If you find a yellowish plaque on your face in the eyelid area, on the cheek, slightly rising above the skin, not painful and moderately mobile, most likely it is a xanthoma or, as it is also called, xanthelasma. Xanthoma is a benign neoplasm with a soft consistency. It consists of fat cells, but, unlike lipoma, is not limited to the capsule. In addition, there is practically no risk of degeneration for this formation. And, nevertheless, such a manifestation should not be ignored.
Even a single skin xanthoma is perceived as a cosmetic defect. And if the formations are multiple, they can grow and merge, forming a large yellow spot, significantly worsening a person’s appearance. What causes such a neoplasm, what does it indicate, how to deal with it? Medical doctors answer frequently asked questions from patients.
What is xanthoma?
Xanthoma appears on the skin suddenly. As already mentioned, this is a non-cancerous formation that rarely degenerates. It consists of fat cells and directly indicates a violation of metabolic processes in the body. The spot does not itch or hurt. There are no symptoms such as redness or discomfort at the site of formation.
A yellow spot, slightly raised above the skin, is tactilely not very different from the texture of the skin. It is soft, without compaction. A common location is the skin of the upper eyelids. But a xanthoma may also appear on the cheek or forehead. Most often, education is limited to a small area. However, the clinical description of the disease in medical reference books suggests that in some cases significant areas of the skin may be involved in pathological processes. Xanthoma of the esophagus, stomach, colon, bladder, and other internal organs also occurs.
This type of formation is removed, rather, for cosmetic purposes, since they do not pose a direct threat to health. However, the appearance of such plaques on the skin may indicate serious problems with the metabolism in the body. Therefore, if multiple xanthomas are detected on the face and body, it is recommended to consult a family doctor.
As for treatment, you should not try to get rid of xanthelasma with folk remedies, since due to a burn when exposed to aggressive environments, mechanical removal of the tumor with sharp improvised objects can cause great harm to the skin. In this case, the risk of secondary infection with subsequent inflammatory process increases rapidly. And now, in place of a harmless xanthoma, a scar or scar appears.
Use the services of professionals if you want to get rid of this education. Laser removal of xanthomas is a common medical service. The clinic’s doctors guarantee complete painlessness, safety, excellent aesthetic results and high speed of treatment.
Features of the clinical picture and diagnosis
Gastric xanthomas do not have a characteristic clinical picture. Most often, they are discovered accidentally during a routine endoscopic examination or during an examination prescribed to diagnose another disease. Therefore, clinical manifestations are reduced to symptoms of the underlying disease.
If a patient has atrophic gastritis, then he is bothered by nausea, a feeling of fullness in the stomach, pain in the epigastrium, and belching. Digestive disorders are also observed in diseases of the liver and biliary tract, which also often cause xanthomatosis.
They are accompanied by heaviness and pain in the right hypochondrium, nausea, vomiting, jaundice, and with the development of liver failure - edema, increased bleeding.
In the presence of diabetes mellitus, the manifestations of high blood glucose levels come to the fore - increased thirst, frequent urination. In the case of widespread atherosclerosis, the patient is concerned about the symptoms of impaired blood flow in various organs: pain in the heart, dizziness, headaches, numbness, weakness, pain in the legs.
In the presence of a hereditary disease associated with a disorder of fat metabolism, the symptoms appear in childhood and are very diverse in nature: disorders of the nervous system, pain in the joints and muscles, restrictions in movement, xanthomas on the skin, vascular problems.
To diagnose xanthomas, an endoscopic examination of the stomach is performed, with a part of the neoplasm taken for a biopsy.
Peculiarities . In fact, a xanthoma biopsy is not a mandatory study, since it is a benign formation that is not prone to malignant degeneration. However, under the mask of xanthoma, cancerous tumors are sometimes hidden, which can have extremely diverse forms. In order not to miss a dangerous disease, microscopy of xanthoma tissue is performed.
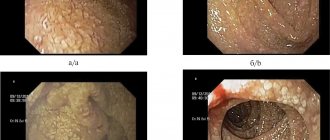
The endoscopic picture of gastric xanthomatosis is shown in this video:
https://endoscop.tv/videos/296/mnojestvennye-ksantomy-jeludka/
If xanthomatosis of the gastric mucosa is detected, the level of cholesterol and other lipids in the blood must be examined, and an ultrasound of the liver, biliary tract, a biochemical blood test for bilirubin, and liver enzymes are prescribed. This is necessary to establish the possible causes of the appearance of the tumor.
Reasons for appearance
There is no clear reason for the appearance of xanthomas. Dermatologists say that most often the pathology occurs in people with metabolic disorders and a history of the following conditions and diseases:
- high cholesterol;
- diabetes;
- endocrine diseases;
- obesity;
- pancreatic diseases;
- hypertension;
- kidney diseases;
- liver dysfunction.
Doctors do not rule out hereditary factors and hormonal disorders in older women as the causes of xanthomas. There is a connection between the appearance of formations and the abuse of fatty foods and insufficient care of the skin of the face.
It is important to note that cases of self-healing have been diagnosed. In some patients who adjusted their diet, xanthomas disappeared some time after starting the diet. But these are rather isolated cases.
What to do if xanthomas appear?
It is very important to consult a dermatologist if you discover xanthomas. Do not forget that their appearance is associated with lipid metabolism disorders. This is a warning about a threat to health and life. The consequences of untimely measures can be very sad - from the development of cardiovascular diseases to death. However, you should know that qualified diagnosis and timely treatment can normalize impaired lipid metabolism and protect you from unwanted complications.
Gorskaya Irina Vladimirovna
, dermatovenerologist, dermatologist, trichologist, medical cosmetologist in Makhachkala, specialist of the highest category.
Types of xanthoma
Diagnosis of xanthoma is not difficult. The characteristic location and appearance of the formations speak for themselves. At a doctor’s appointment, a visual examination method, dermatoscopy, is used to confirm the diagnosis. Using a special digital device, the doctor examines the skin defect at multiple magnification. Its size, shape, structure are assessed. Xanthomas of internal organs are detected during ultrasound and computed tomography. Let us dwell on the types of xanthomas in a little more detail.
Xanthoma eyelids
Xanthoma on the eyelid is the most common manifestation of formations of this type. It is more often diagnosed in women over 45 years of age. But it can also appear in patients of other categories.
Tuberous xanthoma
The disease is manifested by the formation of brown nodules 1-5 cm in size on the skin. Localization - legs, palms, buttocks. The danger of this type of disease is that plaques can form in the coronary arteries, since patients with this type of disease almost always have elevated blood cholesterol levels.
Xanthoma of the stomach
Gastric xanthoma is a formation that looks like a fatty deposit on the mucous membranes of the stomach. Most often this is a xanthoma of the antrum of the stomach. Plaques are diagnosed in patients of the older age group who have advanced atherosclerotic processes. Other parts of the gastrointestinal tract may also be affected, for example, in some patients esophageal xanthoma is detected.
Tendon xanthomas
Formations appear on the extensor tendons of the fingers and on the tendons of the lower leg. Tendon xanomas look like dense, mobile formations of a flesh-colored or yellowish color. When the limbs move, the plaques also move.
Eruptive xanthoma
This name is given to a disease in which many flat and semicircular yellow xanthomas appear. They are soft and clearly defined. Merging of formations is often observed. And then one large plaque appears. Lumps and plaques can cause itchy skin.
Newspaper "News of Medicine and Pharmacy" Gastroenterology (337) 2010 (thematic issue)
Gastric xanthoma (gastric xanthelasma) (GC) is a benign formation, the clinical significance of which remains unclear today, and the literature data are extremely scarce.
Macroscopically, xanthomas are defined as single or multiple yellowish or yellowish-whitish spots, plaques, or lentil-like flat or raised structures with clear edges in the gastric mucosa. Their sizes vary from 0.1 to 1.5 cm [1, 2].
Histologically, xanthomas are represented by a cluster of foam cells (macrophages) containing lipids. Xanthomas are usually located in the own layer of the mucous membrane (ML) of the stomach, but sometimes reach the muscular plate. They are most often localized in the antrum and lower third of the body of the stomach, but with severe duodenogastric reflux (DGR) they can also occur in the upper parts [1, 2].
As already noted, the problem of gastric xanthomatosis is extremely poorly reflected in the literature. The etiopathogenesis of QOL is unknown, but it is believed that there is a relationship between QOL and hyperlipidemia, diabetes, and atrophic gastritis [1–4]. There are separate works regarding the relationship between QOL and Helicobacter pilori infection (F. Arevalo, 2005; S. Gursoy, 2005; S. Hori, 1996; H. Isomoto, 1999). According to the authors, Hp infection can provoke the appearance of QOL [2, 5–7]. There is also an opposite view: according to S. Yi et al. (2007), the presence of QoL is not interrelated with HP [4].
The clinical significance of QoL, according to the literature, remains unclear. M. Naito et al. believe that the presence of QOL may be a marker of pathological age-related changes in the gastric mucosa [8]. We came across several studies on the combination of QOL with hyperplasiogenic polyps and early gastric cancer [9, 10]. S. Gursoy et al. (2005) found a relationship between QOL and chronic gastritis, operated stomach (during the formation of a gastrointestinal anastomosis), intestinal metaplasia and HP, that is, with precancerous conditions of the stomach [2].
According to V.A. Romanov, xanthomas most often occurred in middle-aged and elderly patients against the background of atrophic gastritis with duodenal reflux and intestinal metaplasia, in 70% of cases in early intestinal-type gastric cancer [1]. The author believes that QOL can be included in the so-called satellites of early cancer.
According to most experts, there is no need to take biopsies from xanthomas. But given the fact that in some cases, malignant formations of the stomach can imitate xanthomas, some authors consider it necessary to conduct a morphological study of QOL with careful dynamic monitoring of such patients [2, 11].
Thus, the limited and contradictory data regarding the role of gastric xanthomatosis necessitated the need for us to further study this problem.
As part of the research work “To study the mechanisms of development of precancerous conditions of the stomach under the influence of exo- and endogenous factors and to substantiate the principles of inhibition of the leading links in the formation of the pathological process,” we studied the frequency and role of gastric xanthoma in patients with chronic gastritis.
We examined 122 patients with chronic gastritis (29 men, 93 women aged from 25 to 71 years, average age 49.9 ± 2.1 years). Endoscopic, histological, cytological studies, daily pH measurements, and statistical analysis of the data obtained (multivariate correlation analysis) were performed.
In 21 patients (8 men, 13 women), average age 43.3 ± 3.5 years, non-atrophic gastritis (NAG) was diagnosed.
101 patients (21 men, 80 women), average age 49.30 ± 1.16 years, were diagnosed with atrophic gastritis (AG). Depending on the severity of morphological changes in the gastric mucosa, these patients were divided into the following groups: Group I - atrophy of the gastric mucosa (n = 53);
Group II - atrophy and intestinal metaplasia of the gastric mucosa (n = 35);
Group III - atrophy, intestinal metaplasia and dysplasia of the gastric mucosa (n = 13).
Endoscopic examination (esophagogastroduodenoscopy) with biopsy of the antrum and body of the stomach was carried out according to the generally accepted method using Olympus fibrogastroduodenoscopes (Japan). To improve the quality of endoscopic examination in order to visualize minimal macroscopic changes in the gastric mucosa, the antifoam agent espumizan was used in all cases at a dose of 3–5 ml orally 30 minutes before esophagogastroduodenoscopy.
Histological preparations were stained using the Romanovsky-Giemsa method and the SIF reaction was performed. The presence and severity of Helicobacter pylori infection in the gastric mucosa was diagnosed using a cytological study with Pappenheim staining of smears and using a urease test.
Daily pH monitoring was carried out according to the method of V.M. Chernobrovoy, which made it possible to determine the parameters of the GDR: the total number of alkaline casts with pH > 5 during the monitoring period, the number of massive casts, with determination of the number of waves lasting over 5 minutes. Based on the data obtained, the total percentage of time with a pH level > 5 and pH < 2 was calculated.
An endoscopic examination of patients with NAH and hypertension revealed a number of macroscopic changes: atrophy of the mucous membrane in hypertension, changes in the relief (nodular, lumpy), inflammatory changes in the mucous membrane, incl. erosive, the presence of focal hyperplasia, polyps, xanthomas. A study of the frequency and severity of atrophic changes in the gastric mucosa in patients with hypertension showed that most often atrophic changes in the gastric mucosa were observed in the antrum (100.0%), in the body they were detected in half of the patients (51.5%) and much less often in the cardiac department (23.8%).
In a comparative analysis of data from the studied groups, it was found that the severity of macroscopic atrophic changes in the gastric mucosa gradually increased from group I to group III, that is, with an increase in the severity of atrophic processes in the gastric mucosa, there was an aggravation of morphological changes in the mucous membrane (the appearance of intestinal metaplasia and dysplasia).
Nodular gastric mucosa was characterized by the presence of small protrusions of gastric mucosa (protrusions) of various sizes and was usually caused by focal hyperplasia of the integumentary pitted epithelium, which, when combined with atrophy of the mucosa, was a manifestation of atrophic-hyperplastic gastritis. Lumpy mucosa or mucosa in the form of a “cobblestone pavement” - an extreme degree of nodularity with uneven areas of edematous mucosa, separated by deep flat areas, was often a manifestation of atrophic-hyperplastic gastritis, less often - uneven edema of mucous membranes [12].
The nodular relief of the gastric mucosa, predominantly in the antrum of the stomach, was significantly more often detected in patients with hypertension (28.7%, p < 0.05), with a predominance of the frequency of this sign in groups II and III. The nodularity of the mucus was usually combined with morphological hyperplastic changes and/or the presence of intestinal metaplasia of the mucus. Tuberosity of the mucous membrane (mainly in the antrum) was also more often noted in hypertension (20.8%, p < 0.05), mainly in groups II and III of patients.
In groups I and II of patients with hypertension, erosive changes in the gastric mucosa were found (15.1 and 11.4%, respectively). In the vast majority of patients, erosions were acute and localized only in the antrum.
In all groups of patients with insignificant differences in frequency, but with a predominance in group III, so-called polypoid formations of the mucous membrane (focal hyperplasia, etc.) were found, the presence of which correlated with a number of morphological changes: hyperplasia of the surface epithelium (r = 0.22, p < 0.014), dysplasia of the gastric mucosa (r = 0.35, p < 0.001), as well as with an allergic component of inflammation of the mucosa of the same part of the stomach.
Polyps of the gastric mucosa were found only in hypertension in 7 patients (6.9%, p < 0.05), with a significant predominance of their frequency in group III. Polyps were localized with equal frequency in different parts of the stomach (cardia, body, antrum) and were predominantly hyperplasiogenic in structure. The presence of polyps correlated with atrophic changes in the region where the polyp was localized (r = 0.22, p < 0.016), and polyps in the cardiac region correlated with dysplasia of the surface epithelium (r = 0.18, p < 0.05).
QoL was recorded only in patients with hypertension (12.9%, p < 0.05). Their sizes did not exceed 5 mm (from 2 to 5 mm). The frequency of QOL in group I was 7.5%, in group II (AH with intestinal metaplasia) - 14.3%, in group III (AH with dysplasia of the mucous membrane) - 30.8% of cases. If in group I xanthomas were localized only in the antrum, then in groups II and III they were distributed throughout different parts of the stomach. That is, as structural morphological changes in the mucous membrane of a precancerous nature intensified in patients with hypertension, the frequency and prevalence of gastric xanthomatosis also increased.
Correlation analysis made it possible to detect relationships between xanthomatosis and a number of pathological conditions: the severity of atrophy of the gastric corpus mucosa at the macro- and microlevels (r = 0.18, p < 0.05 and r = 0.31, p < 0.001, respectively), the frequency of mucosal hyperplasia stomach (r = 0.32, p < 0.001), polyps (r = 0.37, p < 0.001), the presence of intestinal metaplasia (r = 0.24, p < 0.009) and dysplasia of the gastric mucosa (r = 0 .33, p < .001).
In general, when analyzing the macroscopic state of the stomach, it was found that the increased severity of morphological changes in the mucous membrane of a precancerous nature in patients with hypertension is characterized by an increase in the severity of macroscopic changes in the stomach: an increase in the prevalence and intensity of atrophy of the mucous membrane, the frequency of gastric polyposis, xanthomatosis, and changes in relief (nodularity, tuberosity).
Helicobacter pylori infection was diagnosed in 19.1% of cases with non-atrophic gastritis and in 45.5% with atrophic gastritis. Of the 13 patients with gastric xanthomatosis, Helicobacter pylori infection was detected in 3 cases (23.1%). Correlation analysis did not reveal a relationship between the presence and degree of Helicobacter pylori infection and gastric xanthomatosis.
Correlation analysis of the parameters of daily pH-metry made it possible to establish the dependence of the frequency of gastric xanthomatosis on GHD: the frequency of detection of xanthomas in the antrum directly correlated with the level of minimum pH during the night monitoring period (r = 0.943; p = 0.001), the frequency of detection of xanthomas in the body of the stomach directly depended on the number of alkaline casts over the entire monitoring period (r = 0.468; p = 0.002) and the number of long-term alkaline casts (r = 0.443; p = 0.003).
It is known that endoscopic diagnosis of atrophic changes in the gastric mucosa when using fiber-optic devices often presents certain difficulties [3, 13]. Only with pronounced atrophy of the mucous membrane, when its thinning, the presence of submucosal vessels, excess gastric mucus, and a decrease in the size of the folds are noted, can we diagnose atrophy of the mucous membrane with sufficient confidence. With minimal and moderately expressed atrophic changes in the gastric mucosa, atrophy is indicated by focal pallor, thinning, and variegation of the mucosa. The determination of these changes may not always be objective; it depends on the qualifications and experience of the endoscopist, and on the quality of the endoscopic equipment. The fact that QOL was found only in patients with hypertension may allow us to classify QOL as a marker of hypertension, that is, the diagnosis of xanthomas contributes to the endoscopic diagnosis of hypertension. We analyzed previous endoscopic studies of 13 patients with gastric xanthomatosis. In the protocols of endoscopic studies, only in 1 case the presence of xanthomas was recorded (the study was performed in our institution). The remaining 12 patients were examined in other medical institutions in the region and country. Consequently, this endoscopic finding is usually not recorded by endoscopists and is not reflected in endoscopic reports.
Most endoscopists do not diagnose xanthomas, in our opinion, for two reasons: 1) attention is not paid to these formations, 2) QOL is not visualized due to gastric foaming. The use of an antifoam agent allows you to quickly clear the stomach of foamy mucus and create conditions for a detailed examination, which helps improve the quality of endoscopic examination in general and visualization of micropathology, incl. xanthoma.
In general, our correlation analysis gave grounds to consider QOL an important endoscopic sign: the frequency and prevalence of gastric xanthomatosis increased with increasing morphological changes in the gastric mucosa and correlated with the severity of microscopic atrophic changes in the gastric mucosa of the body of the stomach, with the frequency of polyposis, hyperplasia, intestinal metaplasia and dysplasia of the gastric mucosa, with severity of DGR. At the same time, we have not recorded a relationship between quality of life and Helicobacter pylori infection. Despite the fact that CLs are small-sized formations, the above indicates the importance of diagnosis and the mandatory display of this finding by endoscopists in the endoscopic protocol. Identification of QOL indicates the need for a thorough dynamic endoscopic and morphological examination of patients in order to timely diagnose early gastric cancer.
Thus, the data obtained indicate that xanthomas, which in themselves do not refer to serious structural changes, are an important diagnostic marker or satellite of precancerous changes in the gastric mucosa (atrophy, intestinal metaplasia, dysplasia).
If left untreated
Xanthomas themselves do not pose a health hazard. However, it is important to establish the underlying disease that led to the formation of skin defects. For example, high blood cholesterol can cause the formation of atherosclerotic plaques in blood vessels. And this is the risk of strokes, heart attacks, thrombosis.
Well, you shouldn’t remain silent about the aesthetic side of the issue. Multiple xanthomas can significantly spoil the appearance, which is why the patient develops complexes and social difficulties. But the problem can be solved in one day.
Histological composition
Xanthomatosis. External manifestations
The composition of the pathology is represented by accumulated lipids inside tissue macrophages. They granulate in the area where the blood vessels running inside the skin are located. Typically, the cytoplasm of tissue macrophages is light in color and looks optically empty. If it is stained with Sudan orange, its color becomes bright orange.
Xanthoma cells are localized in the upper layers of the dermis in individual units, small groups, and large-width strands containing layers of connective tissue with a fibrous structure. Touton cells can sometimes be seen. These are huge multinucleated cells that look like foreign inclusions. Lymphohistiocytic infiltration can also be observed.
It is impossible to cure separately. It is necessary to treat or at least correct the underlying disease. If individual elements worsen the quality of life, they are removed surgically, laser or electrocoagulation. Recurrence after surgery is extremely rare. To alleviate the condition of flat xanthoma of the palms or the eruptive variety, you should strictly adhere to a diet, excluding fats, and taking only low-calorie foods.
If the patient has tendon disease, then limit all foods that contain cholesterol and fatty acids. If cholesterolemia is heterozygous, then it is necessary to additionally take bile acid sequestrants, as well as hydroxymethylglutaryl-CoA reductase inhibitors.
Xanthomas: treatment methods
Treatment of xanthoma is carried out in several ways depending on the symptoms, location, size of the formation:
- If pathology is detected on the skin, then the dermatologist’s task is to remove the cosmetic defect.
- If a formation is detected on internal organs, but does not cause symptoms, then medications are prescribed to improve metabolism and lower blood cholesterol.
At the same time, it is recommended to undergo treatment for the underlying disease, which has led to impaired fat metabolism and increased cholesterol levels in the blood. This will help avoid relapses.
There are several ways to remove xanthoma from the surface of the skin:
- The laser method is considered one of the most effective ways to remove formations from the skin. The technology is safe, treatment is comfortable for the patient. The laser beam targets the plaque cells without damaging the surrounding tissue. Healing of the impact site may take 5-7 days. There are no scars or scars left, and the risk of wound infection is very low.
- If the xanthoma is large, your doctor may recommend surgical removal with a scalpel. The wound may take at least 14 days to heal. The disadvantage of this method is the risk of scar formation. And after micro-surgery you need to wear a bandage.
- Liquid nitrogen is often used to remove skin lesions. However, due to the fact that xanthomas most often form in the eye area, this is not the best option on the eyelids.
- The radio wave method can also be used to treat formations of this type. But the method has a number of contraindications.
Laser plaque removal remains the most effective. It is enough to look at the “before and after” photos to be convinced of the high cosmetological effect. The method has virtually no limitations or contraindications.
Classification of xanthoma
There is a considerable variety of xanthoma and each of its types has its own characteristic features. Most often in the practice of a dermatologist at a medical clinic, the following types are encountered:
- flat. Yellowish in color, different sizes. Mainly formed on the eyelids and near the inner corner of the eye;
- tuberous. They look like hard nodules of red-yellow color. Most often appear on the inner surfaces of the knees and elbows;
- tendon. Formed on the tissues of ligaments and tendons;
- eruptive. Papular, painful red-yellow rashes in the buttocks, shoulders and limbs;
- disseminated. They are represented by multiple red-yellow formations in the form of nodules and tubercles that arise in the skin folds;
- verrucous. These are single rashes that usually form in the oral cavity;
- xanthelasma. This is the name given to tumor formations above the skin around the eyes.
Treatment of xanthomas
Once the main diagnosis has been accurately established, all efforts are devoted to its treatment: correction of diabetes mellitus, liver, kidney, and pancreas diseases. Hereditary diseases are the worst to treat, since they cannot be completely eliminated; at best, it is only possible to minimize the leading manifestations.
Drug and surgical treatment
Therapy for xanthomas comes down to normalizing metabolic processes and reducing the concentration of cholesterol and triglycerides in the blood.
For this purpose, statins are prescribed - drugs that have a hypolipidemic effect - they block the synthesis of cholesterol and other lipids.
This group includes products such as liprimar, roseart, and atoris. Other medications that regulate fat metabolism are fibrates (Trykor, Lipantil, Amotril). They enhance the breakdown of lipids and prevent their accumulation in tissues.
Surgical treatment of gastric xanthoma is extremely rare. It is indicated only when the tumor grows to a large size, which leads to disruption of the organ. In such cases, laser plaque removal is performed.
Folk recipes
Among traditional medicines, garlic has the most pronounced lipid-lowering effect. Moreover, the effect persists even when consuming the dried plant. In second place is fish oil, or rather the polyunsaturated fatty acids it contains.
They “displace” harmful fat fractions from the body, and cholesterol levels drop. For the same purpose, increased doses of vitamin C are prescribed. You can drink it in the form of ascorbic acid preparations or get it from food: citrus fruits, rose hips, cabbage.
Be careful! Having thrown all your efforts into the fight against cholesterol, do not forget about the state of the gastrointestinal tract. If xanthomas have formed against the background of atrophic or hyperacid gastritis, then it is better to avoid eating garlic, cabbage and citrus fruits. They can be taken in the form of dietary supplements that do not have a negative effect on the gastric mucosa.
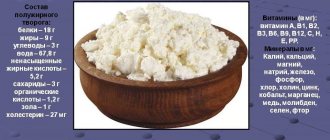
Lipid-lowering diet
Patients with xanthomatosis are recommended to limit the consumption of animal fats (fatty meat, butter, high-fat dairy products), and give preference to their plant analogues: olive, sunflower, flaxseed, sea buckthorn oils. You can eat eggs only in small quantities - no more than three yolks per week.
Simple carbohydrates, which after breakdown can be transformed into fats, are also contraindicated. They are found in sugar, jam, sweets and other sweets. But complex carbohydrates are allowed, found in abundance in cereals, raw vegetables and fruits.
If cholesterol increases, it is necessary to give up not only certain foods, but also bad habits. Smoking and alcohol abuse also lead to lipid metabolism disorders and the formation of xanthomatosis and atherosclerosis.
Stomach xanthomas are not terrible in themselves, but they are an alarming signal indicating that a serious malfunction has occurred in the body. In addition, they act as a marker of the condition of the gastric mucosa. Xanthomas almost never form in healthy tissues. Lipids are deposited mainly in the atrophied mucosa, which requires restorative treatment and a gentle diet.