Indigestion is one of the most common ailments that force patients to seek medical help. Gastrointestinal pathology in children ranks second after respiratory diseases, and in adults, according to various observations, it ranks second or third.
In recent years, epidemiological studies in various countries have shown a rapid increase in the incidence of gastrointestinal diseases throughout the world. In some regions, especially in industrialized, "stressful lifestyles", these diseases are already at the forefront of prevalence statistics.
This was widely discussed at an expert symposium of the gastroenterology section of the European Union of Medical Specialists (UEMS). Research data presented at the event shows that in some Western countries, gastrointestinal diseases kill more people than coronary heart disease, and these negative trends are becoming more pronounced.
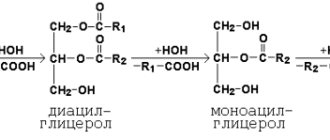
Reactions and splitting
Digestive enzymes have the narrowly focused task of breaking down complex substances that enter the gastrointestinal tract with food. These substances are broken down into simple ones that are easy for the body to absorb. In the mechanism of food processing, enzymes, or enzymes that break down fat, play a special role (there are three types). They are produced by the salivary glands and the stomach, in which enzymes break down a fairly large volume of organic substances. These substances include fats, proteins, and carbohydrates. As a result of the influence of such enzymes, the body qualitatively assimilates the incoming food. Enzymes are needed for accelerated reactions. Each type of enzyme is suitable for a specific reaction, acting on the corresponding type of bond.
Impaired digestion and absorption of carbohydrates
There are pathologies that interfere with the adequate digestion of carbohydrates in the gastrointestinal tract. Such disturbances lead to shifts in the functioning of all human organ systems. Such disorders may occur due to congenital characteristics. They can be either hereditary or acquired.
Enzymes are responsible for the high-quality digestion of food components, therefore disturbances in the functioning of lactase, a-amylase and other representatives of the enzyme group cause disturbances in physical development.
The acquisition of disturbances in the digestive process occurs in diseases of the gastrointestinal tract - colitis, gastritis, enteritis and after operations.
A congenital pathology is lactase deficiency. An insufficient amount of enzyme makes it impossible to digest dairy products. The patient experiences diarrhea, cramps, flatulence and vomiting when consuming products containing milk.
Disorders of carbohydrate metabolism and related diseases
Disorders of carbohydrate metabolism are combined into several groups.
A chronic decrease in blood sugar levels below threshold levels is called hypoglycemia. This disease is often associated with insufficient carbohydrate intake. People suffering from alcoholism are also prone to hypoglycemia.
Diabetes is usually divided into types 1 and 2. Over the past 18 years, 2.5 million patients with this diagnosis have been identified in Russia. Currently, 454 million people worldwide suffer from insulin resistance.
The disease is directly related to the adrenal hormone insulin, which plays a key role in transporting glucose molecules from the blood to the organs.
Type 1 diabetes is more common in children and is caused by viral infections. Insulin levels are never elevated and there is an absolute deficiency of the hormone. Patients require treatment with insulin: it is usually administered intravenously.
Type 2 diabetes is not so dangerous and is often caused by a person’s lifestyle. The effectiveness or production of insulin is impaired - a relative deficiency of the hormone. Occurs in 90-95% of all diabetic patients.
Thus, the causes of carbohydrate metabolism disorders can be considered both hereditary defects and malfunctions of the liver and pancreas. Causes may include tumors, poor diet and stress.
Insulin and glucagon response
In response to the digestion of carbohydrates in the gastrointestinal tract, the body launches 2 reactions. After any meal, often even one that does not contain many carbohydrates, insulin is produced by the adrenal glands. Its task is to regulate glucose concentration and blood viscosity.
First of all, saccharides are sent to the liver and skeletal muscles to replenish the depot. If the depot is full, then the energy is converted into adipose tissue. Insulin is an anabolic hormone.
Glucagon decides whether the liver needs to use its internal reserves. It is also produced by the pancreas and is a peptide hormone.
While insulin stores energy, glucagon activates the breakdown of fat reserves in the liver and the conversion of fatty acids into ketones, which also provide energy.
Glucagon acts like adrenaline: it releases glucose to allow the body to react quickly, increases the frequency and strength of the heartbeat, and also increases blood pressure.
Assimilation
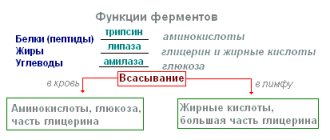
For better absorption of fats, gastric juice containing lipase works in the body. This enzyme, which breaks down fat, is produced by the pancreas. Carbohydrates are broken down by amylase. After disintegration, they are quickly absorbed and enter the bloodstream. Salivary amylase, maltase, and lactase also contribute to breakdown. Proteins are broken down thanks to proteases, which are also involved in the normalization of the microflora of the gastrointestinal tract. These include pepsin, chymosin, trypsin, erepsin and pancreatic carboxypeptidase.
Treatment of carbohydrate metabolism disorders
Depending on the type of disorder, the appropriate treatment method is used:
- Medication – drugs that reduce the concentration of glucose in the blood.
- Insulin therapy – drugs containing insulin.
- Nutrition correction – includes the development of an individual plan depending on the type of disorder and characteristics of the body; often based on reducing calories and increasing fiber. Fractional meals are used. In rare cases, on the contrary, intermittent fasting.
- Physical activity – training and exercises of varying intensity.
Modern medicine is capable of replacing enzyme deficiencies artificially. These are tablets and substances administered orally and intravenously. The disadvantage of this treatment is the cost. Diet is often used to treat enzyme deficiencies. How to improve the digestion process
Proper nutrition promotes efficient digestion and improves overall well-being.
A person can improve digestion by following the recommendations of nutritionists:
- Consumption of natural food significantly reduces the likelihood of metabolic diseases. The fact is that the modern Western diet contains a large amount of refined carbohydrates, which are quickly absorbed and increase blood glucose levels. A high concentration of saturated and trans fats has an equally detrimental effect on metabolism.
- An increase in the amount of fiber promotes the proliferation of normal microflora in the large intestine. In addition, dietary fiber cleanses the gastrointestinal tract and slows down the absorption of fatty acids and fast carbohydrates.
- Vegetable fats are an excellent source of calories , macro- and micronutrients. Fats, unlike carbohydrates, cause satiety and relieve constipation. Many hormones have a base consisting of fatty acids. Natural vegetable fats are a structural unit of hormones, enzymes and the membrane that covers nerve cells.
- Water is very important in the digestion process. Sources of fluid can include vegetables, fruits and drinks. Despite the popular belief that tea and coffee are not sources of liquid, these products are 99% liquid.
- Chewing is the first stage of digestion. Thoroughly chewed food is much easier to digest. The saliva released during chewing softens the food bolus and reduces acidity, preventing dyspepsia and heartburn.
- Movement is life. Physical activity promotes blood circulation, acceleration of metabolism, and the efficiency of the endocrine, cardiovascular and nervous systems.
Products necessary for proper digestion
Following a properly formulated diet and periodic exercise significantly improves digestion and helps speed up metabolism. Here it is important not to go to extremes: you cannot eat only carbohydrates or, conversely, radically reduce their amount in the diet.
In this case, problems with the normal functioning of the gastrointestinal tract may occur. You need to find a balance of macronutrients taking into account the characteristics of the body. Formulas for calculating KBZHU will help with this.
Author: Svitkevich Yulia Vyacheslavovna
What is the name of the main enzyme that breaks down fat in the human body?
Lipase is an enzyme whose main task is to dissolve, fractionate and digest fats in the human digestive tract. Fats entering the intestines are not able to be absorbed into the blood. To be absorbed, they must be broken down into fatty acids and glycerol. Lipase helps in this process. If there is a case where the enzyme that breaks down fat (lipase) is reduced, it is necessary to carefully examine the person for oncology.
Pancreatic lipase in the form of an inactive proenzyme of prolipase is excreted into the duodenum. Prolipase is activated under the influence of bile acids and colipase, another enzyme from pancreatic juice. Lingual lipase is produced in infants by the oral glands. It is involved in the digestion of breast milk.
Hepatic lipase is secreted into the blood, where it binds to the vascular walls of the liver. Most fats from food are broken down in the small intestine by lipase from the pancreas.
Knowing which enzyme breaks down fats and what exactly the body cannot cope with, doctors can prescribe the necessary treatment.
The chemical nature of almost all enzymes is protein. The pancreas is simultaneously an organ of the digestive and endocrine systems. The pancreas itself is actively involved in the digestion process, and the main gastric enzyme is pepsin.
Classification
Depending on their role in chemical reactions, the following classes of enzymes are distinguished:
| Classes | Peculiarities |
| Oxyreductases | Catalyze the oxidation of their substrates by transferring electrons or hydrogen atoms |
| Transferases | Participate in the transfer of chemical groups from one substance to another |
| Hydrolases | Break down large molecules into smaller ones by adding water molecules to them |
| Lyases | Catalyze the cleavage of molecular bonds without the process of hydrolysis |
| Isomerases | Activate rearrangement of atoms in a molecule |
| Ligases (synthetases) | They form bonds with carbon atoms using the energy of ATP. |
In a living organism, all enzymes are divided into intra- and extracellular. Intracellular enzymes include, for example, liver enzymes that participate in the reactions of neutralizing various substances that enter the blood. They are detected in the blood when an organ is damaged, which helps in diagnosing its diseases.
Intracellular enzymes that are markers of damage to internal organs:
- liver – alanine aminotranssephrase, aspartate aminotransferase, gamma-glutamyl transpeptidase, sorbitol dehydrogenase;
- kidneys – alkaline phosphatase;
- prostate gland – acid phosphatase;
- cardiac muscle - lactate dehydrogenase
Extracellular enzymes are secreted by glands into the external environment. The main ones are secreted by the cells of the salivary glands, gastric wall, pancreas, and intestines and are actively involved in digestion.
How do pancreatic enzymes break down fat into simple substances?
Amylase breaks down starch into oligosaccharides. The oligosaccharides are then broken down into glucose by other digestive enzymes. Glucose is absorbed into the blood. For the human body it is a source of energy.
All human organs and tissues are built from proteins. The pancreas is no exception, which activates enzymes only after they enter the lumen of the small intestine. When the normal functioning of this organ is disrupted, pancreatitis occurs. This is a fairly common disease. A disease in which there is no enzyme that breaks down fats is called pancreatic insufficiency: exocrine or intrasecretory.
Decreased enzyme activity - causes
1. Food is not chewed thoroughly, food is absorbed too quickly - there is no stimulation of the production of enzymes in other digestive organs.
2. The body does not have enough necessary nutrients (vitamins, minerals, microelements) for a certain type of enzyme to work, and as a result, the enzyme does not work.
3. Stomach acidity is reduced - the production of enzymes, which is catalyzed by hydrochloric acid, is reduced.
4. Food consumed - nuts, seeds, whole grains, etc. - contains enzyme inhibitors.
5. A person is often in a state of stress, which depletes the production of enzymes.
6. The body is susceptible to intoxication with heavy metals, because of this, enzymatic reactions fade away.
7. Genetic digestive defects (for example, there is no synthesis of lactase, which helps digest lactose coming from milk).
Deficiency problems
Exocrine insufficiency reduces the production of digestive enzymes. In this case, a person cannot eat large amounts of food, since the function of breaking down triglycerides is impaired. Such patients, after eating fatty foods, experience symptoms of nausea, heaviness, and abdominal pain.
With intrasecretory insufficiency, the hormone insulin, which helps absorb glucose, is not produced. A serious disease occurs, which is called diabetes mellitus. Another name is diabetes diabetes. This name is associated with an increase in urine production by the body, as a result of which it loses water and the person feels constant thirst. Carbohydrates almost do not enter the cells from the blood and therefore are practically not used for the body’s energy needs. The level of glucose in the blood increases sharply, and it begins to be excreted through the urine. As a result of such processes, the use of fats and proteins for energy purposes increases greatly, and products of incomplete oxidation accumulate in the body. Ultimately, the acidity in the blood also increases, which can even lead to a diabetic coma. In this case, the patient experiences respiratory distress, including loss of consciousness and death.
This example clearly shows how important enzymes are that break down fats in the human body so that all organs work harmoniously.
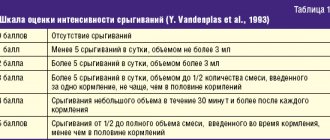
Clinic and symptoms
Clinic and symptoms
Pancreatic enzyme deficiency manifests itself in:
- abdominal discomfort (pain, swimming, bloating, gurgling, etc.);
- signs of disturbance, breakdown of nutrients (primarily fats) - steatorrhea.
Poor intestinal absorption can lead to some symptoms of nutrient deficiency, such as: blurred vision in the dark (vitamin A deficiency), bone pain, muscle twitching, cramps (electrolyte imbalance) and bruising (impaired clotting factor synthesis). blood).
Self-medication
In medicine, enzymes that break down fats in the human body can be obtained with the help of medications. There are many of them - from the most famous brands to little-known and less expensive, but just as effective. The main thing is not to self-medicate. After all, only a doctor, using the necessary diagnostic methods, can select the right drug to normalize the functioning of the gastrointestinal tract.
However, often we only help the body with enzymes. The hardest part is getting it to work correctly. Especially if the person is already elderly. It is only at first glance that it seems that you bought the necessary pills - and the problem is solved. In reality, everything is completely different. The human body is a perfect mechanism, which nevertheless ages and wears out. If a person wants it to serve him as long as possible, it is necessary to support it, diagnose and treat it on time.
Of course, after reading and finding out which enzyme breaks down fats during human digestion, you can go to the pharmacy and ask the pharmacist to recommend a drug with the desired composition. But this can only be done in exceptional cases, when for some compelling reason it is not possible to visit a doctor or invite him to your home. You need to understand that you can be very wrong and the symptoms of different diseases can be similar. And in order to make a correct diagnosis, you definitely need medical help. Self-medication can cause serious harm.
General properties of enzymes
Enzymes are protein molecules that interact with various substances, accelerating their chemical transformation along a certain path. However, they are not consumed. Each enzyme has an active site that attaches to the substrate and a catalytic site that initiates a particular chemical reaction. These substances accelerate the biochemical reactions occurring in the body without increasing the temperature.
Main properties of enzymes:
- specificity: the ability of an enzyme to act only on a specific substrate, for example, lipases on fats;
- catalytic efficiency: the ability of enzymatic proteins to accelerate biological reactions hundreds and thousands of times;
- ability to regulate: in each cell, the production and activity of enzymes is determined by a unique chain of transformations that affects the ability of these proteins to be synthesized again.
The role of enzymes in the human body cannot be overestimated. At a time when the structure of DNA had just been discovered, it was said that one gene was responsible for the synthesis of one protein, which already determined a specific trait. Now this statement sounds like this: “One gene - one enzyme - one trait.” That is, without the activity of enzymes in the cell, life cannot exist.
Digestion in the stomach
Gastric juice contains pepsin, hydrochloric acid and lipase. Pepsin acts only in an acidic environment and breaks down proteins into peptides. Lipase in gastric juice breaks down only emulsified (milk) fat. The fat-digesting enzyme becomes active only in the alkaline environment of the small intestine. It comes along with the composition of the food semi-liquid gruel, pushed out by the contracting smooth muscles of the stomach. It is pushed into the duodenum in separate portions. Some small part of the substances is absorbed in the stomach (sugar, dissolved salt, alcohol, pharmaceuticals). The digestion process itself mainly ends in the small intestine.
Food advanced into the duodenum receives bile, intestinal and pancreatic juices. Food moves from the stomach to the lower sections at different speeds. Fatty ones linger, but dairy ones pass quickly.
The use of digestive enzymes in gastroenterological practice
P
Digestive enzymes are widely used for various gastroenterological pathologies.
Enzymes are actively used for various diseases of the stomach, small and large intestines, biliary tract and pancreas. Indications for the appointment of enzyme therapy
are disorders of the secretion of endogenous enzymes, disorders of absorption of nutrients and disorders of motility of the gastrointestinal tract. Currently, the global pharmaceutical industry produces a large number of enzyme preparations (Digestal, Creon, Mezim-Forte, etc.), which differ from each other both in the dose of digestive enzymes they contain and in various additives (see table). Digestive enzymes are available in various forms: tablets, powder or capsules containing enteric-coated microgranules. All enzyme preparations differ in their composition: containing pancreatin (pancreatic extract, usually of pork origin) or digestive enzymes, plant origin, extract of the gastric mucosa. The composition of the drug, in addition to enzymes, may include components of bile, gastric mucosa or adsorbents (simethicone or dimethicone).
Choice of drug
for the treatment of a patient with gastroenterological pathology should be based on the following indicators:
• absolute and relative content of enzymes in the drug (a high content of proteases is indicated for patients with decreased gastric secretion and a painful form of chronic pancreatitis; an increase in lipase activity is necessary for replacement therapy for pancreatic insufficiency);
• the presence of a shell that protects enzymes from digestion by gastric juice;
• the size of the tablet or granules filling the capsules (evacuation of the drug from the stomach simultaneously with food occurs if the size of its particles does not exceed 2 mm);
• the presence of bile acids in the composition of the drug (bile acids improve the digestion of lipids, increase the absorption of fatty acids and cholesterol, and cause increased pancreatic secretion). However, high levels of bile acids in the intestine during intensive enzyme therapy can cause hologenic diarrhea.
Digestive enzymes are indicated for patients with gastric secretion disorders
(hypo- and anacid chronic gastritis, conditions after gastrectomy). After surgical intervention on the stomach, malabsorption syndrome may develop, which is associated with a large number of different factors: a decrease in the production of hydrochloric acid and pepsin; violation of chyme mixing and mechanical processing; disruption of the fractional flow of chyme into the small intestine; acceleration of passage through the small intestine; decreased endogenous stimulation of pancreatic secretion; asynchronous flow of pancreatic juice, bile and chyme into the small intestine [17]. Treatment of post-gastroresection disorders requires complex therapy using antacids, agents that affect gastrointestinal motility, and digestive enzymes.
In hypoacid conditions accompanied by a decrease in the availability of nutrients, preparations containing bile are indicated. These drugs help increase the production of bile and pancreatic juice; they should be taken 1-3 tablets during or immediately after meals (without chewing) 3-4 times a day in courses of up to 2 months.
Preparations containing bile should be used with caution in patients with chronic hepatitis or cirrhosis of the liver, since bile acids enter the liver via the enterohepatic route, where they are metabolized, as well as in cholestatic diseases, peptic ulcers, Crohn's disease and ulcerative colitis.
Hypoacid gastritis is an indication for the prescription of drugs containing components of the gastric mucosa: pepsin and hydrochloric acid. These components provide mechanical and chemical processing of food, primarily proteins. Proteolysis occurs to the level of polypeptides, which are then broken down by pancreatic proteases and partially to amino acids. Pepsin stimulates pancreatic secretion and is therefore contraindicated in patients with chronic pancreatitis, especially in the presence of intraductal hypertension. Preparations containing pepsin are taken at the rate of 0.2–0.5 g of pepsin per meal, 2–3 times a day before or during meals. Recently, for the treatment of patients with a decrease in the acid-forming function of the stomach, drugs containing pure pancreatin, 1 t (4 times a day at the beginning of meals), have been successfully used.
For the treatment of hypomotor dyskinesia (hypokinesia) of the biliary tract
and disorders of fat solubilization, enzyme preparations containing bile acids are successfully used. Bile acids and salts increase the contractile function of the gallbladder and normalize the biochemical properties of bile.
Treatment of pancreatitis with severe pain
requires strict restriction of diet, prescription of antisecretory agents, antispasmodics and pure pancreatin preparations in high doses.
These remedies are the most universal for normalizing digestion in the gastrointestinal tract and can be used as part of complex therapy for all types of disorders. Enzyme products containing pure pancreatin contain proteases, amylase, and lipase. The drug Digestal
contains hemocellulase, which ensures the breakdown of cellulose. Modern research shows that digestive pancreatic enzymes in the traditional non-enteric form provide pain relief during exacerbation [20]. The entry of pancreatic enzymes (primarily trypsin) into the duodenum destroys the releasing peptides of secretin and cholecystokinin and causes a decrease in pancreatic secretion, ensuring functional rest of the organ (Fig. 1).
Rice. 1. Regulation of pancreatic secretion using releasing peptides (according to Li Y., Owyang C., 1996)
Much hope has been associated with digestive enzymes of plant and fungal origin, primarily due to the high acid resistance of plant and fungal lipases. However, under experimental conditions, bacterial lipase turned out to be 75 times less active than pork lipase, and therefore these drugs have not yet found use in clinical practice. Pancreatin does not affect gastrointestinal motility, bile secretion, or bile duct function.
Replacement therapy for exocrine pancreatic insufficiency
necessary for various diseases when atrophy of more than 90% of the organ parenchyma occurs [19] (Fig. 2), occurring most often in the late stage of chronic pancreatitis. Indications include steatorrhea (fat loss in feces more than 15 g/day, with a normal rate of up to 7 g/day), progressive weight loss, diarrhea, and dyspeptic symptoms. Treatment of exocrine pancreatic insufficiency still remains a challenge. Currently, therapy in several areas can be considered the most established: avoiding alcohol consumption, following a diet with frequent small amounts of food, enzyme replacement therapy, combating vitamin deficiency, analgesics (paracetamol, tramadol), psychotropic drugs.
Rice. 2. Etiology of exocrine pancreatic insufficiency
Enzyme therapy for the development of exocrine pancreatic insufficiency requires the use of capsules containing microgranules (microtablets) of pancreatin. In case of disturbances in the hydrolysis of nutrients, capsules are significantly more effective than regular-sized pancreatin tablets. The peculiarity of these drugs is that the enzymes they contain are released only in the alkaline environment of the small intestine and thus avoid destruction by gastric juice (Fig. 3), which significantly increases the effectiveness of replacement therapy for pancreatic steatorrhea. The stability of the drug in an acidic environment is a very important property of the drugs (the main components of enzyme preparations - lipase and trypsin quickly lose activity in an acidic environment: lipase at pH = 4, trypsin at pH = 3; before the drug enters the duodenum, up to 92% of the lipase can be destroyed ). This property significantly increases the effectiveness of replacement therapy and reduces or eliminates the need to prescribe drugs that block gastric secretion. Thus, when using a drug that has an enteric coating, fat absorption is on average 20% higher than when using a conventional drug in the same dose. However, in patients with chronic pancreatitis, the production of bicarbonates is significantly reduced, which leads to impaired alkalization in the duodenum and impaired activation of accepted enzymes. In this case, the effectiveness of the encapsulated enzymes may be significantly reduced.
Rice. 3. Effect of a microtablet drug with an enteric coating
The downside of enteric-coated drugs is that the enzymes do not have time to activate in the duodenum, the main site of production of pancreatic regulatory peptides. The low activity of proteases in the duodenum does not allow interrupting the stimulation of pancreatic secretion through a negative feedback mechanism and does not reduce the pressure in the ducts and parenchyma of the pancreas. High intrapancreatic pressure is considered the main mechanism for the development of intense pain in chronic pancreatitis, and therefore encapsulated enzymes are recommended only as replacement therapy, and for pain relief (especially with intraductal hypertension) - traditional pancreatin tablets or powder.
However, according to our own data, treatment of chronic pancreatitis using encapsulated pancreatin
led to a significant decrease in the intensity of abdominal pain in the examined patients (p=0.0063; Fig. 4). Moreover, the degree of pain reduction significantly depended on the degree of decrease in fecal elastase activity compared to the initial level (p = 0.0219). Thus, the analgesic effect of the therapy directly depended on the degree of suppression of the exocrine function of the pancreas in the patient. The exocrine function of the pancreas according to the elastase test (determination of fecal elastase using an immunoreactive method) significantly decreased compared to the background: 279.46±27.41 μg/g and 254.87±26.74 μg/g (n=52, p= 0.0152).
Rice.
4. Intensity of pain before treatment and while taking KPMES. The particle size of microgranulated preparations should not exceed 2 mm
, which ensures simultaneous evacuation of food and enzymes from the stomach. Further reduction in granule size does not lead to an increase in the efficiency of food digestion [13]. The administration of pancreatin capsules in a dose of 16–18 thousand units per meal to patients with chronic pancreatitis after surgical interventions on the pancreas (pancreaticoduodenectomy and drainage of the Wirsung's duct) for 2.5 years made it possible to reduce the loss of fat in feces from 33.6 g/day to 15.3 g/day [7]. There was a statistically significant increase in the body weight of patients and biochemical indicators of trophological status (serum iron, total iron-binding capacity of blood serum, total number of lymphocytes).
According to information obtained by Farkas G., Takacs T. et al. (1999), prescribing microgranulated pancreatin to patients after surgery on the pancreas at a dose of 25 thousand units. 3 times a day for 10 days did not lead to changes in pancreatic function compared to placebo [12]. Nevertheless, the therapy made it possible to effectively eliminate the symptoms of maldigestion, stabilize body weight (in the comparison group - weight loss of 3.5 kg over the same time) and increase the breakdown of carbohydrates by 35%.
Adequate therapy of exocrine pancreatic insufficiency syndrome requires the use of high doses of enzyme preparations. It is usually necessary to use enzymes in encapsulated form. The drug dosage regimen is as follows: 1–4 capsules of the enzyme preparation with main meals (at the beginning of a meal) and 1 capsule (tablet) with a small amount of food. The patient should avoid eating foods rich in fiber, as they reduce enzyme activity as in vitro
, and
in vivo
. The main component of the enzyme preparation, which determines the effectiveness of the treatment of digestive disorders, is lipase. At the same time, proteases and, above all, trypsin are the main inhibitors of lipase. Therefore, to relieve steatorrhea, one should not strive to significantly increase the proteolytic activity of chyme. Often, a high dose of enzymes entering the stomach does not provide the desired result: the main components of enzyme preparations, lipase and trypsin, quickly lose activity in an acidic environment. Therefore, the effectiveness of enzyme therapy can be increased by the simultaneous administration of antacid or antisecretory drugs, but it must be remembered that antacids containing calcium or magnesium weaken the effect of enzyme drugs.
Many open questions remain in assessing the effectiveness of enzyme replacement therapy, in particular, replacement therapy, and determining optimal doses. Thus, there are two groups of patients: patients in whom pancreatic secretion exceeds 10%, but nevertheless have steatorrhea; and those in which lipase secretion is practically absent, but normal digestion and absorption of fat is maintained. This may be due, respectively, to the different reserve secretory capacity of the pancreas and to the action of non-pancreatic lipases (produced by the mucous membrane of the tongue and stomach, mainly the upper part of the greater curvature). Researchers estimate that patients with exocrine pancreatic insufficiency may absorb more than 50% of dietary fat in the absence of detectable pancreatic lipase activity. It has been shown that in patients with severe pancreatitis with steatorrhea, when taking 100 g of fat with food, 20–50 g of fat can be absorbed without enzyme replacement therapy. According to Abrams CK, Hamosh M. et al. (1987) [5], in patients with pancreatic exocrine insufficiency, non-pancreatic lipases provide more than 90% of the total lipolytic activity at the level of the duodenojejunal junction, whereas in healthy people - 7%. This observation may, at least in part, explain why some patients do not require enzyme replacement therapy after total pancreatectomy.
However, in a double-blind crossover study, Neoptolemos JP, Ghaneh P. et al. (1999) in 37 patients with CP with exocrine insufficiency after extensive resection of the pancreas, there were no significant differences in stool frequency, fecal volume and daily loss of fat in feces while taking a standard or high dose of pancreatin. In this regard, the authors conclude that the main advantage of modern drugs with a high content of pancreatin in one capsule is convenience for the patient, which ensures more accurate adherence to the treatment regimen. In another study, when prescribing a capsulated drug to patients with chronic pancreatitis, no dependence of fecal fat content on the dose of the drug was found [15], which suggests the presence of a certain threshold of enzyme efficiency, upon reaching which a further increase in dose does not lead to a decrease in steatorrhea.
Treatment of patients with disorders of motor function and colon tone
, for example, with irritable bowel syndrome, in addition to antispasmodics, enveloping, psychotropic drugs, sometimes requires the use of digestive enzymes. The use of enzymes, which contain bile components, causes increased intestinal motility and helps resolve constipation in patients. Enzyme preparations that contain hemicellulase (Digestal) improve the digestion of plant foods and reduce bloating, which gives a good symptomatic effect.
Healthy individuals can take digestive enzymes to relieve dyspeptic symptoms after overeating
. Occasional intake of small doses of digestive enzymes (1-2 tablets) does not affect pancreatic function and is considered safe. In this situation, drugs with bile components have proven themselves to be the best.
The reasons for the ineffectiveness of replacement therapy may be associated with both inaccurate diagnosis of the disease and inadequate therapy. Sometimes a lower dose of the drug is prescribed to reduce the cost of treatment. Patients may incorrectly follow the prescribed treatment regimen: reduce the frequency of doses or take the enzyme at the wrong time (before or after meals). Enzyme preparations are ineffective for steatorrhea of extrapancreatic origin (celiac disease, giardiasis, etc.). The action of enzymes is impaired in intestinal motility disorders. Incorrect treatment regimen: prescription of enzymes that do not have an acid-protective shell without inhibitors of gastric secretion; the use of drugs that, due to the large size of the granules, do not enter the duodenum simultaneously with food.
Side effects of enzyme therapy are usually not severe. The most dangerous of them, the development of fibrosing colopathy, occurs in children with cystic fibrosis with long-term intake of very high doses of encapsulated enzymes - more than 50 thousand units of lipolytic activity per 1 kg of body weight per day. In addition, patients may experience pain in the oral cavity (usually when taking enzymes in powder form), skin irritation in the perianal area, and a feeling of discomfort in the abdomen. Long-term enzyme therapy in high doses can cause hyperuricemia, in some cases allergic reactions to pork protein occur (including in relatives of patients with exocrine pancreatic insufficiency and medical personnel). The formation of complexes with enzymes sometimes leads to impaired absorption of folic acid.
The list of references can be found on the website https://www.rmj.ru
Enzyme preparation –
Digestal (trade name)
(ICN Pharmaceuticals)
Literature:
1. Geller L. I., Pashko M. M., Obukhova G. G. Exocrine and endocrine pancreatic disorders in chronic pancreatitis. // Sov. Honey. – 1989. – No. 8. – pp. 4–7.
2. Yakovenko E.P. Enzyme preparations in clinical practice // Klin. pharm. and ter., 1998, No. 1, p. 17–20.
3. A primer of pancreatitis PGLankisch, M.Buchler, J.Mossner, S.Muller–Lissner // Springer, 1997.
4. Abrams CK, Hamosh M., Lee TC, Ansher AF, Collen MJ, Lewis JH, Benjamin SB, Hamosh P. Gastric lipase: localization in the human stomach. // Gastroenterol. – 1988. – Vol. 95. – P. 1460–1464.
5. Abrams CK, Hamosh M, Dutta SK, Hubbard VS, Hamosh P. Role of nonpancreatic lipolytic activity in exocrine pancreatic insufficiency. // Gastroenterol. – 1987. –Vol. 92. – P. 125–129.
6. Banks PA Acute and chronic pancreatitis. In: Sleisenger and Fordtran's gastrointestinal and liver disease: pathophysiology/diagnosis/management / Mark Feldman, Bruce F. Scharschmidt, Marvin H. Sleisenger–6th ed. WBSaunders company, 1998.
7. Braga M., Cristallo M., De Franchis R., Mangiagalli A., Agape D., Primignani M., Di Carlo V. Correction of malnutrition and maldigestion with enzyme supplementation in patients with surgical suppression of exocrine pancreatic function. // Surg. Gynecol. Obstet. – 1988. – Vol. 167, Dec. – No. 6. – P. 485–492.
8. Creutzfeldt W., Kern E., Kummerle F., Schumacher J. Die radikale Entfernung der Bauch–speicheldruse beim Menschen – Indikationen, Ergebnisse, Folgeerscheinungen. // In: Heilmeyer L, Schoen R, de Rudder B (eds) Ergebnisse der Inneren Medizin. – Springer, Berlin-Gottin-gen-Heidelberg. – 1961. – Vol. 16. – P. 79–124.
9. DiMagno EP Future aspects of enzyme replacement therapy. In Lankisch (Ed.) Pancreatic enzymes in health and disease, pp. 209–214, Springer–Verlag, Berlin, Heidelberg, 1991.
10. DiMagno EP Patterns of human exocrine pancreatic secretion and fate of human pancreatic enzymes during aboral transit. In Lankisch (Ed.) Pacreatic enzymes in health and disease, pp. 1–10, Springer–Verlag, Berlin, Heidelberg, 1991.
11. Diseases of the gut and pancreas. JJMisiewicz, REPounder, CWVenables eds., Blackwell scientific publication, 1994, vol. 1.
12. Farkas G., Takacs T., Baradnay G., Szasz Z. Effect of pancreatin replacement on pancreatic function in the postoperative period after pancreatic surgery. // Orv. Hetil. – 1999. – Dec 5. – vol. 140. – No. 49. – P. 2751–2754.
13. Halm U., Loser C., Lohr M., Katschinski M., Mossner J. A double-blind, randomized, multicentre, crossover study to prove equivalence of pancreatin minimicrospheres versus microspheres in exocrine pancreatic insufficiency. // Aliment. Pharmacol. Ther. – 1999 – Vol. 13. – No. 7. – P. 951–957.
14. Lankisch PG, Banks PA Pancreatitis. Springer-Verlag: Berlin, Heidelberg. – 1998. – P. 377.
15. Opekun AR Jr, Sutton FM Jr, Graham DY Lack of dose–response with Pancrease MT for the treatment of exocrine pancreatic insufficiency in adults. // Aliment. Pharmacol. Ther. – 1997, Oct. – Vol. 11. – No. 5. – P. 981–986.
16. Paris JC A Multicentre Double–Blind Placebo–Controlled Study of the Effect of a Pancreatic Enzyme Formulation (Panzytrat(r) 25,000) on Impaired Lipid In Adults with Chronic Pancreatitis //Drug Invest. 5(4):229–237, 1993.
17. Riley SA, Marsh MN Maldigestion and malabsorption. In: Sleisenger and Fordtran's gastrointestinal and liver disease: pathophysiology/diagnosis/management / Mark Feldman, Bruce F. Scharschmidt, Marvin H. Sleisenger–6th ed. WBSaunders company, 1998.
18. Roberts IM Enzyme therapy for malabsorption in exocrine pancreatic insufficiency. Pancreas 1989, #4, 496–503.
19. Sarles H., Pastor J., Pauli AM, Barthelemy M. Determination of pancreatic function. A statistical analysis conducted in normal subjects and in patients with proven chronic pancreatitis (duodenal intubation, glucose tolerance test, determination of fat content in the stools, sweat test). //.Gastroenterol. – 1963. – Vol. 99. – P. 279–300.
20. Stead RJ, Skypala I., Hodson ME Treatment of steatorrhoea in cystic fibrosis: a comparison of enteric–coated microspheres of pancreatin versus non–enteric–coated pancreatin and adjuvant cimetidine. // Aliment. Pharmacol. Ther. – 1988, Dec. – Vol. 2. – No. 6. – P. 471–482.
Lipase
Pancreatic juice is an alkaline liquid that is colorless and contains trypsin and other enzymes that break down peptides into amino acids. Amylase, lactase and maltase convert carbohydrates into glucose, fructose and lactose. Lipase is an enzyme that breaks down fats into fatty acids and glycerol. Digestion time and juice release depend on the type and quality of food.
The small intestine performs parietal and cavity digestion. After mechanical and enzymatic treatment, the breakdown products are absorbed into the blood and lymph. This is a complex physiological process that is carried out by the villi of the small intestine and the villi from the intestine are directed strictly in one direction.
Brief information about carbohydrates (types, meaning and functions of carbohydrates. What are they for)
Based on their structure, carbohydrates are divided into 3 groups.
- Monosaccharides are the simplest organic compounds. These include: glucose, fructose, deoxyribose and ribose, as well as aldoses and ketoses.
- Oligosaccharides include from 2 to 10 monosaccharide residues. The most famous are disaccharides - a subgroup of oligosaccharides consisting of two monosaccharides. These include lactose, sucrose and maltose. These are dense, sweet, crystalline substances.
- Polysaccharides consist of the largest number of monosaccharides. Unlike oligosaccharides and monosaccharides, many polymers do not dissolve in water and perform reserve, structural functions in the body. Examples of polysaccharides: starch, glycogen, inulin, chitin, pectins, cellulose and arabinoxylans.
The most common carbohydrates in food are glucose, fructose, lactose, starch and cellulose (fiber):
| Name of carbohydrate | Source and functions |
| Glucose | The smallest and most common saccharide molecule, the structure is a monosaccharide. It instantly enters the bloodstream and provokes a surge in insulin, which is dangerous for people with diabetes. |
| Fructose | A carbohydrate obtained from fruits and vegetables. It has its own specifics, since it does not cause a sharp jump in glucose in the blood and is able to be deposited in the form of liver glycogen and adipose tissue of internal organs. |
| Lactose | Contained in the milk of mammals and in products made from it. Milk sugar is one of the first components that enters the child’s body. He is responsible for the growth and development of the baby. People who are lactose intolerant lack the enzyme that helps digest and absorb milk. |
| Starch | Can be found in potatoes, corn, rice and flour. This carbohydrate has the ability to swell in hot water, but does not dissolve in cold water. Tasteless, has the consistency of white powder. Starch performs reserve and structural functions in the human body. |
| Cellulose | Component of plant cell membranes. It has neither taste nor smell, but has a positive effect on the functioning of the digestive system. It is used in pharmaceuticals as a tablet filler. Healthy lifestyle enthusiasts try to increase the fiber content of their diet by eating more green vegetables, whole grains and unsweetened fruits. |
Cellulose has a “double” - tunicin, discovered in 1845. Carl Ernest Schmidt in the simplest tunicates. New research has shown that it is also found in the bodies of slugs, mollusks and arthropods.
First of all, carbohydrates perform an energy function. A person, like any other creature, needs energy for full life. Energy is constantly consumed - during work, mental activity and even during sleep.
Saccharides are part of the structure of cell membranes and complex molecules of ribose and deoxyribose, which are involved in the construction of DNA.
Suction
Amino acids, vitamins, glucose, and mineral salts in the aqueous solution are absorbed into the capillary blood of the villi. Glycerol and fatty acids do not dissolve and cannot be absorbed by the villi. They move into epithelial cells, where fat molecules are formed that enter the lymph. Having passed the barrier of the lymph nodes, they enter the blood.
Bile plays a very important role in the absorption of fats. Fatty acids, combining with bile and alkalis, are saponified. In this way, soaps (soluble salts of fatty acids) are formed that easily pass through the walls of the villi. The glands in the large intestine primarily secrete mucus. The large intestine absorbs water up to 4 liters per day. A very large number of bacteria live here, participating in the breakdown of fiber and the synthesis of vitamins B and K.
Coenzymes and substrates.
Many large molecular weight enzymes exhibit catalytic activity only in the presence of specific low molecular weight substances called coenzymes (or cofactors). Most vitamins and many minerals play the role of coenzymes; that is why they must enter the body with food. Vitamins PP (nicotinic acid, or niacin) and riboflavin, for example, are part of the coenzymes necessary for the functioning of dehydrogenases. Zinc is a coenzyme of carbonic anhydrase, an enzyme that catalyzes the release of carbon dioxide from the blood, which is removed from the body along with exhaled air. Iron and copper serve as components of the respiratory enzyme cytochrome oxidase.
The substance that undergoes transformation in the presence of an enzyme is called a substrate. The substrate attaches to an enzyme, which accelerates the breaking of some chemical bonds in its molecule and the creation of others; the resulting product is detached from the enzyme. This process is represented as follows:
The product can also be considered a substrate, since all enzymatic reactions are reversible to one degree or another. True, the equilibrium is usually shifted towards the formation of the product, and the reverse reaction can be difficult to detect.