The digestive tract is long. It includes the esophagus, stomach, intestines, and endocrine sections. Therefore, when complaining of abdominal pain, it is quite difficult to detect the root cause of the symptom.
When the patient arrives for an appointment, the doctor asks him about the nature, strength, and location of painful sensations. This is required in order to suspect a lesion. Next, laboratory and instrumental tests are prescribed to establish the exact location of the damage.
The table shows different types of pain and the reasons for their formation.
| Nature of pain | Type and diseases |
| Long lasting cutting sensation | Inflammation of the duodenum, tumors, uterine endometritis |
| Sudden spasms | Duodenal and gastric ulcers, vascular aneurysms, urolithiasis |
| Maintaining constant intensity | Intestinal obstruction, thrombus formation in large vessels of the abdominal cavity |
| Gradually increasing | Inflammation of the appendix, pancreas, gall bladder |
| Similar to colic, developing over a long period of time | Intestinal obstruction, increased gas formation, pancreatitis |
Ulcerative colitis
With pathology, chronic intestinal damage occurs. The inflammatory process damages the deep walls. Periodic exacerbations and relapses occur. The mucous membrane undergoes the following deformations:
- ulcer formation;
- necrotic areas.
When the disease occurs, the left lower abdomen is damaged. The patient gradually develops the following negative symptoms:
- pain syndrome, which becomes more intense over time;
- pain concentrated in the left area;
- diarrhea with inclusions of mucus and blood;
- periodic spasms like bowel movements;
- increased body temperature up to 39 degrees, chills, fever;
- appetite suppression;
- dehydration due to fluid loss due to diarrhea;
- intoxication of the body, accompanied by arthralgia and myalgia;
- malaise, chronic fatigue, loss of strength.
If ulcerative colitis is left untreated for a long time, areas of ulcers and necrosis form on the intestinal wall. A perforation is formed, due to which feces penetrate into the abdominal cavity, which provokes peritonitis.
The pathology is difficult to treat; it is important to obtain a period of remission. The following groups of drugs are used:
- anti-inflammatory drugs, aminosalicylates - Mesalamine, Colazal;
- chemotherapy for the autoimmune nature of the pathology - Azathioprine, Methotrexate;
- steroids to eliminate inflammation - Metronidazole, Prednisolone.
If intestinal damage is present, it is important to continue the diet. If the patient violates it, the risk of relapse is high. When consuming low-quality products, intestinal injuries and increased inflammation can occur. All food is divided into 6 servings to prevent overload of the digestive tract and normalize peristalsis.
Treatment
Help before diagnosis
For colic in the side that occurs during training, no treatment is required. It is recommended to temporarily limit physical activity until the discomfort disappears. To get rid of left-sided pain caused by constipation, you need to add fresh or baked vegetables and fruits, fermented milk products, and black bread to your diet. These products stimulate intestinal motility.
To reduce pain caused by emotional turmoil (for example, with IBS), it is important to minimize stressful situations and, if necessary, visit a psychologist. Severe pain in the left side indicates severe gastroenterological or gynecological diseases, so self-medication in this case is unacceptable. The combination of a painful attack with a sharp deterioration in condition is an indication for emergency medical care.
Conservative therapy
Treatment is selected after determining the cause of pain in the side. In case of severe pain, pain relief comes to the fore - non-narcotic and narcotic analgesics, antispasmodics, and local anesthetics in the form of blockades are used. To eliminate pain, it is necessary to influence the cause of its occurrence, so therapy includes the following drugs:
- Probiotics
. Medicines restore intestinal microflora and digestion, eliminate discomfort in the left lateral and lower abdomen. They are usually combined with pancreatic enzymes to quickly normalize the functioning of the gastrointestinal tract. - Laxatives
. For chronic constipation, oil-based rectal suppositories are prescribed to facilitate bowel movements. If they are ineffective, herbal remedies, osmotic laxatives, and oils for oral administration are used. - Intestinal antiseptics
. For infections and dysbiosis, non-absorbable drugs that act in the intestinal lumen are effective. Systemic antibiotics are used less frequently. - Corticosteroids
. Hormones of the adrenal cortex have a powerful anti-inflammatory effect in the treatment of UC. They help the disease go into remission and reduce pain in the left side. Steroids are often taken in combination with immunosuppressants, anticytokines.
For gynecological pain, female sex hormones are used. For pain that occurs due to neurological disorders, sedative herbal preparations and mild hypnotics are indicated. Physiotherapeutic methods are prescribed: electrosleep, neurosedative massage, reflexology. Patients are recommended to undergo psychotherapy.
Intestinal obstruction
The pathology is formed by many damaging factors and often occurs against the background of other diseases. The food bolus does not pass well through the intestines and may not move completely. The movement of feces is difficult. Pain occurs in different areas of the abdomen, depending on the location of the accumulation of feces. But most often it is found below, on the left.
Intestinal obstruction is characterized by the following processes:
- obstruction of the affected area with feces;
- spasms causing pain;
- swelling;
- blood flow disturbance;
- the formation of an acute inflammatory process with additional infection.
If feces remain in the intestines for a long time and are not released, the products of intoxication pass into the blood. Therefore, malaise and signs of an infectious disease develop.
With pathology, the following clinical symptoms develop:
- discomfort in the abdomen is observed to the left of the navel;
- absence or infrequent bowel movements;
- vomiting containing an admixture of bile, in severe cases - intestinal contents;
- hardness, tenderness of the abdomen when palpated, accumulation of feces is determined;
- in the area of accumulation of feces, a protrusion on the abdomen is visually distinguished;
- strong rumbling;
- dehydration with dryness and decreased skin turgor;
- dry mouth, severe thirst.
2-3 days after the initial development of the disease, the patient begins to experience severe pain. He characterizes it as follows:
- dull;
- spastic;
- increases at the height of the spasm.
If timely therapy is not available, the patient experiences complications:
- intoxication;
- shock.
Blood pressure drops, the skin becomes pale, cold sweat and rapid heartbeat increase. In this case, urgent hospitalization is required.
In severe cases, the patient may gradually stop complaining of persistent pain. This occurs if constipation persists. The condition indicates that the nerve endings in the affected area are damaged and completely die. Necrosis forms.
Treatment methods depend on the cause of obstruction:
- lack of intestinal motility - Bisacodyl, Proserin;
- formation of spasms - Spasmalgon, Halidor, Drotaverine;
- intoxication - intestinal lavage.
If there is no quality result, the pathological process continues to grow, necrosis forms, and surgical intervention is required. It is divided into the following types:
- removal of part of the intestine subjected to necrosis, adhesions, tumors;
- reduction of hernia, volvulus;
- establishment of drainage with antiseptic treatment in case of severe infection;
- manual removal of fecal plug.
To prevent the condition from recurring, it is necessary to identify the root cause and eliminate it.
Why does it hurt on the left side?
Physiological factors
The left side often hurts after physical activity. During intense exercise, blood flows to the abdominal cavity, particularly the spleen. This explains the characteristic stabbing sensations in the side, which disappear after 5-10 minutes of rest. The next day after training, pain in the left abdomen is possible due to tension in the abdominal muscles. The pain intensifies when getting out of bed, turning the body to the left, laughing and straining.
Constipation
Pain in the left iliac region occurs when there is no bowel movement for 2-3 days or longer. A person complains of a feeling of fullness and dull pain in the lower abdomen on the left. Periodically there is an urge to defecate, during which the pain intensifies and painful spasms are observed. The intensity of pain depends on the duration of constipation. Patients report the need to strain strongly during defecation, and a burning sensation in the rectum when passing dry stool.
Irritable bowel syndrome
IBS is the most common pathological cause of left flank pain. With this disease, painful sensations of various types are noted: dull, aching, sharp, constant or cramping. The most intense pain syndrome occurs in the morning after waking up, it is accompanied by painful tenesmus. After defecation, the pain decreases or disappears completely.
In some cases, to improve the condition, a person needs to visit the toilet several times in the morning, since after a single bowel movement there remains a feeling of incomplete bowel movement. During the day, pain in the left abdomen may be bothersome, but it is less intense. IBS sufferers do not have night pain that interferes with sleep. Typically, the pain syndrome increases with psycho-emotional stress, in women - before and during menstruation.
Sigmoiditis
With inflammation of the sigmoid colon, patients experience severe paroxysmal pain in the left side, which usually radiates to the lower back, perineum and thigh. The symptom is accompanied by a painful false urge to defecate, loose, foul-smelling stools mixed with mucus and blood. In acute sigmoiditis, such signs are observed constantly, and in chronic pain they are provoked by errors in diet, physical or mental stress.
Diverticulitis
Diverticula of the colon are manifested by moderate pain in the left half of the abdomen, which intensifies before the onset of bowel movements and disappears after bowel movement. The intensity of the pain increases if there is no stool for 3 or more days. Less common is paroxysmal pain that lasts several hours. In addition to pain, patients are concerned about stool instability - alternating constipation and diarrhea.
Nonspecific ulcerative colitis
UC is characterized by severe spastic pain on the left side above the ilium. When the pathological process spreads to the descending colon, pain is felt along the entire left side. The pain syndrome is accompanied by constant diarrhea; the stool contains large amounts of blood and mucus. During the period of remission, there is aching pain and discomfort in the abdominal cavity on the left. With UC, appetite disappears, weight decreases, and painful tenesmus is possible.
Chronic pancreatitis
Damage to the pancreas is characterized by mild aching pain in the left side. Soreness worries a person constantly, intensifies when eating large portions of food, eating fatty or fried foods. Sometimes severe paroxysmal pain develops, which lasts from several minutes to several hours. The pain syndrome in the chronic form of pancreatitis is combined with stool instability, flatulence, and rumbling in the abdomen.
Intestinal infections
Cramping pain in the left side occurs during infectious processes that occur with colitis syndrome - dysentery, amoebiasis, some forms of escherichiosis and salmonellosis. Severe pain begins 12-48 hours after eating contaminated food or water. They are accompanied by painful tenesmus and diarrhea up to 10-20 times a day. During defecation, feces with blood and mucus are released, and there is a stool of the “rectal spit” type.
Colon tumors
With benign intestinal polyps, dull pain in the left side without clear localization is observed. The symptom is not associated with eating or defecation. Increased pain occurs as the polyps increase in size, which creates obstacles to the movement of feces. A person feels a strong distension in the flank or iliac region on the left. Chronic constipation occurs; patients strain or help themselves with their hands to pass feces.
Discomfort in the left side is a sign of cancer of the sigmoid or descending colon. As the tumor grows, severe abdominal pain appears, which is constantly present and does not depend on external provoking factors. Against the background of pain, alternating constipation with diarrhea develops, and traces of fresh blood are found in the stool. Unbearable pain in the left side indicates the disintegration or ulceration of the tumor, its germination into neighboring organs.
Hernias
Pain in the lower abdomen is possible with a left-sided inguinal hernia. When a hernial protrusion forms, a dull pain occurs, which intensifies with straining, physical activity, and bending of the body. With large hernias, irreducible or strangulated hernias, patients complain of severe pain. More rare causes are a hernia of the Spigelian line on the left, a postoperative hernia.
Gynecological diseases
The appearance of pain in the left side in women is often caused by pathologies of the internal reproductive organs. The pain varies depending on the degree of activity of the process and the depth of tissue damage. Gynecological abdominal pain is characterized by intensification 2-3 days before menstruation, irradiation to the pubic region and perineum, dyspareunia (painful sexual intercourse). Most often, pain in the lower abdomen on the left occurs with left-sided adnexitis, endometriosis, and ectopic pregnancy.
Kidney damage
Pain in the left side is observed during exacerbation of urolithiasis - left-sided renal colic. Worrying painful constant or paroxysmal pain that radiates along the ureter to the lower abdomen and perineum. Patients rush around the bed or room, trying to find a position in which the pain will not be so intense. The symptom is accompanied by fever and urinary retention.
Complications of pharmacotherapy
Pain in the left iliac zone occurs due to dysbacteriosis (dysbiosis) caused by the use of antibiotics. Patients complain of constant discomfort in the abdomen, spasms in the left side, worsening after eating and before defecation. When bowel movements occur, greenish feces with a foul odor are released, stools become more frequent up to 3-7 times a day. Characteristic signs of dysbiosis: flatulence and rumbling in the intestines, malabsorption syndrome, lack of appetite.
Flatulence
This is a condition in which the normal balance of intestinal microflora is disrupted, resulting in increased gas formation. Normally, the maximum production should be no more than 0.5 liters of gases. If their volume increases to 2 liters, a pain syndrome forms below, on the left.
The condition often develops due to physiological changes:
- prolonged constipation;
- eating too much food;
- fermentation of the food bolus.
Less commonly, the condition is formed due to pathologies of the digestive tract, which disrupt the process of production and elimination of gases. Therefore, the following clinical signs are formed:
- bloating of the abdomen, in which the wall becomes hard and elastic;
- belching, heartburn, hiccups, nausea;
- removal of gases that have a putrid odor;
- frequent spasms;
- impaired fecal formation with the development of constipation;
- deterioration of health, malaise, heaviness in the stomach.
The following treatment methods have been identified:
- eliminating fermentation in the intestines, which leads to increased production of gases, use Mezim, Digestin, Festal, they normalize the digestion process;
- a diet with a reduced amount of foods that cause rotting, fermentation, and increased gas formation.
It is necessary to exclude cabbage, legumes, peas, and fresh baked goods from the diet.
Visceral pain
The cause of visceral pain can be functional disorders and organic changes in the organ. With functional disorders, this type of pain appears due to a decrease in the pain threshold and can affect all parts of the gastrointestinal tract2. In diseases of the digestive tract, visceral pain can be triggered by stretching, lack of blood supply, or peristalsis. Usually the patient feels it in the midline of the abdomen and is not able to accurately indicate the painful point2.
- The nature of visceral pain is cramping, with periods of subsiding and increasing pain. More often it can be described as aching, much less often - stitching or burning.
- Pain in diseases of the gastrointestinal tract can be caused by errors in diet, alcohol intake and exposure to factors such as running, bumpy riding, etc.
- The severity of pain can be reduced by warming or taking antispasmodics3.
Tumor processes
At the first stages of the process, tumor formation is difficult to detect. Therefore, they are found in the following cases:
- preventive examination of the digestive tract using instrumental tests;
- urgent visit to a doctor due to the development of pain.
The main danger of tumor development is late detection. It continuously produces atypical cells that spread throughout the digestive tract, penetrate the systemic bloodstream, and form metastases in neighboring organs.
The more the tumor grows, the more it compresses the intestinal wall, so patients develop pain. It doesn’t bother him much, it forms sporadically. The larger the lesion, the more the tissue is compressed and the pain increases. It can only be eliminated after taking analgesics. There are a number of additional symptoms:
- increased gas formation, abdominal enlargement;
- severe pain when pressing on the epigastrium;
- loss of body weight with the gradual development of cachexia even with normal food intake;
- decreased appetite, weakness, malaise;
- anemia, which develops as a result of damage to the intestinal wall, from which blood is constantly released;
- increasing heartburn, accompanied by heaviness in the epigastrium;
- nausea, vomiting with mucus and blood;
- impaired stool formation, accompanied by periodic episodes of constipation and diarrhea;
- intestinal obstruction due to tumor enlargement;
- rupture of the intestinal wall with the formation of peritonitis, causing the risk of sepsis;
- black stool mixed with blood;
- the addition of a secondary infection that provokes purulent discharge in the feces;
- pain during defecation;
- belching, hiccups, flatulence.
To eliminate malignant neoplasms, complex treatment is recommended:
- Surgical intervention
. It is necessary to remove the entire tumor and adjacent tissue to prevent recurrence. - Chemotherapy
. The patient is administered cytostatics that destroy atypical cells. With therapy, the tumor gradually decreases in size so that it is easier to remove surgically. In non-adjuvant therapy, the tumor is initially excised, then cytostatics are administered to reduce the risk of relapse. The most commonly used are Oxaliplatin and Capecitabine. - Radiation therapy
. The device is aimed directly at the tumor so that the radiation spreads only to the area where malignant cells develop, without affecting healthy tissue. They are being destroyed. Radiation therapy is usually used as preparation for subsequent surgery. This makes it easier for the oncologist and surgeon to remove the tumor without affecting normal tissue. - Surgical intervention
. This is the most radical, but at the same time effective treatment method. I use it only if more gentle methods of therapy do not help. It is important to remove the entire tumor as well as adjacent tissue. It is also necessary to identify areas of metastases and subsequently remove them.
Chemotherapy, if used incorrectly, is dangerous to human health. It is necessary to follow all the recommendations prescribed by the oncologist to reduce the risk of side effects. It is important to eat right, maintain a healthy lifestyle, and take vitamins.
All treatment methods are selected only by the attending physician. It takes into account the individual characteristics of the body, the degree of spread of the malignant process, the presence of chronic diseases and other abnormalities. This will help reduce the risk of a negative reaction to the therapy.
Diverticulitis
With pathology, nodes form on the intestinal wall, which lead to protrusion. They are called diverticula. Pathology develops due to prolonged accumulation of stagnant food. The condition usually develops more often in women.
The pathology has multiple etiologies. Develops under the following conditions of the body:
- a diet with a decrease in the amount of fiber, as a result of which diverticula can grow for many years (pathology intensifies in people who often consume processed foods, baked goods, excluding plant foods);
- chronic dysbiosis caused by decreased immune function;
- helminthic infestation, causing disruption of the structure of the intestinal walls, irritation, and the formation of a prolonged inflammatory process;
- the spread of bacteria and fungi that cause inflammation.
People with a family history of diverticulitis are susceptible to diverticulitis. That is, their close relatives must suffer from chronic inflammatory diseases of the digestive tract, including diverticulitis.
With diverticulitis, a dull and aching pain develops. Additionally, the following negative symptoms are characteristic:
- constant, monotonous pain, spreading only to one area of the abdomen;
- periodic alternation of diarrhea and constipation due to impaired stool formation;
- discharge of blood into stool;
- low-grade fever that develops as a result of inflammation of the mucous membrane;
- increased discomfort, especially during defecation or pressing on the abdomen;
- nausea, vomiting, abdominal discomfort, decreased appetite.
A number of techniques are used to treat diverticulitis:
- antibacterial drugs that affect only the digestive tract - Cefoxitin, Timentin;
- anti-inflammatory drugs that eliminate swelling - Salofalk;
- antispasmodics - Drotaverine, No-shpa;
- painkiller based on NSAIDs - Nise, Nimesulide.
Other drugs are symptomatic treatments. That is, as negative signs arise, medications are supplemented.
If discomfort occurs in the stomach or lower abdomen, the presence of a digestive pathology is suspected. To identify its location, a general examination is not enough. It is important to conduct diagnostic tests using laboratory and instrumental tests. Without this, it is impossible to identify the exact localization of the damaging process.
Diagnostics
During the examination, the gastroenterologist pays attention to the exact localization of pain identified by palpation of the abdomen and evaluates the symptoms of peritoneal irritation. Valuable information can be obtained from a digital examination of the rectum and a standard gynecological examination. To confirm the diagnosis, a set of laboratory and instrumental examination methods is prescribed, which includes:
- X-ray studies
. To quickly assess the condition of the intestines, a plain X-ray of the abdominal cavity is performed. To visualize the mucous membrane and identify ulcerative or tumor defects, radiography with oral contrast and irrigoscopy are performed. CT is used to refine the image. - Endoscopic methods
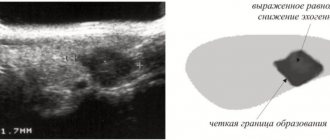
. The main method for diagnosing lesions of the large intestine is colonoscopy, which allows you to examine the intestinal wall and identify signs of an inflammatory or tumor process. During a colonoscopy, a biopsy of suspicious areas of the mucosa is taken. Rectosigmoidoscopy is used less frequently. - Sonography
. Ultrasound is informative for identifying hernias of the anterior abdominal wall. Ultrasound examination of the pancreas and hepatobiliary zone is indicated for suspected chronic pancreatitis. Women must undergo a pelvic ultrasound to rule out gynecological diseases. - Stool tests
. In the coprogram, the levels of muscle fibers, starch grains and neutral fats are assessed, the increase of which indicates malabsorption and a problem with the secretion of pancreatic enzymes. In the presence of inflammation, a large number of leukocytes and mucus are found in the stool. Stool culture is carried out using the Gregersen reaction. - Additional methods
. Sometimes laparoscopy and positron emission tomography are prescribed for differential diagnosis. When examining women with complaints of pain in the left side, colposcopy and hysterosalpingoscopy are performed. Clinical and biochemical blood tests are performed.
Palpation of the left iliac region