Chronic gastroduodenitis is a combined inflammatory lesion of the mucous membrane of the pyloric stomach and duodenum. Symptoms of this disease include dyspepsia, bad breath, epigastric pain, and unstable stool. The diagnostic program usually includes EGDS, endoscopic biopsy with morphological examination of biopsy samples, EGG, antroduodenal manometry, intragastric pH-metry, and tests for Helicobacter. The treatment is long-term and consists of following a daily routine and diet, a special diet, correcting the acidity of gastric juice, and carrying out anti-Helicobacter and symptomatic therapy.
General information
Chronic gastroduodenitis is a common disease affecting both children and adults. The peculiarity of this disease is a combined lesion of the gastric mucosa and the initial parts of the small intestine (duodenum), therefore chronic gastroduodenitis is much more severe than isolated gastritis or duodenitis and is much less treatable.
The clinical picture of gastritis and gastroduodenitis is practically the same, which creates certain diagnostic difficulties for gastroenterologists. A characteristic feature of the pathology is that damage to the mucous membrane of the duodenum leads to disruption of the pancreas and hepatobiliary zone, as well as to autonomic disorders. Therapeutic tactics for gastroduodenitis imply the mandatory inclusion of B vitamins in the treatment regimen.
Chronic gastroduodenitis
Causes
All causes of chronic gastroduodenitis are divided into internal (endogenous) and external (exogenous).
1. Internal causes include gastrointestinal pathology (increased gastric acid production, decreased mucus production, disruption of reparative processes and hormonal regulation of digestion), as well as damage to the liver, pancreas and endocrine disorders. Secondary chronic gastroduodenitis develops against the background of:
- chronic gastritis;
- peptic ulcer of the stomach and duodenum;
- pancreatitis;
- hepatitis A;
- parasitic and allergic diseases;
- pathologies of the cardiovascular system;
- chronic renal failure.
2. External causes of chronic gastroduodenitis include eating too spicy, cold and hot foods, large amounts of food containing dyes, preservatives and pesticides, and indulging in alcohol, coffee and tea. In addition, infection with H. pylori is a factor in the development of this disease.
Chronic gastritis and gastrodoudenitis
Chronic gastritis is a common progressive disease, which is based on inflammation of the gastric mucosa with impaired ability of its cells to self-heal, with the progression of the inflammatory-degenerative process, leading to atrophy of the mucosa. As a result, the motor, secretory, and in some cases endocrine functions of the stomach are disrupted. Chronic duodenitis is accompanied by an inflammatory-dystrophic process in the duodenal mucosa and a violation of its functions. Duodenitis rarely occurs in isolation and is most often combined with chronic gastritis, peptic ulcer, enteritis and other diseases. Chronic gastroduodenitis is a disease that combines inflammation of the duodenal mucosa and the adjacent area of the stomach.
Main symptoms
In half of patients, chronic gastritis can go unnoticed for a long time or with very minor symptoms. Depending on which part of the stomach is affected by inflammation and the amount of hydrochloric acid produced, the disease can manifest itself in different ways.
In chronic gastritis with normal and increased secretion,
- epigastric pain on an empty stomach that goes away after eating;
- increased appetite;
- sour belching, nausea, vomiting, bringing relief;
- heartburn;
- tendency to constipation.
In chronic gastritis with decreased secretion, there may be
- dull aching pain in the epigastrium after eating;
- a feeling of bloating, fullness and heaviness in the epigastrium after eating;
- belching of air and food;
- fast saturation;
- decreased appetite;
- diarrhea, weight loss.
Causes of development of gastritis and duodenitis
An imbalance between the “aggression factors” and “protective factors” of the gastric and duodenal mucosa leads to the occurrence of gastritis and duodenitis.
External reasons include:
- violations of the qualitative and quantitative composition of food;
- chemical, mechanical and thermal influences;
- occupational hazards (vapors of acids, alkalis, cotton, coal, silicate dust, etc.);
- abuse of alcohol and its surrogates (cytotoxic effect);
- smoking;
- medicinal effects (non-steroidal anti-inflammatory drugs, potassium preparations, some antibiotics, etc.).
Internal reasons include:
- metabolic and endocrine disorders (diabetes mellitus, thyroid disease, etc.);
- diseases of the cardiovascular system, liver, biliary tract;
- anemia;
- allergic reactions and other diseases.
It has now been established that the microorganisms Helicobacter pylori play a major role in enhancing the aggressive properties of gastric contents and weakening the protective properties of the mucous membrane of the stomach and duodenum.
When to see a doctor
When there is pain, a burning sensation in the epigastrium and peri-umbilical region, early satiety, bloating, rumbling and other dyspeptic disorders. Also, consultation with a gastroenterologist will be necessary for prolonged anemia.
Complications
Chronic gastritis may precede or accompany serious diseases such as peptic ulcers and stomach cancer.
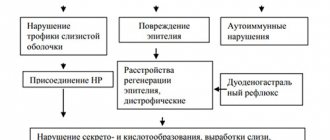
Pathogenesis
In the pathogenesis of chronic gastroduodenitis, the spread of the inflammatory process induced by Helicobacter pylori infection from the gastric mucosa to the duodenum is of leading importance. The combination of these etiological factors leads to increased secretion of hydrochloric acid in the stomach, disruption of the motor and evacuation functions of the digestive tube, and a decrease in the rate of formation of bicarbonates in the pancreas.
In chronic gastritis, metaplasia of the gastric mucosa occurs into the epithelium of the duodenum. Subsequently, these metaplastic islets are damaged by acidic gastric juice, which leads to the development of a pronounced inflammatory process.
The development of chronic gastroduodenitis in diseases of the cardiovascular system is caused by hypoxic damage to the wall of the duodenum. In chronic renal failure, a large amount of nitrogenous waste is released through the intestinal mucosa, which injures it.
Symptoms of chronic gastroduodenitis
The clinical picture of chronic gastroduodenitis is polymorphic, usually including discomfort in the epigastric region, a feeling of heaviness and fullness in the stomach. Often, spasmodic, bursting pain in the epigastric region occurs 1-1.5 hours after eating.
Dyspeptic symptoms are often disturbing: nausea, vomiting, heartburn, acid belching. The stool becomes unstable: diarrhea may alternate with constipation. A pathognomonic sign of chronic gastroduodenitis is the tongue being coated with a yellowish-brown coating, tooth marks on its lateral surfaces; bad breath. Autonomic disorders are typical: pallor, sweating, fatigue, irritability, sleep disturbances. When pressing on the epigastric area, patients report moderate pain.
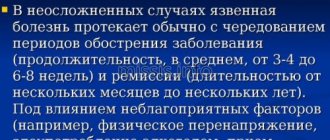
Chronic gastroduodenitis is characterized by alternating episodes of exacerbation (in the autumn-spring periods) and remission. The severity of the patient's condition during an exacerbation is usually determined by the severity and duration of pain, dyspeptic symptoms and other symptoms of the disease. The period of exacerbation can last up to two months, with complaints of pain persisting for about ten days, and pain on palpation for up to three weeks. Incomplete remission is characterized by the absence of complaints in the presence of an endoscopic and morphological picture of chronic gastroduodenitis.
Chronic gastroduodenitis: symptoms and treatment
11.10.2021
Gastroduodenitis is a simultaneous inflammation of the mucous membrane of the stomach and duodenum. This is one of the most common ailments of the gastrointestinal tract, second only to gastritis . Let's consider what is the etiology of the disease, what signs can be used to identify it, and what measures need to be taken to overcome this disease?
Causes of chronic gastroduodenitis
Regardless of the reasons that caused the development of the disease, it always entails inflammatory changes in the mucous membrane, dysfunction of the duodenum and stomach . As the disease progresses, under the influence of aggressive factors (bile acids, hydrochloric acid of gastric juice), ulceration occurs, as well as the formation of wounds on the walls of these organs - ulcers and erosions occur.
The main causes of chronic gastroduodenitis are divided into two groups: endogenous (directly related to functional disorders existing in the body) and exogenous (caused by external factors).
Endogenous factors:
- malfunctions of the immune system ;
- hormonal disorders;
- long-term stress and disturbances in the functioning of the nervous system ;
- genetic predisposition.
Exogenous factors:
- Infection, namely the bacterium Helicobacter pylori, which, during its life in the stomach , releases inflammatory factors of aggression and toxins;
- Improper diet, frequent overeating;
- Composition of food. Thus, smoked meats, fried foods, fatty, spicy foods provoke increased production of gastric juice, and the substances contained in these products lead to inflammation;
- Alcohol and smoking abuse.
Symptoms of chronic gastroduodenitis
The symptoms of chronic gastroduodenitis are extremely varied, they are constant and intensify during exacerbations. The most characteristic manifestation of the disease is aching pain localized in the epigastric region, occurring 2 hours after eating.
Painful sensations are accompanied by nausea , a feeling of fullness and heaviness in the epigastric region, heartburn , and belching . A dense yellowish coating appears on the tongue, it is very swollen, which is confirmed by the imprints of teeth left on its lateral surfaces.
intestinal excretory function , and therefore the patient may experience constipation, diarrhea, or even an alternation of these phenomena. Patients diagnosed with chronic gastroduodenitis are irritable, pale, they often have sleep disturbances, there is weight loss, and fatigue appears.
Treatment of chronic gastroduodenitis
With gastroduodenitis, the duodenum and stomach are in a pre-ulcerative state. This is why it is very important to seek medical help immediately.
In the treatment of chronic gastroduodenitis, great importance is given to diet . The patient's diet should consist of fish, meat and mushroom soups, dairy products, eggs, lean meat, a variety of cereals, fruits and vegetables.
It is very important that the meals are fractional, i.e. the patient should eat food up to 5-6 times a day, but do it in small portions. It is not recommended to eat too hot or cold foods.
If a Helicobacter pylori infection is detected, treatment of chronic gastroduodenitis is based on a course of therapy , the duration of which varies from 7 to 12 days. As a rule, the course consists of taking antibiotics, namely: macrolides, metronidazole and amoxicillin.
If there is increased acidity in the stomach , the specialist will prescribe antisecretory drugs and omeprozole. These products are designed to inhibit the uncontrolled release of acid over a long period of time.
Treatment of chronic gastroduodenitis can last up to 2 years, and therefore the patient will have to prepare himself for a long and persistent struggle.
Published in Gastroentorology Premium Clinic
Diagnostics
To make the correct diagnosis, all patients with suspected chronic gastroduodenitis are consulted with a gastroenterologist and an endoscopist. Hospitalization to the gastroenterology department is usually required only for patients with severe disease. Brief hospitalization may be necessary for examination. Patients undergo:
- Endoscopy of the stomach. During esophagogastroduodenoscopy, both hyperemia and hypertrophy of the mucosa (focal or diffuse), as well as its atrophy, thinning and pallor, can be visualized as the process transitions to the atrophic stage. In order to reliably assess the condition of the mucous membrane of the stomach and duodenum, the severity of the inflammatory process, endoscopic biopsy and morphological examination of biopsy specimens are performed.
- Intragastric pH-metry. Required to assess acidity in the antrum of the stomach, as well as to predict acidity in the duodenum. The difference between the pH of the body of the stomach and its antrum should be at least 2. If this indicator decreases, this may indicate inhibition of the neutralization function of the antrum and the entry of too acidic gastric contents into the duodenum, damaging its mucosa. The criterion for low acidity is a decrease in all indicators, both basal secretion and during its stimulation. Increased acidity is indicated by an increase in at least one indicator.
- Functional studies. To assess the motor-evacuation function of the stomach and duodenum, electrogastrography and antroduodenal manometry are performed.
- Radiation diagnostics. An auxiliary diagnostic method is ultrasound examination of the stomach filled with fluid. For the same purpose, as well as for differentiation from other diseases, barium radiography of the stomach is used.
- Laboratory research. In order to clarify the etiology of chronic gastroduodenitis, Helicobacter in feces is determined by ELISA and PCR, antibodies to H. pylori in the blood, and a breath test. The most reliable method for diagnosing Helicobacter pylori infection is histological.
Differential diagnosis
Chronic gastroduodenitis should be differentiated from functional diseases (stomach dyskinesia, intestinal dyskinesia, dyspepsia, duodeno-gastric reflux, functional stomach disorders), isolated inflammatory process in the stomach or duodenum (gastric ulcer, peptic ulcer of the 12th intestine, bulbitis, chronic gastritis, chronic duodenitis) or vice versa, more common (gastroenteritis, enterocolitis).
Chronic gastroduodenitis and peptic ulcer in children
A
The relevance of the problem of chronic gastroduodenitis and peptic ulcer disease is due to the significant prevalence of diseases of the digestive organs in children, among which gastroduodenal pathology occupies a leading place.
An analysis of the prevalence of diseases of the digestive system in children in the Russian Federation shows that over the past 20 years there has been a significant increase in gastroenterological pathology in children and an uncontrolled increase in the incidence of diseases of the stomach and duodenum. Thus, according to epidemiological studies conducted in the Nizhny Novgorod region in the 70s [1], the prevalence of non-infectious gastroenterological diseases in preschool and school-age children was 61.8 and 81.5%, respectively. Similar studies in the 90s [2] revealed an increase in these indicators - 398.1 and 365.2%o, respectively. Study of morbidity in the regions of the Russian Federation for 1996-1997. showed that the data on appealability and special epidemiological studies differ significantly: in Bashkortostan, 191.9 and 428.0%o, respectively. Leningrad region - 101.9 and 487.7%o, Kursk region - 152.7 and 467.7%o. Very low rates of gastroenterological morbidity in children (less than 50%) were noted in Kaliningrad, Oryol, Volgograd, Amur and other regions, which does not reflect the true prevalence of diseases of the digestive system in children in these regions. The above is directly related to the problem of chronic gastroduodenitis and peptic ulcers in children and indicates their untimely diagnosis, since it has been established that in the structure of the pathology of the digestive system, diseases of the stomach and duodenum account for 50-60% [1-3]. Table 1. Neck diagram
| Factors of aggression | Protective factors |
| Overproduction of HCL | Mucosal barrier: |
| - vagotonia - increased excitability of parietal cells | - mucin, sialic acids; — bicarbonates — reverse diffusion of H+ ions |
| Regeneration | |
| Impaired blood supply to the mucous membrane | Sufficient blood supply |
| Antroduodenal acid thromosis disorder | Antroduodenitis acid brake |
| Bile acid and lysolecithin |
Late diagnosis of chronic gastroduodenitis and peptic ulcer disease in children (63%) is largely explained by the uninformative onset of the disease, the frequent involvement of other organs of the digestive system in the pathological process, insufficient familiarity of doctors with the clinical manifestations of the disease and the complexity of instrumental examination of the child. Table 2. Classification of gastritis and gastroduodenitis in children
| Etiology | Localization | Course of the disease | Phase (stage) | Functional diseases stomach condition |
| Primary (exogenous) gastritis, gastroduodenitis | Focal gastritis: fundal antral | Latent | Exacerbation Incomplete clinical remission | Gastric acidity and motility: increased; demoted; fine |
| Secondary (endogenous) gastritis, gastroduodenitis | Common gastritis Gastroduodenitis | Monotonous Recurrent | Clinical remission Clinical endoscopic remission |
Chronic diseases of the stomach and duodenum often begin in preschool and school age; the recurrent course of the disease leads to pronounced anatomical changes in the organ and subsequently to loss of ability to work and disability of the adult population. Observations in a pediatric gastroenterology clinic indicate that over the past 10 years, an increase in the frequency of severe forms of gastritis and gastroduodenitis has been recorded in children, leading to the development of peptic ulcers [4], multiple erosions [5, 6] and subatrophy, atrophy of the gastroduodenal mucosa [4, 7 ]. Table 3. Morphological characteristics of the mucous membrane of the stomach and duodenum
| Endoscopic | Histological |
| Superficial gastritis (gastroduodenitis) | Superficial gastritis (gastroduodenitis) |
| "Hypertrophic gastritis" (gastroduodenitis) | Diffuse gastritis (gastroduodenitis) |
| Erosive gastritis (gastroduodenitis) | without gland atrophy |
| Hemorrhagic gastritis (gastroduodenitis) | with gland atrophy |
| Subatrophic (atrophic) gastritis (gastroduodenitis) | giant hypertrophic |
| Mixed gastritis (gastroduodenitis) | (Menetrier's disease) |
Peptic ulcer disease in children at the present stage is also characterized by an unfavorable course with the formation of multiple and chronic ulcers [8, 9], which are not amenable to conservative therapy and require surgical intervention [10]. Chronic gastroduodenitis and peptic ulcer are multifactorial and heterogeneous diseases caused by disruption of the body's main regulatory systems (nervous, endocrine and immune), an imbalance between local factors of "aggression" and "defense", impaired regeneration and damage to the gastroduodenal mucosa. Ultimately, the nosological form of gastroduodenal pathology is determined by impaired regeneration and the characteristics of morphofunctional disorders of the mucous membrane. Table 4. Classification of peptic ulcer
| Stage | Endoscopic characteristics of the stages of the disease | Phase | Localization | Form | Flow | Functional characteristics |
| 1 | "Fresh Ulcer" | Exacerbation Incomplete clinical remission Clinical remission Clinical endoscopic remission | In the stomach: Subcardinal section lesser curvature prepyloric sections In the duodenum: bulb postbulbar section Dual localization | Uncomplicated Complicated: Bleeding, penetration, perforation, pyloric stenosis, perivisceritis | Newly diagnosed ulcer and motility: recurrent Rarely (remissions for more than 3 years) Often recurrent (remissions less than 3 years) Continuously recurrent (remissions less than 1 year) | Acidity of gastric contents increased decreased normal |
| 2 | Beginning of epithelization of ulcerative defect | |||||
| 3 | Scarring ulcer with preserved duodenitis | |||||
| 4 | Complete healing (scar deformity) |
Chronic gastroduodenitis is characterized by an inflammatory process, subatrophic, atrophic and (or) erosive changes in the gastroduodenal mucosa. Peptic ulcer disease is a chronic disease in which ulcers form in the stomach or duodenum and which can progress and lead to the development of complications.
Etiology and pathogenesis
Chronic gastroduodenitis and peptic ulcer disease often develop in children who have a hereditary predisposition to the disease and whose compensatory and adaptive capabilities of the body are reduced due to previous somatic and infectious diseases. Research by A.A. Baranova and O.V. Grinina [3] showed that in children born to mothers with pathological pregnancy and during pathological childbirth, who were bottle-fed and have a burdened allergic history, the risk of developing diseases of the digestive system increases significantly. One of the decisive factors in the occurrence of chronic gastroduodenitis and peptic ulcer disease is hereditary-constitutional
.
Hereditary predisposition is more pronounced and more often occurs in patients with peptic ulcer disease, while it is registered in 20-60% of children and is observed more often on the paternal side. Along with a thorough history taking and identifying the disease in the child’s relatives, it is necessary to determine genetic markers of predisposition to peptic ulcer disease, such as the absence of the third fraction of alkaline phosphatase, high levels of acetylcholine and cholinesterase in the blood serum, hyperproduction of hydrochloric acid due to an increase in the number of parietal cells, increased levels of pepsinogen I deficiency of mucopolyproteins, etc. The implementation of a hereditary predisposition may be due to a lack of sialic and sulfated mucins, which provide protection to the mucous membrane, and overproduction of G-cells in the gastroduodenal mucosa, accompanied by continuous acid and enzyme formation [11]. The causes of chronic diseases of the stomach and duodenum can be divided into exogenous, endogenous and infectious. Exogenous factors include: food poisoning and past intestinal infections, long-term violations of the regime and quality of nutrition (rare or frequent meals, uneven intervals between them), consumption of foods that mechanically and chemically irritate the gastroduodenal mucosa, dry food, poor chewing of food.
Important importance is attached to the lack of substances in food necessary for physiological regeneration and restoration of the “glandular apparatus” of the mucous membrane - iron, vitamins, microelements, protein.
It should be taken into account that long-term or indiscriminate use of medications (salicylates, aspirin, sulfonamide drugs, antibiotics, etc.) leads to pronounced structural changes in the gastroduodenal mucosa. Neuropsychic overload causes disturbances in the mechanisms of intersystem relations in the body of children and the development of the disease. Among endogenous factors, the greatest importance is attached to the neuro-reflex effects on the stomach and duodenum from other affected digestive organs, the gallbladder and liver, pancreas, and intestines.
The pathological influence is realized through the nervous and endocrine systems (according to the feedback principle), reflexively, causing dysregulation of the gastroduodenal system, an imbalance of neuropeptides of the APUD system and discoordination of the secretory and motor functions of the stomach and duodenum.
The resulting imbalance of the factors of “aggression” and “defense” in the gastroduodenal system leads to the development of a nonspecific inflammatory process, impaired regeneration of the mucous membrane and the appearance of dystrophic, erosive and ulcerative changes. The cause of damage to the mucous membrane of the stomach and duodenum is diseases of the cardiovascular system, kidneys, blood diseases that occur with anemia, diseases of the endocrine system (diabetes mellitus, adrenal insufficiency, etc.). Pediatricians pay insufficient attention to the timely and complete treatment of chronic foci of infection, helminthic infestation, giardiasis and intestinal dysbiosis. After the discovery of the microorganism Helicobacter pylori (HP) in the mucous membrane of patients with chronic gastritis by B. Marshall and J. Warren (1983), a new stage began in the development of ideas about the etiology and pathogenesis and methods of treatment of diseases of the stomach and duodenum. However, to date, the role and significance of HP in the development of this pathology has not been fully elucidated. The concept of the leading, dominant role of HP in the development of lesions of the mucous membrane of the stomach and duodenum I.L. Blinkov [12] considers it one of the persistent medical myths. The author emphasizes the saprophytic role of the microorganism, pointing out the harm of the HP concept. At the same time, the leading role of HP in the etiology and pathogenesis of diseases of the stomach and duodenum is emphasized in a number of works [13-15], while the authors consider, in particular, “duodenal ulcer” as a manifestation of an infectious disease. Numerous works by both therapists and pediatricians provide conflicting data on the role of HP in the development of gastroduodenitis and peptic ulcers, and on the results of treatment including antibacterial drugs. This is understandable, since currently studies of the microorganism have revealed the existence of more than 40 epidemiologically unrelated strains of HP, with different pathogenicity and sensitivity to antibacterial agents. In addition, the authors use different methods for detecting HP and treating it. It has now been established that contamination of the gastric mucosa with HP contributes to the development of chronic gastroduodenitis and peptic ulcer disease.
Helicobacter infection and its role in the formation of gastroduodenal pathology in children are of interest to many researchers. This is due to the fact that many mechanisms of gastritis and ulcerogenesis and their connection with HP infection have not yet been clarified and clarified [7, 16]. Over the course of many decades, with the discovery of new factors and the discovery of patterns in the pathogenesis of diseases of the stomach and duodenum, new hypotheses and theories arose that are now well known: corticovisceral, neuroendocrine, inflammatory, reflux, infectious, etc. However, none of these theories cannot fully explain the etiology and pathogenesis of chronic diseases of the stomach and duodenum. The peculiarity of the modern period is the intensification of the damaging effects of environmental agents on the body (psychological stress, environmental distress, etc.), disruption of the reaction of defense systems and a decrease in the child’s body’s resistance to health risk factors. Many scientists [16-18] consider the disease as a breakdown of the body’s compensatory-adaptive mechanisms during antigenic overload and from the position of disruption of the biological rhythm of various physiological processes in the body. Currently, there is no unified theory of the pathogenesis of chronic gastroduodenitis and peptic ulcer disease.
| The main links of pathogenesis can be grouped as follows: • disorder of the nervous and hormonal mechanisms regulating the activity of the stomach and duodenum; • local imbalance of aggression and defense factors in the gastroduodenal system; • imbalance of neuropeptides in the APUD system; • impaired regeneration of the gastroduodenal mucosa. |
It should be emphasized that it is conventional to distinguish these links of pathogenesis, since in a child’s body all systems that ensure the implementation of compensatory and adaptive mechanisms are interconnected and interdependent. The leading importance in the development of chronic gastroduodenitis and peptic ulcer disease is given to a violation of the ratio of aggression factors (strengthening) and protective factors (weakening) of the gastroduodenal mucosa (Table 1). Factors of aggression include hyperproduction of hydrochloric acid and enzymes due to increased tone of the parasympathetic nervous system, increased excitability of parietal and main cells.
An increased concentration of hydrogen ions (H+) and their reverse diffusion lead to disruption of the blood supply to the mucous membrane, the occurrence of stasis and hemorrhage.
At the same time, the penetration of active hydrogen ions through a broken mucous barrier causes an imbalance of neuropeptides of the APUD system with the activation of gastrin, histamine and a further increase in the aggressiveness of gastric juice. One of the important factors in the development of the pathological process is a violation of the “antroduodenal acid brake,” leading to significant acidification of the duodenum and the occurrence of reflux of its contents into the stomach. The entry of bile, pancreatic enzymes, and lysolycetin into the lumen of the stomach significantly increases the aggressiveness of gastric juice and activates the gastrin-histamine system. Long-term exposure to aggressive gastric juice on the gastroduodenal mucosa leads to impaired regeneration and disregenerative processes, causing different types of damage to the mucous membrane of the stomach and duodenum (erosions, ulcers, atrophy, metaplasia, etc.). Protective factors include the mucous barrier of the gastroduodenal mucosa and the secretion of mucoproteins that protect the mucosa from antigens.
Preservation of the mucous membrane from damage is also ensured by sufficient blood circulation, preservation of the “antroduodenal acid brake” and physiological regeneration of the mucosa. Local immunological protection is primarily secretory immunoglobulin class A (s IgA), specifically binding protein antigens, lysosomal proteolytic enzymes of enterocytes, and mediator immunity. A nonspecific protective factor is lysozyme, which is resistant to the action of proteolytic enzymes. By enveloping food, lysozyme of digestive secretions protects the mucous membranes from antigenic irritants. It is necessary to highlight the features of the pathogenesis of chronic gastroduodenitis and peptic ulcers associated with HP. Virulent HP strains have the property of damaging the epithelium of the gastric mucosa; Due to the liposaccharide of the outer membrane of the HP and thanks to the flagella, they penetrate the layer of the mucous membrane. Violation of the integrity of the mucous membrane causes reverse diffusion of H+ ions, which leads to the development of inflammation, the appearance of defects on the surface of the epithelium, damage to the vascular epithelium, impaired microcirculation and ulcerations. The urease enzyme produced by HP activates monocytes and leukocytes, which leads to the release of cytokines and the production of free radicals that damage the epithelium. The high proteolytic activity of HP waste products is a factor of aggression. The etiological factors and links in the pathogenesis of chronic gastroduodenitis and peptic ulcer disease presented above must be taken into account by the pediatrician, since identifying the significant causes of the disease and the mechanisms of development of the pathological process, taking into account the individual characteristics of the violation of the regulatory systems of the child’s body, allows for effective therapy.
Clinical manifestations
Clinical manifestations of chronic gastroduodenitis and peptic ulcer disease are varied and depend on the degree of structural changes in the mucous membrane, their localization, the stage of the pathological process, the functional state of the stomach and metabolic disorders in the body. Common signs of the disease are weakness, lethargy, disturbed sleep, and often headaches. The child is irritable and whiny. Objectively: pale skin, manifestations of vitamin deficiency. Muscle tone may be reduced. The severity of these symptoms depends on the degree of metabolic disorder in the body.
Gastroduodenitis
In practical gastroenterology, the classification of chronic gastroduodenitis (Table 2), proposed by a group of leading pediatric clinics, is still used [5]. Undoubtedly, the proposed classification requires revision and discussion, but most practitioners note its simplicity and convenience for identifying the nosological form. The pediatric literature presents numerous, often contradictory descriptions of the clinical manifestations of individual nosological forms, therefore it is advisable to group clinical symptom complexes, manifestations of exacerbation of the disease, taking into account the topographic parts of the stomach and duodenum, depending on the severity and nature of the lesion of the gastroduodenal mucosa (Table 3) and secretory -motor disorders of the stomach and duodenum. It is advisable to distinguish three variants of clinical manifestations of chronic gastroduodenitis.
1. In most children with chronic gastroduodenitis with exogenous factors,
more pronounced changes are determined in the mucous membrane of the antrum of the stomach and duodenum
in the form of inflammation, subatrophy and (or) hyperplasia of the mucosa, erosive lesions.
Nosologically they can be defined as gastroduodenitis, antral gastritis, duodenitis, erosive antral gastritis or duodenitis. A feature of this variant of the course of the disease is preserved or increased function of acid and enzyme formation, discoordination of the secretory and motor functions of the stomach and duodenum. Patients experience irritability and headaches. Appetite is often preserved. Dyspeptic disorders (heartburn, sour belching) are usually associated with cardiac insufficiency of the esophagus. Sometimes children experience increased thirst. The tongue is often covered with a white coating. Abdominal pain is intense, localized in the epigastrium and pyroduodenal zone, and occurs not only after eating, but also on an empty stomach. Often the pain stops after eating. Patients in this group are prone to constipation. 2. With a long duration of the disease and the predominance of endogenous, toxic risk factors, the fundus of the stomach is involved in the pathological process
, and along with inflammatory, atrophic, subatrophic changes, focal atrophy, multiple erosions of the middle third of the gastric mucosa are often determined.
The nosological form in this group of children may be fundal gastritis, gastroduodenitis with damage to the glandular apparatus of the stomach, and erosive changes. Features of this variant of the disease are a decrease in acid and enzyme formation, and atony of the digestive organ. Patients experience weakness, lethargy, fatigue, dyspeptic symptoms - a feeling of heaviness, fullness in the epigastrium after eating, nausea, and sometimes belching air. Abdominal pain is low-intensity, dull, and occurs after eating. In children, flatulence and loose stools are recorded. Palpation determines pain in the upper and middle third of the space between the xiphoid process and the navel. 3. The presence in a child of hereditarily determined morphofunctional changes in the mucous membrane of the stomach and duodenum, which can transform into a peptic ulcer
, is considered a pre-ulcerative condition. In children, hyperplasia of the fundic glands of the gastric mucosa is determined with an increase in the number of main parietal cells [11]. The nosological form can be defined as gastritis, gastroduodenitis, duodenitis with high continuous acid and enzyme formation and pronounced inflammatory, hyperplastic, erosive changes in the mucous membrane of the stomach and duodenum. Clinical manifestations are similar to those of duodenal ulcer. The leading symptom is fasting pain: before meals and 2-3 hours after meals. The pain is intense, paroxysmal, stabbing, cutting, localized in the pyloroduodenal zone, left hypochondrium. Sour belching is characteristic. Seasonality of the pain syndrome (spring, autumn) is observed in 1/3 - 1/2 of patients. The stool in these patients tends to become hard or constipated. Palpation of the abdomen clearly reveals pain in the pyloroduodenal zone, Mendel's sign is positive (pain on percussion).
Peptic ulcer
When considering the clinical manifestations of peptic ulcer disease, it is necessary to emphasize the “rejuvenation” of the disease; Currently, peptic ulcer disease can be diagnosed in children from 5-6 years of age. Ulcerative lesions are mainly (85%) localized on the anterior or posterior wall of the duodenal bulb; 15% of patients have postbulbar (extra-bulb) ulcers. Duodenal ulcer occurs 6-7 times more often than gastric ulcer. In table Figure 4 presents the working classification of peptic ulcer disease in children, widely used in clinical practice. In children, the manifestations of peptic ulcer disease are varied and depend on the stage and location of the defect. Duodenal ulcers are characterized by hunger pain (on an empty stomach or 1.5-2 hours after eating). The vast majority of children experience night pain. The pain is paroxysmal in nature, cutting, stabbing, radiating to the back, right shoulder, and shoulder blade. The localization of pain is determined by the location of the ulcer: pain most often occurs in the epigastric region and to the right of the midline. Palpation of the abdomen is difficult, pain is noted in the pyloroduodenal area. Vomiting in patients occurs more often at the height of the pain syndrome. Dyspeptic manifestations (heartburn, sour belching) with peptic ulcer disease indicate cardia insufficiency. Children's appetite is most often preserved, sometimes even increased. The tongue is covered with a white coating and is moist. Constipation is typical for patients with exacerbation of the disease. Seasonality of pain and dipeptic syndromes is noted (spring, autumn). Extrabulb, or postbulbar, ulcers are characterized by a more severe and complicated course of the disease. The pain is persistent, especially severe at night (children wake up from it). The clinical characteristics of a gastric ulcer have a number of features and are determined by the localization of the ulcer (in the cardiac or antrum of the stomach). When the ulcer is localized in the cardiac part of the stomach, early abdominal pain is characteristic, occurring immediately after eating. The pain syndrome is accompanied by nausea and belching of air. The pain is localized under the xiphoid process. Ulcers in the antrum of the stomach are accompanied by attacks of severe abdominal pain, not associated with food intake, radiating to the back, behind the sternum. The seasonality of exacerbation of the disease is less typical than with duodenal ulcer. Complications of peptic ulcer:
• bleeding accompanied by vomiting mixed with blood, melena, weakness, dizziness; one of the first signs is tachycardia; • penetration, characterized by persistent pain, sharp pain radiating to the back, vomiting that does not bring relief, and persistent heartburn; • perforation, which occurs acutely and is accompanied by sharp pain in the epigastric region, tension in the anterior abdominal wall and symptoms of peritoneal irritation. Peristalsis is weakened or absent. In view of the high infection rate of the child population with HP, reaching 58-72% by the age of 13-15 years of life [12], as well as taking into account the etiopathogenetic mechanisms of diseases associated with HP described above, an important question for practical healthcare arises - what are the clinical and morphofunctional features of chronic gastroduodenitis and peptic ulcer disease associated with HP. Unfortunately, we have to admit that most of the authors who devoted their work to this problem in pediatrics [18-20] did not identify specific symptoms of gastroduodenal pathology associated with HP. Only in some studies [7, 21] HP infection is associated with more frequent recurrent abdominal pain, vomiting and hemorrhagic syndrome (nosebleeds, bleeding gums, hemorrhages in the gastric mucosa). Changes in the gastric mucosa noted during endoscopy in the form of “cobblestone pavement” and “nodular gastritis” [15] can hardly be attributed to markers of infection of the gastric mucosa with HP.
Diagnostics
Observations in the gastroenterology clinic indicate that a thorough study of the anamnesis, analysis of risk factors, assessment of the clinical manifestations of the disease, examination of the child and palpation examination of the abdominal organs allow timely recognition of diseases of the stomach and duodenum in 70-80% of cases. Difficulties in diagnosis in the early stages of disease development are often associated with the involvement of other digestive organs (pancreas, hepatobiliary system, intestines) in the pathological process, which causes the “blurred” clinical manifestations of chronic gastroduodenitis and peptic ulcers in children. Additional methods for examining the stomach and duodenum can be divided into three groups. 1. Methods based on the study of the morphological characteristics of the stomach and duodenum (x-ray studies, gastroduodenofibroscopy, histological, histochemical study of biopsy samples of the gastroduodenal mucosa). 2. Methods for studying the functional state of the gastroduodenal system (fractional gastric intubation, pH-metry, radiotelemetry, electrochastography, manometry, etc.). 3. Methods for detecting HP.
The experience of using modern instrumental diagnostic methods for chronic gastroduodenitis and peptic ulcer disease with the definition of indications, preparation and technique for conducting research, and evaluation of the results obtained is summarized by the country's leading scientists working in the field of pediatric gastroenterology in the “Handbook of Pediatric Gastroenterology” [9] and in the monograph “ Diseases of the digestive system in children" (M., 1996) edited by academician.
RAMS A.A. Baranova. X-ray signs
of chronic gastroduodenitis are changes in the relief of the mucous membrane, mainly in the pyloric antrum of the stomach and (or) in the duodenum (folds are rearranged, thickened, swollen or smoothed).
These changes are accompanied by disturbances in the secretory and motor functions of the stomach, antiperistalsis, and the presence of reflux. Peptic ulcer disease is characterized by direct and indirect signs. Direct symptoms include a “niche” with an inflammatory shaft, convergence of folds, and cicatricial deformation. It should be emphasized that the absence of the “niche” symptom does not exclude the presence of a peptic ulcer if the patient has persistent local swelling of the mucous membrane in combination with palpation pain in this area. In medical practice, endoscopic
research methods are widely used to more accurately identify pathological changes in various topographic zones of the gastroduodenal mucosa.
The inflammatory process is characterized by hyperemic, juicy, loose and very vulnerable mucosa, hemorrhages, often the relief of the mucosa resembles the appearance of a cobblestone street. With subatrophy (atrophy) of the mucosa, the relief is smoothed and depleted areas of a dull grayish-white color with an enhanced vascular pattern are visible. The erosive form of gastroduodenitis is determined by multiple flat or cone-shaped erosions with a diameter of 0.3-0.5 mm with a bottom covered with a gray coating. Peptic ulcer disease is characterized by round or oval defects with smooth, clear edges ranging in size from 5 to 10-15 mm. The bottom of the defect is made of a dense lesion of gray-gray fibrin. Histological and histochemical study of biopsy samples
of the mucous membrane from various parts allows not only to determine the depth and nature of the damage to the membrane in various topographic zones, but also to clarify the degree of activity of the process and the presence of HP.
The assessment of mucosal biopsy should be carried out taking into account the Sydney classification (1990) using a visual analogue analysis scheme according to M. Dixou et al. (1996). Among the methods for studying the functional state of the gastroduodenal system in pediatric practice, the leading one is still the study of the acid-forming function
of the stomach by titrating the stomach contents obtained using a probe before and after the introduction of an irritant and intragastric pH-metry. In clinical practice, when assessing the results of studying gastric secretions using fractional sounding, special attention must be paid to two variants of the results obtained. If high levels of acid and enzyme formation are detected in fasting and basal portions, you must first
Treatment of chronic gastroduodenitis
Diet therapy
Treatment of chronic gastroduodenitis is usually long-term and includes several stages, sequentially following each other. Treatment begins with the appointment of a special diet. Meals include pureed porridge in meat, vegetable or mushroom broth; lean meats and fish; vegetables and fruits, dairy products; bakery products (excluding baked goods).
Food preparation can be varied (steamed, boiled, stewed, baked); Freshly squeezed juices are allowed. Even milk is allowed if it does not have a laxative effect. The diet must include foods rich in vitamins B1, B2, PP, C. There should be at least five meals per day. Food should be eaten warm, chewed thoroughly, and in small portions.
In the acute period, bed rest is required for at least seven to eight days. If you adhere to a diet, this allows you to reduce the intensity of the inflammatory process and pain.
Pharmacotherapy
Considering the high frequency of detection of Helicobacter pylori infection in chronic gastroduodenitis, eradication of the pathogen is carried out according to a certain scheme, which is selected based on the severity of the disease:
- bismuth preparation, metronidazole and tetracycline antibiotic for one to two weeks
- Metronidazole, clarithromycin, omeprazole for a week
- Ranitidine, amoxicillin, metronidazole for 10-14 days
To prescribe or correct the most effective treatment regimen, a second consultation with a gastroenterologist may be required. For increased acidity, H2-histamine receptor blockers (cimetidine, ranitidine, famotidine), proton pump inhibitors (omeprazole, lansoprazole, pantoprazole, rabeprazole, esomeprazole), antacids (aluminum hydroxide, magnesium hydroxide, aluminum phosphate, magnesium carbonate), gastroprotectors (bismuth) are used , sucralfate). Complex treatment necessarily includes prokinetics and enzymes.
Non-drug therapy
Of great importance in the treatment of chronic gastroduodenitis is sanatorium-resort and balneological treatment, physiotherapeutic measures, moderate physical activity and physical therapy. Herbal medicine is also widely used (decoctions of chamomile, string, plantain, mint, yarrow, St. John's wort, valerian).
Chronic gastroduodenitis
Diet therapy
Treatment of chronic gastroduodenitis is usually long-term and includes several stages, sequentially following each other.
Treatment begins with the appointment of a special diet. Meals include pureed porridge in meat, vegetable or mushroom broth; lean meats and fish; vegetables and fruits, dairy products; bakery products (excluding baked goods). Food preparation can be varied (steamed, boiled, stewed, baked); Freshly squeezed juices are allowed. Even milk is allowed if it does not have a laxative effect. The diet must include foods rich in vitamins B1, B2, PP, C. There should be at least five meals per day. Food should be eaten warm, chewed thoroughly, and in small portions.
In the acute period, bed rest is required for at least seven to eight days. If you adhere to a diet, this allows you to reduce the intensity of the inflammatory process and pain.
Pharmacotherapy
Considering the high frequency of detection of Helicobacter pylori infection in chronic gastroduodenitis, eradication of the pathogen is carried out according to a certain scheme, which is selected based on the severity of the disease:
- bismuth preparation, metronidazole and tetracycline antibiotic for one to two weeks
- Metronidazole, clarithromycin, omeprazole for a week
- Ranitidine, amoxicillin, metronidazole for 10-14 days
To prescribe or correct the most effective treatment regimen, a second consultation with a gastroenterologist may be required. For increased acidity, H2-histamine receptor blockers (cimetidine, ranitidine, famotidine), proton pump inhibitors (omeprazole, lansoprazole, pantoprazole, rabeprazole, esomeprazole), antacids (aluminum hydroxide, magnesium hydroxide, aluminum phosphate, magnesium carbonate), gastroprotectors (bismuth) are used , sucralfate). Complex treatment necessarily includes prokinetics and enzymes.
Non-drug therapy
Of great importance in the treatment of chronic gastroduodenitis is sanatorium-resort and balneological treatment, physiotherapeutic measures, moderate physical activity and physical therapy. Herbal medicine is also widely used (decoctions of chamomile, string, plantain, mint, yarrow, St. John's wort, valerian).
Prognosis and prevention
Prevention of chronic gastroduodenitis includes maintaining a healthy lifestyle and diet, and physical activity. It is necessary to avoid stress and devote enough time to rest and sleep. It should be remembered that timely treatment of chronic gastroduodenitis is an excellent prevention of gastric and duodenal ulcers. Secondary prevention of chronic gastroduodenitis is aimed at preventing the recurrent course of the disease. Anti-relapse treatment is carried out in two-month courses during periods of probable exacerbations (autumn and spring). Diet No. 5 is prescribed. Treatment with mineral waters, physiotherapy, physical therapy is advisable.
If chronic gastroduodenitis is treated irregularly and not fully, the disease becomes severe, significantly worsening the quality of life and negatively affecting the patient’s ability to work.