intestines: sarcoma, lymphoma, carcinoid tumor.
To develop an effective treatment program, it is important to determine the exact type of tumor, therefore, in foreign clinics, special attention is paid to the diagnostic stage.
What does colon cancer look like?
Doctors at the Yusupov Hospital collect material from a rectal tumor during an endoscopic examination or surgery and send it to the histology laboratory. Laboratory assistants determine the histological type of the tumor based on what colorectal cancer looks like.
Rectal adenocarcinoma consists of atypical cells that originate from glandular epithelial tissue and are formed into tubular, papillary and other structures. The cellular structure can have varying degrees of differentiation: highly differentiated neoplasms have cytological signs of maternal epithelial tissue, and poorly differentiated adenocarcinomas only vaguely resemble the original material. They are highly aggressive, grow and spread faster.
Mucous adenocarcinoma is a group of cells that are surrounded by mucus. Tumors of the mucous type can be poorly differentiated and highly differentiated. Mucus accumulates in tumor structures in the form of “lakes” of varying sizes
Signet ring cell carcinoma gets its name due to the shape of the cells, which, due to an excess of mucus in them and the displacement of nuclei towards the membranes, take on the appearance of a ring. The mucous substance that occupies the space of cells is a specific protein mucin. Signet ring cell tumors of the rectum are quite aggressive.
Squamous cell carcinoma of the rectum consists of atypical cells. They belong to the squamous intestinal epithelium. Pathological lesions contain intercellular bridges and keratin. Rectal squamous cell tumors can be keratinizing or non-keratinizing.
Glandular squamous adenocarcinoma is a rare type of rectal cancer. Such neoplasms are represented by adenocarcinoma, in combination with squamous cell carcinoma. Under a microscope, histologists see small fragments of squamous cell transformation.
Undifferentiated rectal tumors consist of atypical cells of epithelial tissue that do not form glandular structures and do not produce mucus. These cells represent different cytological structures. They form sheets or cords that are separated by a scant stroma of connective tissue.
Scirrhus is a cancerous tumor in which the connective tissue predominates over the stroma. Cytological structures in scirra are cubic cells collected in strands or small cells. Sometimes there are neoplasms in the rectum that do not fit into any histological type. In this case, oncologists talk about unclassified rectal cancer.
Neuroendocrine tumors of the rectum originate from cells of the diffuse neuroendocrine system. They have a well-developed fibrous stroma and are histologically different from adenocarcinomas.
Melanomas of the anal canal
They make up about 18% of all malignant tumors of the anal canal and almost 1.5% of melanomas of all localizations.
The clinical picture and diagnosis of melanomas of the anal canal are similar to those of squamous cell carcinoma of this area. Of the diagnostic procedures, special attention should be paid to biopsy (taking a piece of the tumor for examination). It is well known that melanoma biopsy is strictly contraindicated! However, almost all patients undergo a tumor biopsy before hospitalization, which significantly worsens the prognosis (outcome) of the disease.
Melanomas of the anal canal are usually pink in color, not black, like on the skin, and are not pigmented to the eye. Biopsy contributes to the generalization of the tumor process and worsens long-term treatment results.
At the slightest suspicion of melanoma of the anal canal, a less traumatic, but diagnostically no less informative method should be used - a cytological examination of fingerprint smears taken from the surface of the tumor.
Locally advanced forms of melanoma of the anal canal are much less common than with squamous cell carcinoma, but melanomas of this localization are characterized by early generalization of the process and distant metastasis.
Local recurrence after local excision of small melanomas is rare. This allows for small exophytic (outward growing) melanomas, especially those on the legs, to use a sphincter-preserving treatment method - cryodestruction (low temperatures).
For tumor sizes less than 3 cm, the use of cryodestruction is an adequate, radical method of treatment. However, local relapse is not observed in these patients.
Long-term treatment results for anal canal melanomas are generally unsatisfactory: the 5-year survival rate is 17%.
The difference between hemorrhoids and rectal cancer
Hemorrhoids and rectal cancer are proctological diseases that occur most often. How to distinguish hemorrhoids from colorectal cancer? You can independently determine the nature of the disease by the symptoms, but it is best to seek advice from the doctors at the Yusupov Hospital. Oncologists will conduct a comprehensive examination and differential diagnosis.
Hemorrhoids and rectal cancer have very similar symptoms and are well camouflaged. For a long period of time they do not manifest themselves in any way. A characteristic difference is the color of the blood. With hemorrhoidal bleeding, the blood is bright scarlet in color and practically does not mix with the feces. In cases of colorectal cancer, dark blood appears during bowel movements. It is evenly distributed in the feces.
Cancer and hemorrhoids are manifested by characteristic discharge. With pathological inflammation of hemorrhoidal veins, the mucus is transparent and does not have a pungent odor. A sign of rectal cancer is the presence of a foul-smelling, purulent substance in the stool, which appears not only during bowel movements.
With hemorrhoids, stool does not change shape. The growth of a malignant tumor, the gradual narrowing of the lumen of the anus contributes to the formation of ribbon-like feces. With hemorrhoids, patients deliberately refuse to eat because of pain during constipation or bowel movements, while they experience hunger and lethargy. With rectal cancer, the patient does not complain of poor appetite, but rapidly loses body weight.
Colon cancer
The following types of colon oncology are distinguished:
- Adenocarcinoma - originates in glandular cells that produce mucus to lubricate the inner surface of the intestine;
- Carcinoid tumor - arises from hormone-producing cells of the intestine;
- Lymphoma is a cancer directly related to disorders of the immune system;
- Squamous cell carcinoma develops from mucous membranes and epithelial tissue. Quickly grows into adjacent tissues and organs;
- Angiosarcoma - formed from fragments of the wall of blood vessels (hemangiosarcoma) or lymphatic vessels (lymphangiosarcoma).
Diagnosis of colon tumor, prognosis after treatment
Effective treatment of colon tumors with maximum guarantees of no relapse is possible only if cancer is detected in the early stages. Therefore, regular and complete diagnostics is a necessity. This is especially true for patients over 40 years of age.
One of the first tests to determine abnormalities is a stool occult blood test. It's a quick and easy way to keep your health under control. Older people, especially those at risk, are recommended to undergo this test annually.
A more detailed examination before starting treatment by a gastroenterologist includes:
- colonoscopy;
- irrigoscopy;
- CT and MRI to clarify the location of formations and metastases;
- Ultrasound diagnostics to determine the extent of damage to neighboring organs;
- biopsy (performed during colonoscopy);
- Laparoscopy or laparotomy is prescribed when other methods are insufficient.
After accurately determining the location of the tumor and metastases, the stage of intestinal cancer, the doctor prescribes appropriate treatment.
Treatment of malignant lesions in rectal cancer
Tomography - used to assess the condition of neighboring organs.
The main method of treatment is surgery in combination with chemotherapy and radiation therapy. This type of cancer responds well to drugs, so chemotherapy is carried out both before and after surgery. This helps improve survival and reduce relapse rates. Small tumors in the early stages are burned out using laser radiation.
Surgeries on the rectum are quite traumatic interventions and require careful preparation. If the tumor is small and located ten centimeters above the sphincter, then an anterior resection is performed, when the section of intestine with the tumor and regional lymph nodes are removed, and the remaining ends of the intestine are sutured. With this type of surgical intervention, the patient recovers quickly.
If the tumor is located lower (6 cm from the anus), then a low resection is performed, when part of the intestine, after removing the tumor, is brought out through the anus, they wait for the intestine to grow together, and cut off the removed intestine. In this case, the intervention due to the removal of a large section of the intestine is more traumatic; it is necessary to create a temporary path for defecation - a stoma.
At stages 2 and 3 of rectal cancer, a permanent colostomy is formed and the rectum is excised. Constantly wearing a colostomy bag is very inconvenient, so every effort is made to restore the natural process of defecation. At stage 4, intestinal patency is restored and nearby metastases are removed. If the process is accompanied by multiple metastases, then palliative treatment is carried out aimed at maintaining the life of the patient and alleviating his condition.
Risk factors
- The likelihood of detecting a tumor in yourself increases if the medical history of relatives already includes colon polyposis;
- Unbalanced diet: satiety with fatty foods, lack of vegetable and fruit components, legumes, whole grain bread, buckwheat and corn in daily dishes;
- Frequent constipation, especially those that were eliminated after the use of laxatives that irritate the mucous surface of the intestinal layer;
- Crohn's disease - inflammation of the colon mucosa with the appearance of numerous ulcers, diarrhea is much more pronounced than with ulcerative colitis, the presence of perianal lesions in the form of polyps and fistulas (inflammation in the recess of the anal mucosa, perirectal tissue or intersphincteric space);
- Hypodynamia - weakened motor tone;
- Age limit: over 50 years;
- Angiodysplasias are congenital malformations of blood vessels;
- Smoking;
- Nonspecific ulcerative colitis (UC) is a chronic diffuse inflammatory process of the mucous layer of the rectum and colon, which serves as an impetus for the formation of various ulcers of the mucous membrane.
Fact. The total length of the colon is approximately one and a half to two meters.
Diagnosis of precancerous diseases
A number of methods are used to detect precancerous diseases and even to diagnose colon cancer:
- Sigmoidoscopy - examination of the rectum and final sections of the colon. Using this method, polyps and tumors can be detected in the rectum and distal sigmoid colon;
- Irrigoscopy (link to x-ray page);
- Videocolonoscopy;
- Radiography;
- Ultrasound examination of the abdominal organs;
- CT (computed tomography);
- Complete blood test to determine the level of red blood cells and white blood cells;
- Endoscopy.