Doctors call curettage curettage, and patients in gynecological departments call it cleansing. Some doctors believe that such manipulations for diagnostic purposes have no right to exist. Others easily prescribe and perform such mini-operations. There are cases when one woman undergoes 12 diagnostic cleanses in a year, causing irreparable harm to her health.
Goals and objectives of rehabilitation
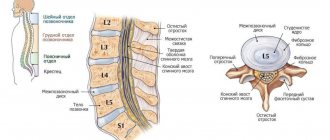
Severe back pain occurs when a hernia occurs when the cartilage disc connecting the vertebrae is destroyed. A nucleus emerges from it, which compresses the nerves going from the brain to different parts of the body. Because of the pain, a person cannot raise his arm, bend over, or turn his neck. Sometimes it is so strong that conventional hernia treatment does not help and surgery is needed.
There are 2 types of surgery to remove a herniated disc:
- Open surgery (discectomy, laminectomy)
- the surgeon removes osteophytes, body parts, vertebral arches and other formations that caused pinching. To reduce pressure on nerve fibers, it strengthens adjacent vertebrae with special inserts. Open operations are complex and are used only in extreme cases. Recovery takes several months. - Minimally invasive interventions
- the doctor eliminates the hernia through a small incision using endoscopic equipment or nucleoplasty. The patient recovers after a few days.
After discectomy, pain caused by pinching of the spinal cord and its roots disappears quickly. The causes that caused problems with movement and bending are also eliminated.
But surgery is not the final stage of hernia treatment. Ahead of the patient lies rehabilitation, the goal of which is to speed up healing and restore the functions of the spine.
The doctor develops actions, the sequential implementation of which helps to solve the following problems:
- prevent relapses;
- reduce the risk of complications that appear after operations (thrombosis, keloid scars);
- restore normal muscle function;
- eliminate problems associated with gait and posture;
- develop the habit of correctly distributing the load on your back.
What conclusions can be drawn?
Of course, it is impossible to recommend embolization to all women suffering from fibroids without exception. However, it is important to understand the fact that if there is an opportunity to reduce all risks, you should take it!
Removal without pain, long-term rehabilitation, or fear for one’s health is what many women dream about. Some of them plan to conceive and bear a healthy child in the future. The embolization technique allows you to achieve all your goals and reduce risks. Removal is as safe as possible and has a minimum number of contraindications. Myoma disappears quite quickly. Thanks to this, the patient does not suffer from various symptoms of the disease.
Have you decided to intervene?
Do you want fibroid therapy to be carried out by an experienced doctor?
Contact the endovascular surgery center prof. Kapranova! Here, only a progressive technique is used to remove fibroids.
You yourself will be able to choose a clinic for the intervention and determine the time of the procedure.
Call Sergei Anatolyevich on his personal numbers:
- +7,
- +7.
Discuss all conditions and features of the intervention. Talk about possible risks and complications. This will allow you to make the right decision.
What happens if you don't undergo rehabilitation?
If you ignore the rehabilitation period, the tissues will not heal properly, which will reduce the effectiveness of the hernia surgery. Muscles and ligaments will remain undeveloped, which will have a bad effect on flexibility and the ability to withstand stress. The result is a recurrence of the vertebral hernia, the return of discomfort.
Each type of intervertebral hernia has serious complications, so you should not delay treatment.
See how easy it is to get rid of a hernia in 10 sessions
Stages of rehabilitation
Conventionally, rehabilitation is divided into 3 stages.
Follow your doctor's instructions at every stage! Do all actions step by step, do not jump to more difficult movements or exercises ahead of time.
Stage 1 – initial
The early, initial stage lasts the first 15 days. After surgery to remove a spinal hernia, rehabilitation involves taking antibiotics, NSAIDs (non-steroidal anti-inflammatory drugs), sedatives, and sedatives, as the patient feels discomfort in the back. It subsides within a week. Antiseptic treatment of sutures is carried out regularly to prevent inflammation.
Drug treatment is aimed at:
- tumor reduction;
- reduction of pain syndrome;
- acceleration of tissue healing;
- reducing the risk of infection of the operated area;
- maintaining muscle tone;
- reducing the risk of thrombosis.
What not to do
You can walk at the early stage of rehabilitation only after the doctor’s permission, 5-10 minutes
Immediately after the operation, the body is weak, any sudden movement can provoke suture separation and complications. Therefore, many actions are prohibited at an early stage, including:
- Sit for 3-6 weeks after surgery (the duration of the ban depends on the complexity of the case).
- Walk around the ward on the 1st day after surgery. The doctor usually allows you to move for 2-3 days. However, you cannot walk for a long time at this stage.
- Deep bends – If you have to bend down to pick up something that has fallen, have someone hand it to you.
- Sharp, twisting movements in the spine, bending.
- Any sports.
- Massage.
- Travel by transport, car – 14 days after surgery, even better – 2-3 months.
- Lifting weights – more than 2 kg.
If there are no complications, after the sutures are removed (7-10 days), the patient is discharged from the hospital and given a list of recommendations indicating what can and cannot be done for a year after removal of the hernia. Additionally, the next visit to a rehabilitation specialist is agreed upon.
Stage 2 – recovery
Readaptation (recovery stage) lasts 3-8 weeks. During the second period of rehabilitation after surgery to remove a hernia, the patient is already at home, taking medications if necessary. The main actions are aimed at accelerating healing and developing the back muscles. To achieve these effects, the following is prescribed:
- Physiotherapy.
- Walking 30 minutes a day.
- Exercise therapy in the gym under the supervision of a doctor. Exercise equipment is prohibited.
- Swimming on your stomach.
During movements and physical exercises, the patient should continue to use a corset or collar, which will take the load off the sore back.
At 4-6 weeks after removal of the hernia, the doctor allows you to “sit.” This also needs to be done “correctly”: at first you can only sit on the edge of the chair, trying not to overload the tailbone. The knees should be lower than the pelvis. You need to rise by holding onto the armrests of the chair.
What not to do
Sports, cycling, sudden movements, massage, bathhouse, sauna remain prohibited. However, you need to do exercise therapy and walk for at least 20 minutes. per day with breaks. You cannot stand or sit for more than 20 minutes. Periodically unload the spine, rest lying down for 20-30 minutes.
Stage 3 – late
At stage 3 of rehabilitation after removal of a hernia, you can do more active exercise therapy
From the 9th week after surgery to remove a herniated disc, the late stage begins - intensive physical rehabilitation. It provides:
- more active physical therapy exercises;
- swimming;
- classes on special simulators;
- physiotherapy;
- mud therapy;
- balneotherapy;
- massage, other gentle manual therapy techniques (after 6 months).
What not to do
In the late period of rehabilitation, a person does not feel pain, but one must remember the limitations. Remain prohibited:
- Active sports, sudden movements (swimming allowed).
- Sharp tilts and turns.
- Heavy physical work, lifting weights more than 3 kg.
- Hypothermia - always dress well, if it is very cold, wear a warm belt. If you work as a seller on the street, it is better to find something else to do.
- Bath, sauna.
Jumping and long car rides are prohibited. You cannot sit or stand for a long time (for example, in the office). Get up and move around periodically. If it's cold outside or raining, wear a warming belt. You cannot wear a corset for a long time, so as not to atrophy the long back muscles.
OUTPATIENT TRAINING
Outpatient training consists of general and ophthalmic training. In patients with hypertension, elevated blood pressure should be normalized if possible.
.
Patients with chronic bronchitis and bronchial asthma must be prescribed appropriate treatment to eliminate coughing and asthma attacks, as this can complicate the operation and lead to complications in the postoperative period
.
It is also important to establish blood sugar control in patients with diabetes. If it is impossible to carry out these measures on your own, it is better to consult with a general practitioner and endocrinologist at the clinic. It is very important to achieve regular activity of the gastrointestinal tract
(no constipation), as well as to sanitize foci of inflammation that can cause an eye infection in the postoperative period (sanitation of the oral cavity, relieving inflammation of the paranasal sinuses, nose and eyes, washing the lacrimal ducts). For chronic kidney diseases, it is necessary to obtain permission from a urologist about the possibility of eye surgery.
Meals on these days should be fractional
, 3-4 times a day, in small portions. The main rule is not to overload the stomach, especially at night, and also avoid spicy, salty and spicy foods that stimulate the appetite.
Before surgery, it is important to identify the patient's drug allergies.
Terms of rehabilitation
A rehabilitation program is drawn up immediately after the completion of surgery. Patients should take their first steps within 1-2 days. The rehabilitation period is from 4 months. It depends on:
- Type of operation. After a minimally invasive intervention, rehabilitation will take a month, while after a discectomy it will take at least six months.
- Patient's age. Rehabilitation for older people takes longer.
- Health. Rehabilitation will be delayed if there is a history of chronic diseases (diabetes mellitus).
- Weights. Obese people take longer to recover.
- The nature of the vertebral hernia. This is its size, how long ago the disease was, what difficulties it caused.
Operation methods
In the classic case, laparotomy involves the doctor making a vertical incision in the abdominal wall, bypassing, above or below the navel. The length of the incision line depends on the indication for the procedure.
Main types.
- Median laparotomy. It is used more often in gastroenterology. The surgeon gains access to the organs by making a cut with a scalpel in the center of the abdomen from the bottom of the chest to the womb.
- Pararectal laparotomy. It is carried out primarily for the treatment of gynecological pathologies. The specialist begins the operation with a dissection along the outer zone of the rectus abdominal muscle.
Techniques for directing cutting lines:
- transverse;
- longitudinal;
- corner;
- oblique;
- combined.
In gynecology, transverse and longitudinal techniques are used.
There is also exploratory laparotomy, which is used in surgery to open the abdominal cavity in order to diagnose the characteristics of the development of an oncological tumor.
What does rehabilitation include?
High-quality rehabilitation is a set of measures, each of which is aimed at improving the patient’s health. They are selected individually. To achieve the desired effect, all actions must be carried out under the strict supervision of a physician. The doctor's recommendations must be followed strictly.
Drug therapy
To relieve pain and swelling after surgery in the cervical, lumbar, and thoracic regions, the doctor prescribes:
- Analgesics
(Analgin, Lidocaine, Ketotifen) - relieve pain or reduce its manifestations. - Antibiotics
(Penicillin, Cefazolin, Vancomycin) are needed to prevent post-surgical infections. - NSAIDs
(Diclofenac, Diclak, Ketorol) - non-steroidal anti-inflammatory drugs prevent and relieve inflammation, swelling, pain. - Muscle relaxants
(Baclofen, Tolperisone, Tizanidine) - relax stiff muscles. - Chondroprotectors
(Teraflex, Artra) – strengthen bones and cartilage. - Vitamin-mineral complexes
– trigger metabolic processes, which promotes tissue healing.
Drugs prescribed during the rehabilitation period after hernia surgery
The course of drug therapy is selected by the doctor. You cannot independently reduce or increase the dosage, or shorten the course of rehabilitation after removal of a hernia. As healing progresses, the need for antibiotics, NSAIDs, and analgesics disappears. On the 10th day after removal of the hernia, antibiotics are discontinued if there are no bacterial complications.
Analgesics and NSAIDs are taken until the pain disappears. Chondoprotectors and vitamin complexes that strengthen bones and joints can be used in courses for the rest of your life.
Exercise therapy and gymnastics
The goal of exercise therapy is to restore lost functions of the spine. Exercises strengthen the back muscles, make the ligaments more flexible, without injuring or overloading them. They improve blood flow, and with it the supply of nutrients to the damaged disc, which accelerates tissue regeneration.
To achieve the desired effect, a set of exercises must be selected by the doctor taking into account the age, health, weight, and physical capabilities of the patient. Any attempts to independently adjust exercise therapy, without consultation with a rehabilitation specialist, can provoke an exacerbation of the hernia.
When performing exercises, remember these rules:
- Do not increase the load suddenly.
- Always wear a brace or collar during training.
- If an exercise causes pain, stop immediately or reduce the load. You are not ready for it yet. Contact your doctor for exercise correction.
- Do not do exercises that are prohibited at this stage of rehabilitation after surgery for a herniated disc.
- Avoid active, sudden actions. Swinging legs, jumping, strong bending, twisting exercises, and pull-ups on the horizontal bar are prohibited. Also, you should not make sharp turns of the body to the right or left.
- At the initial stage, the use of barbells, dumbbells, and any power loads is prohibited. If the doctor has approved push-ups, the exercise should first be done from the wall, and only then gradually move on to the classic version.
- Walk every day, preferably in a park or forest. Duration of walks is 30-60 minutes, rest periodically.
Best exercises
Immediately after surgery to remove a herniated disc, the doctor prescribes a gentle complex of exercise therapy. Exercises are done from a supine position:
- Rotation of hands and feet in a circle.
- Move your feet down/up.
- Bend your legs at the knee, bend your arms at the elbow.
- Pulling the right, then the left leg towards the stomach.
Over time, the complex becomes more complicated. The doctor gives more complex stretching exercises to strengthen muscle tissue. Depending on the situation, each action must be done from 4 to 10 (no more) times:
- Lying on your left side, lift your left leg straight. Bend your left elbow and place your hand behind your head. Then change the side.
- Lying on your back, lift your pelvis off the surface.
- Lying on your back, tuck your chin toward your chest.
What types of intervertebral hernias are most difficult to treat?
4 stages of treatment for intervertebral hernia
How is it carried out?
Before prescribing a cleaning procedure, the doctor reviews the results of laboratory and instrumental examinations:
- Blood analysis.
- Coagulogram (checking the rate of clotting).
- Smear for microflora and oncocytology.
- ECG.
- Ultrasound of the pelvic organs.
- Fluorography.
At the same time, the attending physician consults with an anesthesiologist and therapist. On the day of surgery you should not drink or eat. The use of vaginal products is prohibited for 24 hours. Before the procedure, the bladder is emptied. The operation is performed in a gynecological chair under general anesthesia, most often intravenous. In case of individual contraindications, local anesthesia is possible.
Separate diagnostic curettage (SDC) lasts from 10 to 15 minutes. First, the external genitalia are treated with an antiseptic composition. Then the uterine canal is expanded. Using a curette, a special tool in the form of a spoon with a long handle, a scraping is taken. These biomaterials are sent to the laboratory separately to distinguish between pathologies. During a frozen pregnancy, the contents are sucked out using a vacuum aspirator. The operation ends with repeated treatment of the vagina with an antiseptic, and ice is placed on the abdominal area for 15 minutes.
In case of prolonged reddish or brown discharge, if there is no pregnancy, the bleeding is stopped with medication. You will learn about this possibility from your attending physician. When re-evaluating the condition after the next menstruation, it often turns out that cleaning would be unnecessary. Curettage for endometrial hyperplasia or polyposis may not be necessary if a drug that can solve this problem is prescribed already in this cycle. When, a month later, the diagnosis is confirmed, cleaning with a hysteroscope is inevitable.
Physiotherapy
Physiotherapeutic procedures are prescribed when the main stage of rehabilitation is completed. Their action is aimed at improving blood circulation and lymph flow in the sore back. This helps relieve swelling, inflammation, and improves the supply of nutrients to the diseased area. The result is rapid tissue healing, restoration of muscles and nerve fibers.
In most cases, the doctor prescribes several procedures that improve the effect of each other. This:
- Electromyostimulation
is electrical stimulation of nerves and muscles aimed at improving their functioning. - Iontophoresis
- a current of low strength and voltage is supplied through electrodes. Its action is aimed at improving the condition of smooth muscles and blood vessels. Also, using the procedure, you can deliver medications to the deeper layers of the skin. - Magnetotherapy
is the effect on the body using magnetic fields, which helps improve nervous, immune, and metabolic processes. - UHF
is the effect of a high-frequency magnetic field on the body, which increases the permeability of blood vessels. Penetration of nutrients and immune cells to the diseased area improves. This stimulates tissue growth, development and healing after the hernia is removed. - Laser therapy
is the effect of a beam of concentrated light on the diseased area, which helps to warm up the soft tissues, improve blood flow, and heal the diseased area. - Diadynamic therapy
is treatment with current of different frequencies, which has an analgesic effect, improves metabolism, nerve and muscle function.
Each physiotherapy course consists of 10-15 sessions. Treatment can be continued after a short break if there are medical indications.
Manual therapy, massage
Manual therapy methods, primarily massage, will improve the condition of muscles and nervous tissue. With their help you can:
- quickly restore range of motion;
- stimulate tissue regeneration;
- remove neurological symptoms, which often persist after surgery.
Massage is prescribed no earlier than the third stage of rehabilitation after spinal hernia surgery, otherwise recently healed tissue can be damaged. A good effect is achieved by combining manual therapy with other physiotherapeutic procedures. The massage must be performed by a qualified specialist, which is confirmed by a medical diploma, reviews, and client comments.
Corset and neck collar
Corset and cervical collar are fixing accessories that need to be worn after surgery to remove lumbar and cervical hernia
If there has been surgery for a lumbar disc herniation, rehabilitation involves wearing a semi-rigid corset. If the hernia was in the upper back, you need a Shants collar.
The purpose of fixing accessories:
- correctly distribute the load, reducing pressure on the cervical, thoracic or lumbar spine;
- protect your back from overload;
- prevent sudden movements;
- reduce pain;
- recover faster after surgery.
The corset and/or collar is worn when performing exercise therapy or doing housework. According to reviews, they are very helpful when walking and at work. When the doctor allows you to drive in a car, you also cannot do without a corset.
The corset is put on and removed while lying on your back. You must wear it for at least 2 months. after surgery from 3 to 6 hours a day, and remove only at night and before daytime rest. If your doctor allows you to go to work, check with him how many hours you need to be in a corset. You cannot wear it all the time, because the back muscles will weaken too much, which will have a bad effect on the functioning of the musculoskeletal system.
Diet
During the rehabilitation period, pay special attention to diet. The body extracts nutrients from foods that are used to build cells. Therefore, food should be healthy and easily digestible.
Meat broth, cartilage, jellied meat are a natural analogue of chondoprotectors that strengthen the tissues of the intervertebral disc and prevent recurrence of the hernia. Also, products must contain fiber, vitamins A, B, C, D, phosphorus, manganese, potassium, calcium. That is why include products containing them in your menu:
- lean meat;
- offal - kidneys, heart, liver, brains;
- eggs;
- nuts;
- legumes;
- vegetables fruits;
- honey;
- dairy products.
Avoid foods that contribute to weight gain, which puts stress on the spine. Nutritionists do not recommend fatty, pickled, salted, smoked foods; they advise limiting sweets.
During the rehabilitation period, it is important to follow a diet
Possible complications
Cleaning the uterus is a simple, even routine procedure, but unpleasant consequences are not excluded. Among the most common problems that curettage leads to:
- Cervical rupture. It is more common in nulliparous patients and in those experiencing postmenopause.
- A through hole in the wall of the uterus. Perhaps because the surgical intervention is performed almost “blindly” with the hope of the accuracy of the gynecologist’s tactile sensations. Thinning and loosening of the mucosa increases the risk of such complications. Their elimination consists of suturing the walls of the reproductive organ or removing it.
- An inflammatory process affecting the uterus and its appendages. The reason is the colonization of the vagina with a large number of bacteria, both beneficial and harmful, which makes it difficult to maintain sterility when performing surgery. As a result, despite preparatory measures and the use of antibiotics, inflammatory processes still arise, develop and spread.
- Hematometra or collections of blood clots. Characteristic of nulliparous women. Treatment involves the procedure of vacuum aspiration for a frozen pregnancy and the use of oxytocin to contract the walls of the uterus.
The likelihood of severe complications is reduced if the operation is performed with clean vaginal smears of grade I-II. And:
- Antimicrobial prophylaxis is carried out.
- The procedure is carried out by a qualified, experienced doctor.
- The hysteroscopy method is used.
Video: Is curettage of the uterine cavity dangerous?
When to see a doctor during rehabilitation
Contact your doctor immediately if the following symptoms appear:
- back pain that does not subside and intensifies;
- burning in the area of the damaged disc;
- urinary disturbance;
- pain in the abdomen, arms, legs;
- numbness of hands, feet;
- heat;
- spasm, tension in the back muscles;
- too much swelling in the area of the diseased disc;
- ichor that oozes from the stitches.
These symptoms indicate complications that may result from infection in the wound, purulent inflammation, the onset of pathological narrowing (stenosis) of the spinal canal, when bone/cartilaginous structures affect the nerve roots, and other complications, including recurrence of intervertebral hernia.
When should you agree to curettage of the uterine cavity?
Cleaning is required in case of bleeding to stop, or if a pathological pregnancy is suspected. Curettage is also prescribed for the following conditions:
- Polyposis or endometrial hyperplasia, which was discovered after the end of menstruation and drug treatment.
- Detection of residual tissue after childbirth, miscarriage, abortion, and any discharge during menopause.
To avoid unnecessary interference in your body, do not be afraid to ask your gynecologist questions. If there is no understanding on his part, it is better to turn to other specialists. Disagree when answered “This is how we do it” instead of justifying the need for a traumatic procedure. But do not forget that these warnings apply to cases where there is no threat to the patient’s life.
Another effective office or outpatient method is hysteroscopy. It consists of inserting a thin optical tube with a lighting device at the end into the uterine cavity. Allows you to get a clear, enlarged image on your computer monitor. If a suspicious area is detected, a catheter is inserted into it for targeted removal of a piece of tissue.
After cleaning, a repeat hysteroscopy is performed to assess the quality of the intervention performed or establish a morphological diagnosis. The experience of RAMS specialists has shown that hysteroscopy speeds up the process of detecting a cancerous tumor and saves a woman from the unpleasant curettage procedure.
Video: Curettage of the uterus - what to take with you to the department
Approach to rehabilitation at Paramita
At the Moscow Paramita clinic, rehabilitation after surgery to remove a spinal hernia takes place in stages. A detailed recovery program is established based on:
- medical history;
- complexity of operations;
- concomitant diseases;
- age;
- gender;
- physical capabilities;
- data from laboratory tests, x-rays, MRI, etc.
After removal of a hernia, our doctors work with each patient according to an individual program. In the treatment of hernia, we use both Western and Eastern methods - physiotherapy, massage, hirudotherapy, acupuncture, etc.
The center has modern equipment at its disposal, which helps to quickly recover after surgery. Doctors closely monitor the progress of rehabilitation and adjust the program in a timely manner. We are always in touch with our patients and respond to all requests instantly.
We use non-surgical hernia treatment techniques
Read more about our unique technique
List of used literature:
- “Controversial issues of uterine artery embolization for uterine fibroids”, Issues of gynecology, obstetrics and perinatology, 2005, volume 4, No. 4, pp. 44-48 (co-authors V.G. Breusenko, I.A. Krasnova, S.A. Kapranov, V.B. Aksenova, B.Yu. Bobrov, N.A. Shevchenko).
- “Some controversial issues of uterine artery embolization in the treatment of uterine fibroids”, Obstetrics and Gynecology, 2006, No. 3, pp. 23-26 (co-authors V.G. Breusenko, I.A. Krasnova, S.A. Kapranov, B. Yu. Bobrov, V.B. Aksenova, N.A. Shevchenko, D.G. Aryutin).
- “Controversial issues of uterine artery embolization for uterine fibroids”, Issues of gynecology, obstetrics and perinatology, 2006, vol. 4, no. 4, pp. 44-49, (co-authors V. G. Breusenko, S. A. Kapranov, V. B.Aksenova, B.Yu.Bobrov, N.A.Shevchenko).
- “Embolization of the uterine arteries in the treatment of uterine fibroids”, Russian Medical Journal, 2006, No. 2, pp. 23-25, (co-authors Yu.E. Dobrokhotova, S.A. Kapranov, B.Yu. Bobrov, A.A. Alieva, I.I. Grishin).
- “Embolization of the uterine arteries - as a method of treating uterine fibroids,” in the book. Obstetrics and gynecology: modernity and traditions (edited by Yu.E. Dobrokhotova), Moscow, 2008, pp. 5-11) (co-authors A.A. Alieva, N.A. Litvinova, D.M. Magomedov, I .I.Grishin, O.I.Kauseva, S.A.Kapranov, Yu.E.Dobrokhotova).
Karmanov
Author: Kapranov S.A.
Doctor of Medical Sciences, Professor, twice Laureate of State Prizes of the Government of the Russian Federation in the field of science and technology, Laureate of the Lenin Komsomol Prize, author of more than 350 scientific papers on medicine, 7 monographs, and 10 patents for inventions in medicine
FAQ
When can you sit down after surgery?
Not until the spine is strong enough. If there are no problems, you can sit 4 weeks after the hernia surgery.
Are there relapses during the rehabilitation period?
They happen, but proper rehabilitation will reduce the risk of hernia recurrence.
How to eliminate leg pain during rehabilitation?
Leg pain after hernia removal is normal. The reason is the long-term pressure of the hernia on the nerves through which the brain controls the functioning of the legs. During surgery, the pressure is relieved, but it may take several weeks for the nerve tissue to recover. During this time, your lower leg will hurt, your hip will pull, and your limbs will experience numbness. If, while recovering, your leg suddenly begins to hurt sharply and go numb, be sure to tell your doctor. The sooner he determines the cause of the complication, the faster the chances of a speedy recovery, and you will not have to spend several years on treatment.
When can I plan a pregnancy after finishing rehabilitation?
You cannot plan to conceive within a year after removal of the hernia. The fetus will put pressure on the spine, causing a relapse. If you become pregnant, contact your doctor right away.
Is disability granted after completion of rehabilitation?
Rarely, only if the patient’s mobility has not been restored. The decision on disability is made by the ITU commission after a comprehensive examination. The status is assigned for six months, after which it must be confirmed. Your doctor will tell you whether you can get disability.
When is sick leave closed during the rehabilitation period?
If rehabilitation is successful, there are no complications, the doctor closes sick leave after the end of rehabilitation - after 2-3 months. After this, the patient can return to work or change it if it involves difficult working conditions.
Bibliography
- Badalyan L. O. Neuropathology. - M.: Education, 1982. - 317 p.
- Bogolyubov, Medical rehabilitation (manual, in 3 volumes). // Moscow - Perm. - 1998. - 1885 p.
- Popov S. N. Physical rehabilitation. 2005. - 608 p.
- Feshchenko, Ya. V. Non-surgical treatment and prevention of recurrence of intervertebral disc herniations / Ya. V. Feshchenko, L. D. Kravchuk // Pain. Joints. Spine. ─ 2014. ─ No. 3(15). ─ P. 59-61.
Themes
Intervertebral hernia, Spine, Pain, Treatment without surgery Date of publication: 03/26/2021 Date of update: 03/28/2021
Reader rating
Rating: 5 / 5 (1)
Pregnancy after curettage
You can’t even think about conceiving immediately after curettage, because the uterus is bleeding. The body must recover, especially if there was a connection with a frozen pregnancy or the need to remove embryonic tissue. Over 6 monthly cycles, not only the endometrial mucosa is restored, but also the woman’s hormonal background, which is seriously affected by the loss of the fetus. The reasons for an unsuccessful pregnancy must be excluded from your life so as not to provoke a new abortion.
If the cause was polyps or hyperplasia of the uterine wall, then you can plan conception already 2 months after the procedure. The body, which has not experienced a hormonal imbalance, recovers faster and is ready to bear and give birth to a healthy baby. In any case, doctors advise not to rush into conception, to get stronger and gain strength, which will be useful to the expectant mother. Features of pregnancy occurring after cleansing:
- High risk of placenta previa and miscarriage
. The reason is insufficiently restored endometrium. You will have to be under constant medical supervision and take supportive treatment to save the fetus. - In a nulliparous woman, when cleaning, the surgeon can damage the integrity of the muscle fibers of the uterine cervix.
As a result, the retaining function of this part of the reproductive system is disrupted and the child may be lost in the second trimester. The pathology is difficult to recognize and it is possible to prepare for it only at the next conception. - Damage to the growth layer of the endometrium
due to excessive cleaning.
Mental disorders from an unsuccessful pregnancy can provoke new pathological conditions that have a rather gloomy prognosis. In such cases, special help is required already at the “spiritual” level, so that the newborn is greeted by a joyful, warm mother.