What are the dangers of losing weight in a cancer patient?
Cancer patients, regardless of the amount of food they eat and their physical activity, suffer from hypermetabolism (increased energy expenditure).
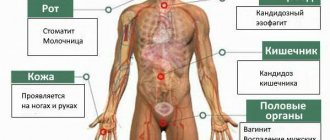
Lysis or destruction of deposits of sugars, proteins and fats causes a shortage of reserves, weakening the body in the fight against cancer, if this also causes difficulties with food. As a result, anorexia develops with decreased appetite and exhaustion. The following complications appear:
- fatigue (asthenia);
- anemia (decreased red blood cell levels);
- fluid retention and swelling;
- atrophy of muscle structures.
And these are not all the complications that worsen the quality of life of patients, increase inertia and dependence. Changes in appearance are fraught with deterioration of the psychosocial situation, complicate cancer treatment and worsen the prognosis of recovery.
Identifying patients at risk of malnutrition requires knowledge of tumor location, stage, treatment, intercurrent illnesses, and problems that impair nutritional intake. The following symptoms are taken into account:
- lack of appetite;
- fast saturation;
- difficulty swallowing;
- dry mouth and constipation;
- depression and anxiety.
Patients with advanced cancer and no active cancer treatment (palliative care phase) are, regardless of other factors, at high risk of malnutrition. This is observed primarily in cancers of the digestive tract, head, neck, lungs or ovaries.
There is a high risk of digestive problems and loss of appetite during chemotherapy (30-50% chance of symptoms with serious impact on nutrition). Immediate preventive measures are required to prevent toxic events, including vomiting, mucositis, diarrhea, and sensory changes that cause aversion to certain foods.
What types of cancer cause weight loss?
Losing body weight is not the first sign of cancer. This symptom develops in the later stages, when there is no longer any doubt about the progression of the malignant process in the body. In most cases, if a diagnosis has not been made for one reason or another, and the person has suddenly and significantly lost weight, we are talking about metastasis, and not about the initial stages of the development of the disease.
Weight loss for stomach or pancreatic cancer, in which 8 out of 10 patients develop cachexia. When this symptom appears, tumor operability is rare. With a malignant tumor of the lung, severe joint and muscle pain, as well as fever, accompany a sharp weight loss. In this case, weight loss is a secondary symptom.
Anorexia-cachexia syndrome is characterized by 4 symptoms:
- decrease in skeletal muscle mass;
- complete lack of appetite (anorexia);
- quick satiation with a small amount of food;
- constant unreasonable fatigue.
Weight loss within SACOB is typical for cancer of the uterus, prostate and lungs. In patients with malignant tumors of the mammary glands, it occurs in ¾ of cases. In the later stages of progression of the malignant process, anorexia-cachexia syndrome develops in all forms and types of cancer.
When treating malignant tumors, the patient has to lose weight repeatedly. Before surgery, appetite worsens due to stress. After surgery, you cannot eat the way you want. Because you need to adhere to a special diet. In this case, appetite is restored after 3-4 weeks and body weight returns to normal. With bowel cancer, weight loss takes longer, which is associated with a longer rehabilitation period.
A course of chemotherapy is accompanied by the development of adverse reactions such as nausea and vomiting, as well as damage to the mucous membranes of the gastrointestinal tract and oral cavity. During this period, patients have no time to eat at all. Drug-induced anorexia is characterized by severe suppression of appetite.
During radiation therapy for cancer of the mediastinal organs, breast and lung with areas of lymphatic drainage, nausea is also initiated due to damage to the mucous membranes of the esophagus. When exposed to the organs of the genitourinary system, the rectum and intestines are affected, which also leads to a deterioration in appetite. In this case, there is also a need to limit nutrition to reduce the number of bowel movements.
In the situations considered, body weight decreases by no more than 5% of the initial indicators and after the end of therapeutic manipulations, the index tends to increase. The main criterion for cancer cachexia or chemotherapy and radiation therapy is uninterrupted weight gain after completion of the procedures.
Dyspepsia: causes and diagnosis
Experts classify dyspepsia syndrome as a set of clinical symptoms that occur when gastric emptying is disrupted (slowed down) due to the patient not only having diseases of the digestive system, but also other body systems.
The symptoms united by the term “dyspepsia” traditionally include:
- A feeling of heaviness in the abdomen (a feeling of fullness in the stomach), most often occurring after eating (both immediately and several hours after eating) - some patients interpret these sensations as a dull aching pain in the epigastric or periumbilical areas
- Feeling of quick satiety
- Nausea (both on an empty stomach in the morning, aggravated by the first meal, and occurring immediately or several hours after eating)
- Vomiting (a possible, but not obligatory symptom), if it does occur, then after it comes, even if short-lived, relief (reduction in the manifestations of dyspepsia)
- Bloating (flatulence) with or without belching of air
- The named symptoms and severity in each individual patient can vary widely. A combination of dyspepsia with heartburn, pain behind the sternum when swallowing (symptoms caused by diseases of the esophagus, most often gastroesophageal reflux disease), as well as a change, often a decrease, in appetite is possible.
Dyspepsia syndrome is a fairly common manifestation of various diseases and, according to various sources, occurs in at least 30-40% of the world's population. If we take into account single episodes of dyspepsia that occur during acute enteroviral infections or the response to acute toxic damage to the gastric mucosa by a wide variety of factors, including alcohol and drugs, then these figures should at least be increased by 2 times.
To better understand the causes of dyspepsia, we should briefly talk about what happens to food in the stomach of a healthy person.
The process of digestion of food in the stomach (Fig. 1)
When food enters the stomach, a change in the configuration of the organ occurs - the muscles of the body of the stomach (1) relax, while the outlet section (antrum - 2) contracts.
In this case, the pyloric canal (3), which is a muscle sphincter, or sphincter, remains practically closed, allowing only liquid and solid food particles less than 1 mm into the duodenum (4). In response to food entering the stomach, its cells increase the production of hydrochloric acid and the digestive enzyme pepsin, which provide partial chemical digestion of proteins (along with mucus, the main components of gastric juice).
At the same time, the activity of the muscle cells of the stomach increases, due to which the solid components of food are mechanically crushed and mixed with gastric juice, which facilitates its chemical digestion. This process, with increasing intensity of muscle contractions of the stomach wall, lasts about 2 hours. Then the pyloric canal opens and with several powerful contractions the stomach “expels” the remaining food into the duodenum.
Then comes the phase of restoration (rest) of the functional activity of the stomach.
Causes of dyspepsia
As already mentioned, in most cases, dyspepsia is caused by slow gastric emptying. It can be either functional (without signs of damage to organs and tissues) or organic in nature. In the latter case, dyspepsia occurs as a manifestation of diseases of the stomach and other organs and systems of the body.
Functional disorders of gastric emptying as a result of irregular nutrition, reduction of time and violation of eating conditions (stress, constant distraction by extraneous activities while eating - active and emotional discussion of any issues, reading, doing work, movement, etc.), overeating , regular intake of foods that slow down gastric emptying (primarily fats, especially heat-treated ones), exposure to other factors (so-called non-ulcer dyspepsia) Functional disorders of gastric emptying as a result of damage (mismatch) of central (located in the central nervous system) regulatory mechanisms (neurological and mental illnesses) Organic diseases of the stomach:
- Gastritis (inflammation)
- Acute – acute massive impact on the stomach wall of bacteria and their metabolic products that enter the body from outside
- Chronic - long-term exposure to the wall of the stomach of bacteria and their metabolic products (Helicobacter pylori is a microorganism, the presence of which in the stomach is associated with the occurrence of peptic ulcers, gastritis, tumors), bile (with its regular reflux into the stomach from the duodenum), an autoimmune process with damage body and/or antrum of the stomach, the influence of other pathogenic factors (see below)
- Tumors, mainly those that are located in the outlet (antrum) region and mechanically impede the exit of food from the stomach
- Benign
- Malignant
- Peptic ulcer complicated by reversible inflammatory edema (completely disappears after healing of the ulcer) and/or cicatricial deformation of the outlet of the stomach or duodenum (completely irreversible and, with progression, needs to be eliminated surgically)
- Accumulation in the stomach of substances that cannot be digested and removed from the stomach naturally (so-called bezoars, consisting of hair compressed and glued together with mucus, peels of vegetables and fruits, etc.)
- Diseases of the gallbladder and biliary tract: cholelithiasis, dyskinesia, condition after removal of the gallbladder (bile enters the duodenum not only with the intake of food, but also in the absence of it, which facilitates the reflux of bile into the stomach with the development of “gallitis”, or reflux gastritis)
- Diseases of the pancreas (inflammation – pancreatitis, tumor)
- Endocrine diseases (diabetes mellitus, inflammatory and tumor diseases of the thyroid gland, accompanied by a decrease in its function)
- Long-term use of medications that can both damage the mucous membrane of the stomach and duodenum (acetylsalicylic acid, or aspirin, non-steroidal anti-inflammatory drugs) and slow down the evacuation of food from the stomach (aluminum-containing antacids, for example, Almagel, psychotropic drugs, various antispasmodics etc.)
- Chronic liver and/or kidney failure due to various diseases of these organs (exposure to the stomach of toxic substances that are not neutralized by the liver and/or kidneys as a result of disruption of their functions)
- Other rare diseases and conditions
- Pregnancy
- Nausea and vomiting, sometimes uncontrollable, can be manifestations of neurological diseases accompanied by increased intracranial pressure, and therefore these symptoms are associated with headaches, sometimes very intense. In such cases, the connection between the manifestations of dyspepsia and food intake is not clearly visible; on the contrary, these symptoms often appear against the background of high blood pressure
The appearance of dyspepsia forces most people to seek help from a doctor.
Patients whose dyspepsia first appeared at the age of 45 years or older, as well as those (regardless of age) who have one or more of the following symptoms: repeated (recurrent) vomiting, weight loss, must necessarily consult a specialist. (if it is not associated with dietary restrictions) pain when food passes through the esophagus (dysphagia) proven episodes of bleeding gastrointestinal bleeding (vomiting “coffee grounds”, loose tarry stools) anemia Of course, the cause of dyspepsia in each case must be determined by a doctor . The patient’s task is to clearly state his symptoms so that it is easier for the doctor to understand the cause-and-effect relationships between them.
To do this, the patient must answer the following questions to the doctor:
- How are the symptoms of dyspepsia related to food intake (occur on an empty stomach in the morning; immediately after eating, if yes, then is there a connection with the nature (liquid, hard, spicy, fatty, etc.) of food; several hours after eating or in the evening; do not depend on the time of meal and its nature)?
- How long does dyspepsia last if nothing is done?
- After what (take liquids, tablets, etc.) and how quickly does dyspepsia go away?
- How long does dyspepsia last without symptoms?
- Is there a connection and, if yes, then what, between the manifestations of dyspepsia and other symptoms that the patient has (for example, dyspepsia is accompanied by abdominal pain, after eliminating dyspepsia the pain disappears or not)
- If vomiting is a manifestation of dyspepsia, it is necessary to clarify what is contained in the vomit (fresh blood, contents resembling coffee grounds, remnants of food eaten just or more than 2-3 hours ago, colorless mucus or colored yellow-brown), as well as did vomiting bring relief?
- How stable has your body weight been over the past 6 months?
- How long ago did dyspepsia appear, is there a connection (according to the patient himself) between its appearance and any events in his life?
- How did the severity of the symptoms of dyspepsia change from the moment of its onset to the visit to the doctor (did not change, increased, decreased, their wavy course was observed)?
- Important for the doctor is information about the presence of concomitant diseases in the patient, for which the patient regularly takes medications (which ones, how often, for how long), about possible contact with harmful substances, about the peculiarities of the regime and diet.
Then the doctor conducts an objective examination of the patient using “classical” medical methods: examination, tapping (percussion), feeling (palpation) and listening (auscultation). A comparison of the data obtained during an objective examination with the information obtained during a patient interview allows the doctor, in most cases, to outline the range of possible diseases and conditions that could cause the appearance of dyspepsia. In this case, such important factors as gender, age, ethnicity of the patient, his heredity (the presence of diseases associated with dyspepsia in blood relatives), time of year and some other factors must be taken into account.
How much weight do cancer patients lose?
Losing more than 5% of body weight when no attempt is made to lose weight can be an early sign of cancer. Therefore, unexplained weight loss should not be ignored.
It is unclear what causes cancer wasting syndrome or cancer cachexia. It is assumed that malignant cells replicate exponentially* and consume energy during replication.
*replicate exponentially – increasing over time not only the value, but also the growth rate
How to stop losing weight and gain lost kilograms?
Cancer is one of the biggest threats to human life. In many cancers, sudden weight loss is one of the most dangerous manifestations. And this should be an urgent reason to visit a doctor.
The main problems of most cancer patients are related to the consumption of low amounts of protein and insufficient calories. Eating high-calorie and protein-rich foods is essential to provide energy to help the body fight disease.
Dietary recommendations for cancer:
- good sources of protein include lean meat, fish, poultry, nuts, dairy and/or soy products;
- To gain strength and feel better, patients are advised to take vitamins, minerals, and carbohydrates (fruits, vegetables and whole grains).
Not having enough of these nutrients can cause cancer patients to feel tired, weak, and less able to cope with treatment.
Even if the process of depletion of the body has already gone too far, doctors are faced with the task of maintaining the life of the patient and improving his condition. The measures taken are aimed at eliminating symptoms that negatively affect the supply of nutrients: damage to the mucous membranes, nausea and vomiting. Medicines are also prescribed to relieve pain and improve appetite.
How to get rid of constant hunger
The first thing you need to do is figure out what its source is.
- A disease means you should see a doctor and get treatment;
- Psychosomatics – get rid of stress, groundless fears, come out of the shadows onto the bright side of life;
- Violation of the regime - try to comply with it, adhering to a healthy lifestyle.
If all of the above does not apply to you, but the feeling of hunger still does not go away, depriving you of peace, try to fight the bad habit of continuously chewing, using psychological tricks. This will help trick the brain and reduce the feeling of emptiness in the stomach:
- eat food while sitting, slowly, without a book or TV;
- consume food consciously, chewing slowly, this way satiation occurs faster;
- use small plates, so the portions will seem larger;
- give up spices that stimulate the appetite, but lay out the dish beautifully and decorate it.
Herbal decoctions of mint, parsley, fig compote, and plums help suppress the appetite.
After each meal, rinse your mouth with mint mouthwash.
Before going to bed, if you feel a lot of pain, drink warm water with a spoon of honey. This will give a feeling of fullness in the stomach, and glucose, once in the blood, will signal the brain about satiety.
Try to fill your free time with important things so that you are distracted and forget about food.
If your route to work passes by a bakery or candy store with a generous display of sweets and pastries, change the route so as not to be tempted, nor to irritate your imagination, nor expose your weak will to temptation.
What can you do yourself?
One of the main goals when fighting cancer is weight maintenance, so proper nutrition is of utmost importance. When cachexia develops, it is necessary to increase the total intake of beneficial nutrients.
Regardless of the causes of malnutrition, cancer patients receive therapy to reduce the impact of treatment and side effects. The team of doctors, working closely with the patient, makes every effort to maintain weight in a healthy range. Medicines to treat nausea and vomiting and steroid medications to increase energy may also be prescribed.
However, each patient should take independent steps to maintain a healthy weight and build strength:
- Maintain a balanced diet
. You need to make sure you have enough protein in your diet. Consuming adequate amounts of protein can help maintain body weight. - Increase your calorie intake
. A cancer patient's body uses energy to fight cancer, so it makes sense to get more calories each day. - It is recommended to reduce portions, but increase the number of meals
per day. Instead of three meals a day, you can eat 5-6 times a day. - Increase fluid intake
. To prevent dehydration and increase energy at the same time, you should drink more fluids. These can be juices, broths, cocktails, etc. - Keep a diary
. Helps monitor the patient’s well-being after eating certain foods. It is also recommended to note any new side effects that may develop during treatment. Monitor fluid and medication intake. Clear information about these things will help develop a better strategy to fight cancer. - Include physical activity
. It is enough to take walks in the fresh air every day to activate your metabolism and strengthen your body.
Dietary recommendations for cancer patients are aimed at helping the patient cope with the consequences of the disease and speed up recovery. Dietary therapy helps you get enough calories to maintain a healthy weight, gain strength, and prevent tissue breakdown and infection.
Eating disorder - symptoms and treatment
Social influences
In modern European culture, the ideal characteristics of a female figure are slimness and flexibility.
As a result, most young women in the United States and Europe go on some kind of diet, hoping to control their weight and improve their figure. It is not surprising that NB is most common among the female part of the population: it affects mainly Caucasian women of the middle and upper middle social class. They follow a diet because they want to conform to the ideology of their social class and the formal signs of a “high position” in society. It is curious that the opposite trend is demonstrated by the Latin American and African American part of the female population, where curvy figures combined with an athletic physique are the criterion of superiority and attractiveness.
It is possible that globalization and the mixing of cultural ideas about the figure will soon lead to some changes in the criteria of female attractiveness. Thus, along with advertising and promotion of slimness, there are almost opposite requests in plastic surgery (for example, increasing the size of the buttocks in women). The interpenetration of cultural ideas, the abundance of visual data, along with the simplification of the exchange of opinions on social networks, are likely to change the specificity and prevalence of eating disorders.[12][16][31]
Diet
The desire to be slim forces you to diet. Diet in this case is a strict, unhealthy restriction on the quantity and, often, quality of food consumed. Observations by specialists show that after periods of dietary restrictions, a kind of “rollback” occurs: a tendency to overeat arises. Often the change in phases of “diet - overeating” is caused by stress factors (conflicts, quarrels, infidelity, divorces, dismissals, etc.) Reliable studies show that young women who are already on a diet are more likely to develop eating disorder. In particular, one British study showed that schoolgirls who were on a diet were 8 times more likely to suffer from an eating disorder.
However, dieting is not a risk factor for overeating. As noted earlier, women suffering from this problem are much less likely to follow a diet.
Although there is a significant connection between dieting and the occurrence of the disorder, diet alone is clearly not enough to cause the disease. Obviously, the interaction of several factors is necessary. One study of risk factors found that eating disorders most often develop in women who are prone to obesity and mental disorders. In particular, emotionally unstable personality disorder is often accompanied by dysmorphophobia (excessive striving for ideality) and is a parameter that predicts eating disorder. There is an opinion that a strict diet is a variant of self-harmful behavior in this personality disorder. An “obsession” with food or the lack thereof distracts patients from experiencing severe “emotional pain,” and anxiety about the “imperfection” of one’s own figure plays approximately the same role.
How can dieting contribute to the development of eating disorder in women?
The practice of psychotherapy shows that such patients tend to exorbitantly overestimate social standards in relation to themselves and suffer from perfectionism. On a mental level, these unrealistic standards literally shut women out from meaningful interactions with other people. Getting objective feedback from others becomes almost impossible. Under such conditions, women who tend to diet easily lose control of their emotions. Next comes the all-or-nothing cognitive reaction. This phenomenon has been called the “abstinence-breaking effect.” Thanks to him, such patients completely lose control of themselves. As a result, they give up the ability to regulate their food intake and, at best, overeat.
Repeated diet violations and chaotic eating destroy the conditioned reflex connections of the body, which normally regulate normal nutrition. For example, abruptly stopping food intake due to the urgent intention of losing weight, without paying attention to the feeling of satiety, coupled with a lack of regularity in eating, can turn off conditioned satiety responses, which, in turn, will cause an episode of overeating.
Following a diet also leads to neurohumoral consequences. Thus, even a short-term diet can lead to serotonin dysfunction in the brain. Serotonin is an important neurotransmitter, regulator of mood and eating behavior. Its reduced level is associated with eating disorder (an interesting fact is that a lack of serotonin due to diet is observed only in women). As a result, a mutual reinforcement of two predisposing factors is formed: women are more likely to diet due to cultural pressure and at the same time become significantly vulnerable to the negative consequences of even a moderate diet due to the peculiarities of their biology.[5][18]
Family factors
Eating disorder occurs in close relatives of patients. The prevalence of ND among relatives of patients suffering from this disease is almost 4 times higher than among relatives of healthy people in the control group. AN is 12 times more common in relatives of patients with NB. This interdependence proves the existence of some common family predisposition. Parents of patients with eating disorder are significantly more likely to have obesity and alcohol abuse. It has been shown that the occurrence of ND is associated with excessive criticism from the parents of patients. More often this is expressed in the form of unflattering statements regarding girls’ weight, shape or eating habits.[5]
Genetic factors
The results of currently known twin studies are conflicting. Some reports show up to 30%, and sometimes up to 83%, of the influence of heredity on the formation of eating disorder. However, these results cannot be considered reliable due to the small size of the group of subjects and the complexity of describing the eating disorder phenotype. However, it is impossible to completely exclude the heredity of eating disorders. Therefore, in the interests of treating the disease, it should be considered that genetics is a factor whose influence should and can be minimized.[9]
What to do if you experience a sudden weight loss
Every fourth patient out of 20 patients with cancer dies from cancer cachexia. If you lose weight, it is recommended to immediately notify your doctor in order to take therapeutic measures aimed at correcting the patient’s condition. Take advantage of the services of oncologists with extensive practical experience who see you at the Medscan clinic in Moscow.
Our medical center uses a special approach to treating cancer patients, which differs from the generally accepted ones. To prevent unintentional weight loss, an early intervention strategy is used and a multidisciplinary approach is practiced. The attending physician works in a team with an oncopsychologist and nutritionist. An integrated approach is aimed at compensating the energy balance and maintaining a high quality of life for the patient.