Bile duct obstruction is a blockage or obstruction of the bile ducts. By their nature, bile ducts are channels emerging from the gallbladder. Their function is to transport bile from the liver to the small intestine. This transport occurs through the pancreas.
As for bile, it is a liquid produced by the liver. This liquid may have a dark green or yellow-brown tint. The main task of bile is to break down fats. Through the sphincter of Oddi, the vast majority of liver fluid passes directly into the small intestine. The remaining volume of bile is stored inside the gallbladder. When a person eats, the gallbladder releases liver fluid to digest food and absorb fats. In addition, bile rids the liver of accumulated waste.
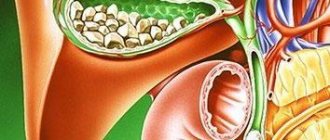
Cholelithiasis (GSD)
- a disease caused by impaired metabolism of cholesterol and bilirubin, characterized by the formation of stones in the gall bladder and bile ducts with the possible development of life-threatening complications.
Factors contributing to the formation of cholesterol and mixed gallstones:
- obesity,
- starvation,
- dyshormonal disorders in women associated with pregnancy, taking contraceptive medications,
- diseases of the ileum (Crohn's disease, etc.),
- irrational and unbalanced diet (food rich in fats, insufficient consumption of vegetables and fruits, etc.),
- gallbladder dyskinesia,
- age.
Factors contributing to the formation of pigment stones - black stones consisting of bilirubin and calcium and making up 70% of all radiopaque stones:
- chronic hemolytic anemia,
- alcoholism,
- alcoholic cirrhosis of the liver,
- chronic infections,
- helminth infections of the liver,
- age.
In 10-15% of cases, gallstones are diagnosed during a preventive ultrasound examination of the abdominal organs. The development of cholelithiasis (GSD) goes through several stages.
- first stage - there are no clinical symptoms of the disease, the diagnosis is based on the results of a study of gallbladder bile (the tendency to form stones is determined),
- the second stage is asymptomatic “stone carriage” in which most of the stones located at the bottom of the gallbladder remain asymptomatic,
- the third stage – with a pronounced complicated clinical picture (acute or chronic calculous cholecystitis, etc.).
The manifestations of cholelithiasis depend on the size of the stones, their location and the activity of the inflammatory process, the patency of the biliary system, as well as on the condition of other organs of the gastrointestinal tract.
Treatment
Before starting treatment, the patient should consult with a gastroenterologist and surgeon. Therapeutic tactics depend on the location of the blockage and the degree of obstruction. If the patient is in serious condition, he is transferred to the intensive care unit to stabilize his condition. An operation cannot be performed at this time, so they usually resort to minimally invasive techniques - nasobiliary drainage, percutaneous puncture of the gallbladder, cholecystostomy and choledochostomy.
When the patient's condition is stabilized, treatment with endoscopic techniques or extended surgery may be prescribed.
Options for housing and communal services
| Biliary (hepatic, biliary) colic. A stone lodged in the neck of the gallbladder closes the exit and causes biliary colic. A stone up to 0.5 cm in size will most likely pass into the lumen of the duodenum; a larger stone may lodge in the common bile duct, which will lead to the development of complete or intermittent obstruction (“valve stone”) with a typical clinical picture of biliary colic. The presence of stones in bile is always accompanied by inflammation (cholangitis). Colic is accompanied by intense short, “minute-long” pain with an interval of up to an hour, long-term recurrent pain in the right hypochondrium is characteristic of chronic cholecystitis. If the pain lasts more than 72 hours and is accompanied by fever, this is most often a sign of acute cholecystitis. Constant pain that continues continuously throughout the day is not typical for biliary colic. The pain is accompanied by flatulence and nausea. Acute cholecystitis. The main cause of the development of the disease is strangulation of a stone in the cystic duct. Characterized by fever and constant pain in the right hypochondrium. Typical pain in acute cholecystitis occurs in less than 50% of patients. Most often, pain occurs soon after eating and increases in intensity over an hour or more. Fever usually appears 12 hours after the onset of the attack and is associated with the development of inflammation. The pain becomes constant. Acalculous acute cholecystitis is extremely rare and can occur secondary to salmonellosis, sepsis and trauma. Complications of acute cholecystitis.
Chronic calculous cholecystitis. Usually characterized by recurrent attacks of biliary colic, less often by constant pain. The development of an attack is provoked by fatty foods, spices, smoked foods, hot seasonings, severe physical stress, working in an inclined position, as well as infection. Less commonly, colic occurs “for no reason.” Usually accompanied by fever, nausea, and sometimes vomiting. The pain intensifies with movement and deep breathing. Sometimes the pain radiates to the heart area, simulating an attack of angina. The pain is varied - from intense cutting to relatively weak aching. Vomiting with cholecystitis does not bring relief. In women, colic sometimes coincides with menstruation or occurs after childbirth. Choledocholithiasis (common bile duct stones) occurs when a stone from the gallbladder enters the common bile duct. Symptoms are characterized by pain in the right hypochondrium similar to biliary colic, fever, chills, jaundice and characteristic changes in blood biochemistry. Cholangitis. A variant of the course of gallstone disease is accompanied by pain in the upper abdomen, jaundice, fever, and often chills. Bacterial cholangitis is one of the most dangerous complications of cholelithiasis; it is usually associated with cholestasis, which occurs when a stone blocks the common bile duct. The severity of cholangitis depends, first of all, on the duration of cholestasis and the level of cholemia. Gangrene and empyema of the gallbladder are manifested by sepsis, a serious condition of the patient with symptoms of peritonitis. Requires immediate medical attention. Empyema is an acute purulent inflammation of the gallbladder, characterized by intoxication and a high risk of perforation. Open perforation into the abdominal cavity is accompanied by peritonitis, causing high mortality (up to 25%). Bile stasis in the gallbladder is hypomotor dyskinesia of the gallbladder. As a rule, it accompanies cholelithiasis. Stasis of bile in the gallbladder is usually manifested by constant dull aching pain in the right hypochondrium, aggravated by shaking, walking quickly, carrying a heavy object in the right hand, or bending forward. It is also observed during pregnancy, long-term use of antispasmodics, after vagotomy, diabetes mellitus, obesity, i.e. for conditions and diseases that are risk factors for the development of cholelithiasis. |
Treatment: surgical. Absolute indications for surgery:
- acute cholecystitis,
- chronic cholecystitis with recurrent biliary colic,
- non-functioning gallbladder,
- common bile duct stones,
- gangrene of the gallbladder.
Diagnosis of deviation
First of all, a blood test and liver function test are performed. A blood test can help rule out an incorrect diagnosis. In particular, such a measure will not allow the obstruction to be confused with inflammation of the gallbladder, inflammation of the bile duct, or increased concentrations of alkaline phosphatase or liver enzymes.
Magnetic resonance cholangiopancreatography is considered a good assistant in making a diagnosis. It almost accurately detects blockage of the bile ducts. Very often, endoscopic retrograde cholangiopancreatography is used for diagnostic purposes. This procedure is universal. It allows not only to examine the bile ducts, but also to take tissue for analysis.
CHRONIC AALCTIC CHOLECYSTITIS (CAC)
It occurs much less frequently than is diagnosed. If there is a clinical picture of chronic cholecystitis, it is necessary to exclude, first of all, cholelithiasis and parasitic infestations. CBC can be caused by microbial flora. The infection can enter the gallbladder from the gastrointestinal tract through the common bile and cystic ducts (ascending infection). Downward spread of infection from the intrahepatic bile ducts is also possible. The development of the inflammatory process in the gallbladder is promoted by stagnation of bile. CBC is characterized by a long progressive course with periods of remissions and exacerbations, aching pain in the right hypochondrium, less often in the epigastric region, lasting for many hours, days, sometimes weeks. The occurrence or intensification of pain is associated with the consumption of fatty and fried foods, eggs, cold and carbonated drinks, wine, beer, and spicy snacks. The pain may be combined with nausea, belching, bloating, and fever. There is a constant feeling of heaviness in the upper abdomen. Treatment. Diet, fractional meals, pain relief, anti-inflammatory and antiparasitic therapy, taking enzymes.
Contraindications to bile duct stenting
- Disintegration of the tumor with the development of bleeding.
- Severe stenosis of the bile duct, in which it is impossible to bring endoscopic surgical instruments to it.
- The presence of intestinal obstruction (operations are carried out after relief of this condition).
CHOLESTATIC (subhepatic) JAUNDICE
Cholestatic jaundice develops when there is an obstruction to the flow of bile at any level of the biliary system. Obstructive or subhepatic (obstructive) jaundice develops when bile flow is obstructed at the level of the extrahepatic bile ducts (choledochal stones, pancreatic cancer, chronic pancreatitis, post-traumatic narrowing of the common bile duct, pancreatic pseudocysts, etc.). 70% of cases are associated with stones in the common bile duct and cancer of the head of the pancreas. Intrahepatic cholestasis is most often observed in acute drug-induced hepatitis and primary cirrhosis, less often in viral, alcoholic hepatitis, cholangitis, liver cirrhosis, metastases, etc. Jaundice develops slowly, often preceded by itchy skin. It is typical for both extrahepatic and intrahepatic cholestasis. Diagnostic criteria:
- light-colored (non-pigmented) stools
- dark brown urine
- traces of scratching on the skin,
- yellowish gloss of nails,
- xanthelasma (cholesterol deposits on the eyelids),
- xanthoma (cholesterol deposits on the palmar folds and tendons),
- hepatomegaly – enlargement of the liver.
When blocked by a stone, jaundice develops within 24 hours after the onset of pain, and fever occurs due to developing cholangitis. Itchy skin does not occur in all patients. Unlike a tumor, long-term stone blockage is rarely complete. Diagnostics: Laboratory tests of blood, feces, urine. Instrumental diagnostics: Ultrasound, CT, MRI diagnostics with contrast, Endoscopic diagnostics.
Surgical relief of obstruction
If a person is diagnosed with pancreatic cancer, doctors install a stent in the narrowed area of the bile duct. First, specialists insert an endoscope into the esophagus, and then pass it into the stomach and at the very end reach the duodenum. Such actions help to study the blocking site for proper stent placement. Before taking an x-ray, a dye is injected into the patient's body, which will also ensure the correct placement of the device. If obstruction recurs, the medical device is replaced.
POSTCHOLECYSTECTOMIC SYNDROME
In 15% , pain and dyspeptic disorders remain or recur These symptoms are associated with impaired motility of the sphincter of Oddi, dyskinesia of the extrahepatic bile ducts and duodenum . The main features are:
- recurrent colicky pain in the right hypochondrium,
- fat intolerance,
- diarrhea,
- bloating.
Patients often have duodenogastric reflux, antral gastritis, duodenitis, causing a feeling of heaviness and pain in the epigastrium, nausea, bitterness in the mouth, flatulence, unstable stool, etc. Inflammation of the gastroduodenal mucosa is usually associated with a microbial factor and the damaging effect of bile acids
Mechanical jaundice. Pancreas cancer
Return to section:
Department of X-ray surgical methods of diagnosis and treatment
Obstructive jaundice - what is it?
Rice. 1 - The anatomical structure of the biliary tract is normal |
First, let me remind you: bile is formed in the liver, after which it enters the duodenum through the bile duct system, where it helps digest food. The gallbladder is a kind of “reservoir” where bile “accumulates” between meals (Fig. 1).
So, any obstacle to the “movement” of bile into the intestine forms a pathological condition called “obstructive jaundice.” Bile begins to accumulate in the bile ducts and gallbladder, enlarging and expanding them. Excess bile is released into the blood, and the body removes it through other routes, including the kidneys and skin. Therefore, one of the initial signs of obstructive jaundice is an increase in bilirubin in the blood, a bile pigment that is the main component of bile. Since bile does not enter the intestines and does not color the stool, it becomes light, even gray. The urine becomes very dark due to increased secretion of bilirubin by the kidneys. The skin turns yellow, and due to an excess of bile salts in the blood, severe skin “itching” may begin.
Thus, “obstructive jaundice” is a pathological syndrome associated with a violation of the outflow of bile, which is externally manifested by yellowing of the sclera and skin, lightening of the stool and darkening of the urine, and can cause weakness, drowsiness, abdominal discomfort and itching. Quickly identifying the cause of this syndrome (that is, making a diagnosis) is the main task of the doctor in this situation.
Obstructive jaundice: causes.
| Rice. 2 The most common causes of obstructive jaundice. |
There are many diseases that cause disruption of the flow of bile.
The main ones are listed in Figure 2.
The method of treatment, its result, as well as the prognosis of the disease (i.e., the expected duration and quality of life with this disease and its "curability").
Unfortunately, in 40-67% of cases, the cause of obstructive jaundice is tumors, and they are benign only in 2-3% of cases.
The most common cause that doctors have to deal with is cancer of the head of the pancreas.
The tumor compresses the duct from the outside, disrupting the outflow of bile. (Fig. 3)
Obstructive jaundice in pancreatic cancer - treatment methods
| Rice. 3 Compression of the common bile duct due to a tumor of the head of the pancreas. |
It is impossible to consider all possible types of treatment for various causes of obstructive jaundice in one article. Therefore, I will dwell in more detail on treatment options for the most difficult category of patients - those with malignant tumors that cause compression of the bile ducts.
The only chance for patients with a malignant tumor causing obstructive jaundice is radical surgery (complete removal or resection of part of the organ), but this is possible in less than 30% of cases. This happens because the disease develops very slowly and begins to “manifest” already at an advanced stage.
In each case, the question of the possibility of complete tumor removal is decided individually; it depends on many factors: the extent of the process, the age of the patient, the presence of concomitant diseases, etc. These operations are considered one of the most difficult in modern abdominal surgery and are performed, as a rule, in specialized departments by experienced oncologist surgeons.
All other methods of treatment - radiation, chemotherapy (so-called dietary supplements, phyto- and homeopathic therapy, I do not consider “treatment” in principle) are ineffective and are aimed only at slowing down the growth of the tumor and improving the “quality of life” of the patient.
Why is obstructive jaundice dangerous?
As I already mentioned, the main parameter that assesses the severity of obstructive jaundice is the level of total bilirubin in the blood. All of the above treatment methods, including radical surgery, with rare exceptions, are possible when the level of total blood bilirubin is below 50-90 µmol/l (normal 3-17 µmol/l) due to the high risk of complications. However, visible jaundice of the sclera and skin occurs, as a rule, when the bilirubin level is above 100-120 µmol/l. At levels above 300-350 µmol/l, bilirubin begins to penetrate the blood-brain barrier, i.e. enter the brain and, with further growth, cause severe intoxication, even death.
According to the literature, in conditions of biliary tract obstruction and inflammation, surgical treatment is risky, accompanied by a large number of complications, and mortality reaches 10-34%, which is 4 times higher than in cases where obstructive jaundice can be eliminated before surgery.
Therefore, one of the first tasks in the treatment of obstructive jaundice is to reduce the level of bilirubin in the blood - to treat intoxication and prepare the patient for one or another type of specialized medical care (surgery, chemotherapy or radiation therapy).
Choosing a treatment method for obstructive jaundice
Conservative therapy (intravenous infusions of drugs) in patients with obstructive jaundice of tumor origin is rarely effective. of decompression of the bile ducts come to the fore - i.e. methods aimed at restoring the outflow of bile from the bile ducts into the digestive tract. Among the surgical methods for treating obstructive jaundice, three main areas can be distinguished:
decompression of the bile ducts – i.e. methods aimed at restoring the outflow of bile from the bile ducts into the digestive tract. Among the surgical methods for treating obstructive jaundice, three main areas can be distinguished:
- Endoscopic techniques for drainage and stenting of the bile ducts.
- Percutaneous transhepatic techniques under ultrasound and fluoroscopy control.
- Open surgery is the creation of an “anastomosis” (i.e., “connection”) between the bile ducts and the intestine, bypassing the tumor.
The latter method is used quite rarely today, as it is associated with a greater number of complications. It is used when it is technically impossible to perform the operation using the first two methods or when there are no specialists of the required profile in the hospital.
The choice between endoscopic (“retrograde”) (Fig. 4) or percutaneous transhepatic (“antegrade”) (Fig. 5) techniques, all other things being equal, largely depends on the specific situation.
| Rice. 4 “Retrograde” stenting of the common bile duct using an endoscope for the treatment of obstructive jaundice caused by compression of the common bile duct by a pancreatic tumor. | Rice. 5. “Antegrade” - percutaneous transhepatic drainage of the bile ducts for obstructive jaundice caused by Klatskin’s tumor |
Thus, for the technical feasibility of percutaneous puncture under ultrasound control, a necessary condition is the expansion of the intrahepatic bile ducts. At the same time, the use of endoscopic techniques in patients who have previously undergone surgery on the stomach or duodenum, as well as with obstructive jaundice caused by a tumor in the “gate” of the liver, is difficult and, at times, impossible.
In 70-80% of patients with obstructive jaundice, it is possible to use both methods of decompression, and then the choice largely depends on how common one or another method is in a particular hospital (technical equipment, experience of a particular specialist, on whom it largely depends percentage of successful interventions and number of complications).
Obstructive jaundice - surgical treatment in St. Petersburg
The State Budgetary Healthcare Institution “City Hospital No. 40” has implemented the ability to provide urgent and emergency medical care to patients with obstructive jaundice of any etiology using all of the listed methods. The availability of the latest equipment and experienced specialists allows us to provide timely, highly qualified medical care to this complex category of patients.
More information about minimally invasive methods of percutaneous transhepatic drainage and stenting of the bile ducts for relieving obstructive jaundice can be found in the second part of the article.
Percutaneous transhepatic drainage and stenting of the bile ducts for the treatment of obstructive jaundice.
As a specialist x-ray surgeon, I would like to dwell in more detail on the technique of percutaneous transhepatic decompression of the bile ducts for the malignant nature of obstructive jaundice.
Percutaneous transhepatic cholangiography – conditions for implementation, advantages and disadvantages of the method.
A necessary condition for performing percutaneous puncture is the expansion of the intrahepatic bile ducts to 3-5 mm. With obstructive jaundice of any etiology, this phenomenon is quite common; if the outflow of bile is disrupted, it begins to accumulate primarily in the ducts, gradually expanding them. If an obstacle (stone or tumor) does not completely compress the common bile duct, i.e. Some bile still flows into the intestine, but this process may take some time.
Fig.1. X-ray operating room.
Advantages of the method:
- Performed under local anesthesia (i.e. does not require general anesthesia)
- In experienced hands, the rate of successful drainage is 98-100% (which exceeds the technical success of endoscopic methods).
- Fewer complications (if the necessary equipment and experienced specialists are available).
Disadvantages of the method:
- It is performed under the control of fluoroscopy (although modern equipment makes it possible to reduce the radiation dose to minimal figures - less than during computed tomography).
- When installing external or external-internal cholangiodrainage, part of the bile flows into a special plastic container, which must be carried with you for 3 to 14 days, which worsens the patient’s quality of life.
In the hospital, patients with obstructive jaundice are admitted to the surgery/oncology departments. As a rule, operations aimed at decompressing the bile ducts are urgent - i.e. urgent enough to avoid complications associated with bilirubin intoxication, but at the same time not performed immediately upon admission of the patient. Usually doctors have 1-3 days to further examine the patient - to determine the cause of jaundice (stone, tumor, stricture), determine the level of bilirubin in the blood, and other tests that need to be taken into account when preparing for surgery.
The purpose of the operation, its risks and possible complications are explained to the patient, and voluntary informed consent to the procedure is signed. A light dinner is allowed the day before, and fasting on the day of intervention.
Percutaneous transhepatic drainage for pancreatic and bile duct cancer.
Rice. 2. Puncture of the bile ducts under ultrasound control on the right in the 8th intercostal space.
Percutaneous transhepatic cholangiodrainage (PTCHD) and stenting operations are performed in a specially equipped cath lab.
The intervention is performed under local anesthesia, usually 20-30 ml of a 1% lidocaine solution. In our hospital, an anesthesiologist-resuscitator is always present in the operating room, who, if necessary, provides intravenous anesthesia.
The puncture site is selected individually, depending on the anatomical structure and location of the obstacle. As a rule, access to the ducts of the right lobe of the liver is carried out from the 7-8 intercostal space along a line drawn perpendicular to the anterior angle of the axilla. Access to the ducts of the left lobe is from under the xiphoid process.
The correct choice of access has the greatest impact on the safety of the technique.
How is bile duct drainage surgery performed?
After treating the skin with an antiseptic solution and anesthesia, the skin at the puncture site is incised with a scalpel to facilitate insertion of the puncture needle. The needle itself has a diameter of less than 1 mm. Under ultrasound or fluoroscopy control, it is carried out to a depth of 5-10 cm until it enters the dilated bile duct.
Several milliliters of a non-ionic iodine-containing contrast agent (Omnipaque, Optireum) are injected through a needle. This is done to ensure that it enters the bile duct and not the liver vessels. A thin soft conductor with a diameter of up to 0.3 mm is inserted through the lumen of the needle, the needle is removed, and a thin plastic catheter (diameter less than 2 mm) is inserted along the installed conductor. Through it, 20-30 ml of contrast agent is injected - the so-called. Cholangiography.
| Rice. 3. Percutaneous transhepatic cholangiography. | Percutaneous transhepatic cholangiography. The following is determined: a) pronounced expansion of the intrahepatic bile ducts; b) complete block in the distal third of the common bile duct (compression of the head of the pancreas by the tumor) |
| Rice. 4. Cholangiography for obstructive jaundice caused by Klatskin tumor. | Cholangiography for obstructive jaundice caused by Klatskin tumor. A pronounced narrowing of the right (a) and left (b) lobar bile ducts is determined due to the germination of cholangiocarcinoma. Tight filling of the bile ducts allows you to accurately determine the level and degree of blockage of the bile ducts, the degree of their expansion, defects in their filling (large stones and intraluminal tumors are visible), as well as determine the tactics and method of further treatment - decompression of the bile ducts. |
| Rice. 5. Cholangiography for intrahepatic cholangiolithiasis | Cholangiography for intrahepatic cholangiolithiasis: a) multiple small concretions (stones) up to 2-3 mm in size inside the dilated bile ducts of the right lobe of the liver; b) benign (post-inflammatory) stricture of the terminal part of the common bile duct; c) entry of the contrast agent into the duodenum through the installed percutaneous transhepatic drainage. Bile obtained during primary puncture of the bile ducts is often taken for culture and determination of sensitivity to antibiotics. This greatly helps to combat such a common complication of obstructive jaundice as cholangitis - i.e. inflammation of the wall of the bile duct. |
Rice. 6 - Drainage tube for percutaneous transhepatic drainage of the bile ducts. | After determining the level of the block, the doctor, using catheters of various shapes and conductors of different stiffness, performs recanalization of the obstacle (the conductor is passed through the stricture or the common bile duct compressed from the outside into the small intestine). A plastic tube with a diameter of about 3 mm with a large number of holes is inserted into the intestine along the guide to restore the outflow of bile - drainage. It is positioned so that the drainage holes are located both before and after the obstacle. Thus, bile enters the drainage tube before the obstruction and exits the openings into the intestine after it. |
For the first 2-3 days, a plastic bag is connected to the outer end of the drainage (in the intercostal space). This allows you to eliminate excess bile located in the ducts and control (in time identify) possible complications, such as hemobilia - bleeding into the bile ducts.
If the obstacle cannot be passed, then drainage is left only for external outflow in order to reduce the level of bilirubin in the blood and its toxic effects. In such cases, the patient has to drink bile (along with juice or water), since with it the necessary liquid and microelements that are necessary for an already exhausted body are lost. After a few days, when the inflammation and swelling of the wall of the bile ducts passes, as a rule, a second attempt is made to pass the obstacle. After installing the drainage in the desired position, it is fixed to the skin with a suture, which reduces the risk of its displacement.
Treatment after a decrease in bilirubin levels. Caring for bile duct drainage.
Rice. 7. External-internal percutaneous transhepatic cholangiodrainage.
The success of drainage largely depends on the availability in the hospital of the entire range of instruments and the experience of the surgeon performing the intervention. In our department, the success of external-internal drainage with restoration of normal passage of bile into the intestine is 98-99%.
In the case where, after a decrease in the level of bilirubin in the blood, radical surgery is possible (i.e., completely eliminating the root cause of obstructive jaundice), the drainage is removed during or after this operation. In cases where the process is inoperable, the drainage is closed after a few days and remains with the patient on an ongoing basis. It must be washed - once a day, by injecting 20 ml of saline solution into the drainage. This is done in order to avoid its rapid “clogging” with bile salts or so-called “sludge” - thick stagnant bile. Patients are prescribed drugs that “thin” bile, such as Ursosan. Despite all these measures, the drainage has to be changed every 4-6 months. This happens quite quickly, since there is no need for repeated puncture of the bile ducts and the drainage channel has already been formed.
However, even the presence of a foreign body in a patient for a long time, even a thin plastic tube without a bag, causes psychological discomfort and reduces the quality of life. By itself, the drainage can shift and cause inflammation when food enters the bile ducts through its openings from the intestine; Bile may leak through the external drainage channel and stain clothing.
Stenting of the bile ducts for obstructive jaundice.
In order to avoid these complications, bile duct stenting surgery was developed in patients with inoperable malignant process (in some cases with other causes of obstructive jaundice). In fact, it is a logical continuation of the drainage operation, and, if possible, is performed on a stable patient with a satisfactory prognosis for survival.
Stenting of the bile ducts is usually performed 1-4 weeks after drainage surgery, after assessing the dynamics of the decrease in bilirubin levels and preparing the patient. It is performed through the same access - a thin conductor is inserted into the intestine through the existing drainage, after which the drainage tube is removed. A special balloon is inserted along this guide, which is positioned inside the stricture (benign or malignant), and opened for a minute for “plasticity” of the common bile duct - i.e. expanding it to allow insertion of a mesh metal structure – a stent – into it.
The diameter of the opened balloon is 6-8mm. The balloon is deflated and removed, and a stent is inserted along the same guidewire.
| Rice. 8. Bile duct stent | Rice. 9. Balloon catheter for “plasty” of common bile duct strictures. | Rice. 10. Balloon plasty of malignant common bile duct stricture before stent placement. A balloon with a diameter of 6 mm (a) is opened on a guide (b) in the area of the stricture. |
The size of the stent is determined in advance, according to the data of cholangiography. Most modern stents are coated with a special material (looks like fabric on the outside). Such stents are called “grafts” and have a much lower percentage of “tumor growth” through it - and therefore relapse of obstructive jaundice.
The stent (like the balloon) is rolled up on a special delivery system, which is quite thin and does not require additional expansion of the channel in which the drainage was previously located.
The stent is inserted and opened in such a way as to block the stricture, but not block the remaining bile ducts.
| Rice. 11. Stent-graft with polytetrafluoroethylene coating for stenting of bile ducts. | Rice. 12. Stent-graft installed in the common bile duct from the confluence of the lobar bile ducts (a) to the duodenum (b) for the treatment of obstructive jaundice caused by metastases of colon cancer to the porta hepatis. |
If necessary, intravenous anesthesia is added at the time of balloon and stent deployment. After installation of the stent, the patient is observed for several days in the surgical department, then, after making sure that there are no complications, he is discharged to continue treatment (chemotherapy, radiation therapy, photodynamic therapy) in a specialized institution or at the place of residence (symptomatic therapy).
Obstructive jaundice is the cost of an operation where drainage and stenting of the bile ducts are performed.
In most hospitals in St. Petersburg, minimally invasive operations are performed for a fee, because require quite expensive consumables and the presence of experienced specialists.
St. Petersburg State Budgetary Healthcare Institution “City Hospital No. 40” provides residents of St. Petersburg with the opportunity to perform such operations free of charge, using coupons for the provision of high-tech specialized medical care within the framework of the compulsory medical insurance program.
Doctor on X-ray endovascular methods of diagnosis and treatment, oncologist Popov V.V.
← Back
Contraindications
There are no absolute contraindications to ultrasound of the biliary tract, except for the reasons why the examination will be uninformative. Such conditional contraindications include:
- a patient with skin lesions at the time of exacerbation;
- the presence of wounds, purulent skin lesions;
- presence of scars in the abdominal area.
With such lesions, the ultrasound probe will not be in close contact with the skin, which will prevent the penetration of ultrasonic waves to the required depth, and it will be difficult to obtain complete information about the condition of the area under study.
Symptoms of oncopathology of the bile ducts
In the early stages, the tumor often does not show any signs. Symptoms usually occur when the flow of bile is disrupted. In addition, the clinical picture depends on the location of the malignant tumor. With intrahepatic bile duct cancer, symptoms develop much later, often when the tumor has time to spread widely in the body.
The main manifestations of bile duct cancer:
- Obstructive jaundice is a condition in which the outflow of bile is disrupted, a toxic breakdown product of hemoglobin, bilirubin, enters the blood, and because of this, the skin and mucous membranes turn yellow.
- Itchy skin also occurs due to increased levels of bilirubin in the blood.
- Dark urine and light-colored stool - These symptoms occur because bile cannot pass into the intestines, and the body tries to reduce the level of bilirubin in the blood by excreting it through the kidneys.
- Abdominal pain - localized in the upper right.
- Decreased appetite.
- Weight loss for no apparent reason.
- Increased body temperature.
- Nausea and vomiting.
Biliary tract cancer is a fairly rare disease. If you are bothered by the symptoms on this list, this does not mean that you have a malignant tumor. Most often, such manifestations indicate other diseases of the liver, gallbladder and pancreas. However, in each case it is necessary to exclude oncological pathologies. Visit your doctor and get examined.
Preparation for the procedure
In preparation for GB stenting, the patient undergoes a comprehensive examination, which includes a number of laboratory tests and instrumental research methods:
- General and biochemical blood tests.
- Coagulogram is an analysis that reflects the functioning of the blood clotting system.
- Ultrasound examination of the liver and bile ducts.
- Retrograde cholangiography is a study of the patency of the gallbladder.
If necessary, a CT and/or MRI is performed, which will clarify the duration of the stenosis and better plan the operation.
Prevention
Many risk factors for the disease, such as age, congenital pathologies, and bile duct abnormalities, cannot be influenced. However, there are some ways to reduce the risks:
- You need to maintain a healthy weight throughout your life, and physical activity and proper nutrition will help with this.
- Stop smoking and drinking alcohol.
- Vaccination protects against viral hepatitis B.
- Avoid promiscuous sex, use condoms - this will help protect against infection with viral hepatitis.
- If you have been diagnosed with hepatitis B or C, you should see your doctor regularly and receive treatment.
Book a consultation 24 hours a day
+7+7+78