What is pancreatitis
Pancreatitis in medicine refers to the inflammatory process in the pancreas, the development of which is caused by:
- Galloon pathologies, stomach, duodenum;
- Unhealthy diet;
- diabetes;
- Severe poisoning;
- Injuries, surgery in the abdominal area.
The disease often occurs during pregnancy or during drug therapy with estrogen, glucocorticosteroids, sulfonamides, tetracyclines. The risk of developing pancreatitis is present in infectious diseases (hepatitis, chickenpox, swine), and the presence of a genetic predisposition to gastrointestinal disorders.
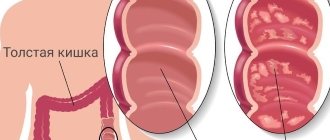
The disease develops against the background of impaired outflow of enzymes and digestive juices in the small intestine. Their accumulation leads to compression of the pancreatic wires, the development of inflammation and swelling. Destructive processes are activated in the Orguard patient, and Gland begins to digest.
Disease progression is associated with the death of pancreatic tissue and the vessels and organs adjacent to the pancreas. This leads to a serious deterioration in the patient's condition and even death.
Diagnosis of “Pancreatitis”
True (primary) pancreatitis is a very rare diagnosis. Its cause in most cases is alcohol abuse. Frequent drinking of alcohol causes impaired motility in the sphincter of Oddi, because of this, protein plugs form in the pancreatic ducts, the outflow of enzymes is disrupted and pressure of pancreatic juice occurs on the tissue of the gland itself. This causes pain and inflammation. Long-term use of large amounts of medications is also a fairly common cause of pancreatitis. The disease can also be triggered by systematic poor nutrition, alcohol, frequent stress and hormonal imbalances.
More common is secondary (reactive) pancreatitis, which occurs against the background of disorders in the gastrointestinal tract. The main reason for the development of secondary pancreatitis is problems with the gallbladder (for example, cholecystitis - inflammation of the gallbladder, cholelithiasis, postcholecystectomy syndrome, bile duct dyskinesia and chronic gastroduodenitis). Thus, the development of pancreatitis is a consequence of other previous diseases of the stomach and gall bladder. In children, the disease may appear after viral infections and influenza. True, this happens quite rarely.
How does it affect blood pressure?
You may be under the impression that there is no strict relationship between blood pressure and the pancreas. In fact, the situation is completely different. Blood pressure in pancreatitis can both rise and fall. The first option is possible during the attack of an acute disease, while the second option more often appears in patients with a chronic form of pathology and internal bleeding (bleeding).
During exacerbation and in the acute stage
Increasing severity of pancreatic disease causes the most severe feelings of pain. This condition releases stress hormones into the bloodstream and increases the activity of the autonomic nervous system. The patient's blood vessels are disturbed and the overall blood flow is impaired.
Increased blood pressure in the acute phase of pancreatitis occurs against the background of psycho-emotional stress and metabolic disorders. This leads to disruption of the mechanisms that control the arteries.
Worsening of pancreatitis can lead to the development of a breakthrough of excess pressure and its typical complications. Often the increase in pressure is short-lived and gives way to hypotension.
In remission and chronic course
Chronic inflammation of the pancreas is characterized by hypertensive pressure, leaving patients alternately with hypertension and hypotension.
Factors that contribute to frequent fluctuations in blood pressure:
- Inability of the pancreas to perform basic functions (this leads to nutritional deficiency, insufficient absorption of micro- and macroelements necessary to maintain the proper functioning of blood vessels and myocardium, provokes poisoning of the body).
- Swelling of the patient, leading to depression of the surrounding lymph nodes, blood vessels, nerve endings, activation of the autonomic system and increased pressure.
- Insufficient production of insulin by the pancreas, a hormone necessary for the proper use of glucose. As a result of this malfunction, the development of diabetes occurs.
Patients with pancreatitis often develop diabetic nephropathy, in which sodium is not excreted from the body, stopping fluids. This leads to an increase in total blood volume and blood pressure increases.
Consequences of pancreatitis for the body
Inflammation of the pancreas, called pancreatitis, occurs due to a violation of the outflow of pancreatic enzymes from the gland. After this, enzymes begin to destroy the pancreas, digesting it. Such processes are often accompanied by stagnation of bile. In the intestines at this time the situation is not much better: the lack of enzymes does not allow it to digest food, and it begins to rot. The result of a combination of pathological processes is poisoning and complete failure of the digestive system.
Such changes have a serious impact on the functioning of the autonomic nervous system, blood vessels and lymphatic systems, which, in turn, leads to changes in blood pressure.
Symptoms of high blood pressure with pancreatitis
If high blood pressure and pancreatitis occur together, the patient will experience the following symptoms
- dizziness;
- Impaired temporary vision;
- headache;
- Ears;
- Palpitations;
- numbness of fingers;
- "Goose bumps" on the skin;
- sleep disorders;
- Excessive nerve stimulation.
Pancreatic hypertension can cause swelling of the face and limbs, hyperhidrosis (increased sweating) and heart pain. A sudden increase in blood pressure is often accompanied by severe epigastric pain, which then moves to the lumbar region.
A sudden increase in blood pressure is a symptom that accompanies pain shock, indicating the development of an attack of acute pancreatitis or the manifestation of pancreatic necrosis.
Stages of pancreatitis
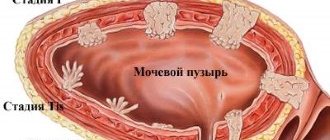
Staging of pancreatitis is very important because it determines the therapeutic strategy.
- The first stage does not manifest itself in any way, the patient does not suspect anything, which is why it is called “preclinical”. At this stage, pancreatitis is discovered by chance during an examination for another reason, when, for example, CT scan reveals changes in the gland tissue.
- The appearance of symptoms of the disease is designated as the second stage, during which exacerbations with pronounced manifestations already occur, and between attacks there is an almost normal life for an almost healthy person. Gradually, the severity of exacerbations decreases, but the symptoms occur even between attacks, so there is no feeling of health at all, but there is a feeling of constant discomfort. On average, this stage lasts about 5 years.
- At the third stage of chronic pancreatitis, pancreatic insufficiency already appears, clinical signs do not disappear, they are constant.
- The fourth stage occurs almost without pain, there are no acute attacks, but with clear signs of insufficient pancreatic function.
Diagnosis
According to medical statistics, in 65% of cases, arterial hypertension is caused by a malfunction of the pancreas. Therefore, in the case of periodic increases in blood pressure, mandatory examination for pancreatitis is recommended.
The main diagnostic measures will be:
- Anamnesis collection.
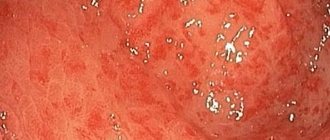
- External examination of the skin, palpation of the abdominal cavity.
- Clinical and biochemical blood test.
- Urine and stool analysis.
- Ultrasound examination of internal organs.
If complications occur, the patient is prescribed computed tomography (CT) or endoscopic retrograde cholangiopancreatography (ERCPG). Less commonly, in case of damage to the pancreas, laparoscopy, abdominal radiography and fibrogastroduodenoscopy (FGDS) are used.
When blood pressure drops
Elevated blood pressure during an attack of pancreatitis is quickly followed by a decrease in blood pressure. The torpid phase of shock begins, having three degrees of severity:
- First degree. Systolic pressure drops to 90-100 mmHg. Art. The heart rate increases, weakness is observed, and the reaction to external stimuli is inhibited. The pain is still present. At this time, antispasmodics and analgesics must be prescribed.
- Second degree. The upper pressure reading drops to 75-90 mmHg. Art. Pulse and breathing quicken. If there is a lack of fresh air, fainting may occur. The patient continues to be given medications to relieve pain, drugs that support heart function are added, and solutions are administered intravenously to replenish the lack of fluid in the body.
- Third degree. The pressure drops to 65-70 mm Hg. Art. The heartbeat is barely noticeable, the hands and feet are cold, the skin is pale blue, breathing is weak, and renal failure is severe. In the absence of urgent resuscitation measures, the person dies.
A decrease in blood pressure is sometimes caused by significant blood loss. With pathological destruction of the pancreas, internal bleeding is possible.
Treatment methods
To normalize blood pressure, pancreatitis and other parallel diseases are successfully treated. When the pathology worsens, the patient is hospitalized. In addition to pharmacological treatment, the patient is advised to fast and rest. Chronic pancreatitis requires adherence to a diet and a course of enzyme analgesics.
Medication
Among the drugs for acute pancreatitis, arterial hypertension progresses:
- Antispasmodics (Papaverine, No-shpa).
- Painkillers (Analgin, Baralgin).
- Anti-dehydration medications (Regidron, Alvogen).
The patient is prescribed detoxification therapy, administration of saline and colloidal solutions. General treatment helps eliminate vascular spasm, relieve swelling of the pancreas and adjacent tissues, and reduce the activity of the autonomic nervous system. Patients with acute pancreatitis are not prescribed antihypertensive tablets. This helps avoid the risk of a sudden drop in blood pressure and the development of collapse.
In the chronic form of pancreatitis, accompanied by increased blood pressure, the patient requires constant antihypertensive maintenance therapy. The administration of ACE inhibitors, beta-blockers and diuretics becomes important.
To normalize the functioning of the pancreas, it is advisable to take Pancreatin, Festal. To suppress secretory functions, a course with Contrical helps. The patient still needs to follow the diet rules.
Patients who simultaneously suffer from pancreatitis, hypertension and diabetes mellitus need to additionally take medications that lower blood sugar levels, stimulate insulin production, hormonal drugs, and statins.
Surgery
The department of surgical intervention is decided by specialists in cases where traditional treatment of pancreatitis does not bring relief to the patient. In such cases, irrigation, abdominal irrigation and drainage are indicated. In rare cases, surgeons perform necrectomy, that is, removal of diseased tissue from a diseased organ. If there are appropriate indications, resection of the gallbladder is performed in remission.
ethnoscience
Before using folk remedies for pancreatitis complicated by hypertension, it is necessary to obtain the consent of the attending physician. If the specialist deems it necessary, the patient can supplement basic therapy:
- fresh potato juice;
- milk thistle seeds;
- dill infusion;
- mumiyo solution;
- propolis tincture with milk.
Alternative medicine offers a significant number of herbal combinations that help avoid the progression of pathology - token + chamomile + wormwood (in a ratio of 4: 3: 2), celery + corn silk + fertilization + anise + tricolor (1: 1). ratio). Water infusions are prepared from such herbal mixtures, which are recommended to be taken several times a day.
Symptoms of pancreatitis in men and women
From a physiological point of view, the pancreas is a very important organ of our body, responsible for normal digestion, as well as the production of the hormone insulin. A lack of the latter can cause diabetes.
In acute pancreatitis, the symptoms are similar to severe poisoning. This happens because during inflammation, enzymes are retained inside the pancreas, causing its subsequent destruction. Dead cells enter the blood in large quantities, which is manifested by symptoms of intoxication.
The most common signs of acute pancreatitis are described as follows:
- Intense constant cutting or dull pain that does not go away for a long time (up to painful shock). Pain is felt under the ribs on both sides (together or separately), sometimes pain is felt throughout the entire area of the abdomen and radiates to the lumbar region.
- A sharp decrease or increase in blood pressure.
- Changes in complexion: with pancreatitis in children and adults, the skin turns pale, gradually approaching grayish shades.
- Increase in body temperature to high levels.
- Nausea, hiccups, belching, and a feeling of dry mouth. Vomiting with secretion of bile.
- Diarrhea (diarrhea) with pancreatitis is a common phenomenon. Moreover, the feces come out with foam, with a sharp unpleasant odor, and undigested pieces of food are noticeable in it. There may also be constipation.
- Abdominal muscle tension.
- The appearance of shortness of breath, a characteristic icteric coating on the tongue, as well as sticky sweat: all this is the result of a lack of electrolytes due to vomiting and diarrhea.
- Bloating.
Preventive measures
To avoid increased blood pressure during pancreatitis, it is recommended:
- Compliance with a dietary diet (exclusion from the menu of high-calorie, spicy and salty foods).
- Regularly engage in accessible sports and breathing exercises.
- Stay in the fresh air every day (at least 1 hour a day).
For patients with symptoms of pathology, it is equally important to quit smoking and get enough sleep. Avoid stress, minimize the consumption of alcohol, strong tonic drinks - coffee and black tea.