The term “gastroduodenitis” in medicine refers to joint inflammation localized on the mucous membrane of the stomach and duodenum. The anatomical and physiological features of this digestive zone are so connected that damage to one organ leads to disease of another if left untreated.
Signs of gastroduodenitis necessarily precede peptic ulcer disease. According to statistics, 50% of adults have pathology of the digestive system in the form of gastritis and duodenitis. Over the past two decades, the problem has worsened among young children and schoolchildren. Before finding out what gastroduodenitis is, let's figure out why these diseases occur together.
What features of anatomy and functioning connect the two organs?
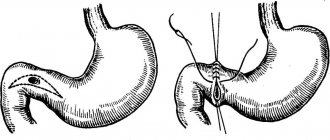
The stomach comes into contact with the initial part of the small intestine in the pyloroantrum through the sphincter. The adjacent part of the duodenum is called the bulb, which is what we are talking about when dealing with duodenitis.
Food that enters the stomach remains for 6–10 hours. This time is required to completely process the contents with gastric juice and move them towards the intestines. In the antrum area there are the necessary glandular cells that produce hormone-like substances (gastrin, pepsin, histamine, acetylcholine).
They stimulate the production of gastric juice under the influence of endocrine and nervous regulation. The inhibitory effect is exerted reflexively by enterogastrines and hydrochloric acid entering the bulb (acid duodenal reflex). As a result, protein substances from food are broken down in the stomach into albumins and peptones.
Some substances are absorbed into the blood already at this stage. The importance of supporting the digestive process in the pyloroduodenal zone is indicated by the massive blood supply, established according to one principle - arteries on both sides. Such vascularization provides the possibility of compensation and replacement in case of thrombosis.
Moreover, in the area below the duodenal bulb, blood enters only from one side (through the vessels of the mesentery). To neutralize the acidic contents of the stomach in the border region of the intestine, it is necessary to reduce the concentration of hydrogen ions by 100 thousand times. In the upper part, the wall of the duodenum is strengthened by three layers of membranes (then only 2 remain).
Mucosal cells produce enterogastron, cholecystokinin, secretin, pancreozymin, enterocrinin, valkinin to counteract hydrochloric acid from gastric juice. In addition, enzymes from bile and pancreatic secretions enter the lower sections.
One of the reasons for digestive failure and gastroduodenitis in patients after gastric resection surgery (tumor, peptic ulcer) is the lack of necessary duodenal hormones
Every 20–26 seconds, due to the contraction of the muscular wall, a circular wave passes through the stomach (in an empty stomach after an hour and a half), promoting the bolus of food to the pylorus. The opening and closing of the canal is regulated by the obturator reflex. The signal comes from the duodenal bulb: if there is an acidic reaction there, the pylorus closes; if it is alkaline, it is open.
The normal throughput of the pylorus is about 3% of the stomach contents per minute. Any failure of a clear mutual connection affects the general process of digestion; gastroduodenitis affects other organs.
What causes gastritis and duodenitis?
The causes and mechanism of development of gastroduodenitis differ depending on the form. Acute inflammation is caused by ingestion of:
- poisonous and toxic substances in case of poisoning (accidental or for suicidal purposes);
- drinking a significant dose of alcohol;
- reaction to spicy seasonings, rough meat foods;
- a type of allergic manifestation to foods, the content of pesticides in vegetables and fruits;
- a stressful state experienced by a person.
Under the influence of these factors, during gastroduodenitis, the secretion of gastric juice sharply increases, the concentration of hydrochloric acid increases, and it is thrown into the bulb. At the same time, local protection drops. In men, acute gastroduodenitis is detected 3 times more often. Up to 70% of cases of gastroduodenitis are chronic forms. The risk increases with age.
Their main reasons:
- development of infection, most often Helicobacter, although damage by salmonella, staphylococcus, and enterobacteria is possible;
- transition from the acute form in the absence of timely and complete treatment of gastroduodenitis;
- violation of the diet, nutritional value of products, women's passion for fashionable diets, vegetarianism instead of the expected result leads to a long period of hunger (acid corrodes its own mucous membrane), lack of protein and vitamins (causes anemia and immunodeficiency);
- frequent consumption of fast food, chips, carbonated water, canned food;
- work, study with constant overload, nervous breakdowns;
- the need for long-term treatment with nonspecific anti-inflammatory and hormonal drugs, uncontrolled use of headache medications containing Aspirin, Paracetamol;
- long-term smoking, alcoholism;
- hereditary predisposition to gastroduodenitis.
The problem is aggravated by the patient’s chronic diseases of the liver, gall bladder, intestines, pancreas, cardiac decompensation, blood diseases, endocrine and nervous systems. More often there is not one, but several causes.
65–85% of cases of chronic gastroduodenitis are caused by Helicobacter pylori
As it turned out, Helicobacter pylori can be present in a person since childhood and “wait” for the right moment to attack. When other factors appear that disrupt the formation of secretions, the regulation of the processes of digestion and movement of food in the stomach and duodenum, and the ability to restore the mucous membrane, Helicobacter “strikes.”
Causes
There are several causes of inflammatory disease, which are divided into two groups:
- endogenous;
- exogenous.
Endogenous causes are the basis for focusing on acid formation, disruptions in hormonal regulation of secretion, and a decrease in the level of mucus formation. A predisposition to gastroduodenitis is observed in patients with the following diagnoses:
- diseases of the biliary tract and liver;
- endocrine pathology.
The most common exogenous etiological factors influencing the development of gastroduodenitis are:
- eating cold or hot, spicy food;
- chemical (exposure to pesticides);
- penetration of the bacterium Helicobacter pylori into the body.
What forms of gastroduodenitis exist?
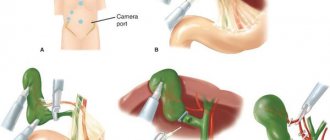
Clinical forms of gastroduodenitis differ little in symptoms. The main classification is determined after a visual examination of the mucous membrane using esophagogastroduodenoscopy and determination of the patient’s gastric acidity.
Superficial gastroduodenitis - most often occurs during acute inflammation, is expressed by thickening and swelling of the folds, hyperemia. Hypertrophic gastroduodenitis - against the background of redness of the mucous membrane, areas with a white coating, pinpoint hemorrhages are visible, the folds are swollen and thickened.
Mixed gastroduodenitis - in addition to the picture of hypertrophy, foci of gray atrophy are detected due to impaired blood circulation, death of epithelial cells, the folds of the mucous membrane in such cases are smoothed.
Erosive gastroduodenitis - typical are multiple erosions (superficial cracks, shallow ulcers), covered with mucus and a film of fibrin. The form is considered closest to peptic ulcer disease.
The type of lesion is determined by the endoscopic picture
Some authors, by analogy with gastritis, add: atrophic, hemorrhagic, gastroduodenitis with duodenogastric reflux. Gastroduodenitis is classified according to the level of acidity:
- with hypersecretion (high acidity) - most cases;
- with normal secretion;
- hyposecretory - reduced secretion is characteristic of atrophic gastritis, a malignant tumor of the stomach.
Up to 40% of cases of gastroduodenitis occur in atypical and asymptomatic forms. During the diagnosis, the attending physician is convinced that the degree of organ damage does not correspond to the severity of the symptoms.
What is superficial gastroduodenitis
Gastroduodenitis is an inflammation of the mucous membrane of the lower stomach (pyloric zone, pylorus) and duodenum.
In the superficial form, only the superficial layer of the mucosa is involved in the pathological process, deep tissues are not affected, and the atrophy process does not occur
Superficial gastroduodenitis is considered the mildest form of the disease, characterized by redness of the mucous membrane and mild swelling.
The main cause of the disease is poor nutrition, namely the abuse of fatty, spicy, and salty foods.
In addition, hereditary predisposition can play a significant role in the development of pathology. Other reasons are bad habits, long-term use of antibiotics, diseases of the biliary tract and liver, Helicobacter pylori, mental and physical overload.
Manifestations
Symptoms of gastroduodenitis in adults depend on the extent of the inflammation process. Based on the pain that bothers the patient, it can be assumed that the stomach or duodenum is predominantly affected.
“Stomach” pain appears almost immediately after eating and is localized on the left side and in the center of the epigastrium. With increased acidity, they are relieved by eating (acid binding occurs). The character is aching and bursting.
Duodenitis is expressed by hunger and night pain
Pain occurs 1.5 hours after eating. Localized on the right side of the epigastrium, in the navel area. Digestive disorders due to gastroduodenitis are manifested by dyspeptic syndrome with sour belching, nausea, heartburn, bitter vomiting, and changes in stool.
In the clinical course there are:
- acute form - if the disease lasts up to three months;
- exacerbation phase in a chronic process;
- incomplete remission lasting no more than two weeks;
- complete remission - in cases where there are no signs of pathology for several years, but when foci of inflammation are detected on gastroduodenoscopy;
- recovery, which is confirmed by examination.
In the acute form, the pain syndrome is much more pronounced, the infection causes a rise in temperature, and general symptoms of intoxication (weakness, dizziness, headaches).
Chronic inflammation with gastroduodenitis occurs in waves, the severity of symptoms is less intense. Patients are concerned about:
Exacerbation of gastroduodenitis
- constant feeling of heaviness and fullness in the stomach;
- aching pain is difficult to associate with lunch or breakfast, can occur after 2.5 hours, is relieved after artificially induced vomiting;
- sometimes the only manifestation is heartburn and belching, they decrease after eating, then bother again;
- appetite is unchanged or increased;
- unpleasant taste in the mouth;
- stool disorders (diarrhea is replaced by prolonged constipation);
- smell from the mouth.
During the acute stage, all signs become more intense. Patients with chronic gastroduodenitis are characterized by changes in character over the years. They are characterized by increased irritability, tearfulness, short temper, and poor sleep. They often become the cause of conflicts in the workplace and in the family.
The plaque is thick, despite the copious secretion of saliva
When examining a patient with gastroduodenitis, the doctor sees the tongue coated with a white thick coating and pale skin. Pain in the area of maximum pain is determined by palpation. There is no tension in the abdominal muscles. You can read about the clinical course of gastroduodenitis in childhood in this article.
Diet and nutrition rules
Without the use of this treatment method, drug therapy will definitely not bring the desired results. Table No. 5 according to Pevzner is used, which indicates what can be eaten with gastroduodenitis and what cannot be eaten. The menu of this table includes lean meats (beef, rabbit), poultry (chicken), vegetables, cereals, and dairy products. A prerequisite is that the preparation of these products is carried out by steaming, stewing is possible.
What is recommended to eat for gastroduodenitis:
- soups cooked in vegetable, mushroom, fish broths, pureed;
- soft-boiled eggs, omelet;
- lean meat (chopped, fried); boiled chicken;
- cutlets, steamed, stewed, fried, but without a rough crust;
- lean ham;
- boiled lean fish, chopped lean herring, pre-soaked, black caviar;
- porridge, boiled or pureed (buckwheat, semolina, rice);
- flour dishes: stale white, gray bread, dry crackers (exclude baked goods);
- vegetables, fruits, boiled, grated raw;
- vegetable and fruit juices;
- tea, coffee, cocoa with water and milk, marmalade, sugar;
- milk (if there is no diarrhea), butter, kefir, yogurt, cream, non-sour sour cream, fresh non-sour cottage cheese, mild grated cheese;
- Do not overuse tea and coffee: they promote the release of hydrochloric acid.
When eating, observe the following rules:
- Food and drink should not be too hot or too cold;
- You should never swallow solid food without chewing it thoroughly.
- It’s better to eat small amounts several times a day.
Proper nutrition consists of eating regularly in small quantities (at least 5 times a day). You can have dinner no later than 2 hours before bedtime.
Diagnostics
In diagnosis, correct assessment of patient complaints is important. The main additional methods are the following. Signs of anemia in a general blood test (decrease in hemoglobin level, number of red blood cells), nonspecific evidence of inflammation in the form of moderate leukocytosis and ESR is possible.
Analysis of stool for scatology reveals digestive disorders (presence of undigested fibers, mucus). Esophagogastroduodenoscopy allows you to visually assess the degree of damage to the mucous membrane of the stomach and duodenum, clarify the form of gastroduodenitis, and take material from the affected areas of the mucosa for biopsy.
It is most convenient to identify the causative agent of inflammation (Helicobacter pylori) using a urea breath test with urea. In acute forms of inflammation, a bacteriological examination is carried out and the infection is cultured. The pH-metry method is necessary to determine the type of gastric juice secretion in order to treat the disease with optimal medications.
Classification
Like any inflammatory disease, there are acute, chronic, and aggravated gastroduodenitis. Chronic gastroduodenitis is the most common; patients usually seek medical help in the acute stage. As a rule, a chronic process is a consequence of an untreated acute one, but the disease is often primary chronic, that is, it initially arises as a chronic disease, occurring with periods of exacerbations and remissions.
Depending on the nature of the pathological process occurring in the mucous membrane of the stomach and duodenum, the following forms of chronic gastroduodenitis are distinguished:
| Hypertrophic | the mucous membrane is hyperemic, in some areas there are hemorrhages (punctate hemorrhages), edematous, covered with a fibrinous-mucosal coating; |
| Surface | with this form, the mucous membrane of the stomach and duodenum is swollen, the folds are thickened; |
| Erosive | the mucous membrane is swollen, hyperemic, contains multiple erosions, covered with fibrinous-mucosal plaque. |
| Mixed form | the mucous membrane as a whole has the appearance of hypertrophic gastroduodenitis, but there are foci of atrophy; |
Depending on the secretory function:
- With reduced secretory function (reduced acidity);
- With normal secretory function;
- With increased secretory function (increased acidity).
The signs of the disease are extremely varied, and the form of their manifestation depends on the nature of the course; in acute gastroduodenitis they are bright, pronounced, but short-lived, in chronic gastroduodenitis they are constant, intensifying during exacerbations.
Treatment
Treatment of gastroduodenitis in adults is impossible without the patient refusing to drink alcohol, smoke, and comply with diet requirements.
Mode and nutrition
It is recommended to normalize mental and physical stress, and be more attentive to the organization of regular rest. You need to eat 5-6 times a day, in small portions and strictly following the schedule.
You will have to stop snacking “on the go” and dry food; food should be served warmed up, but not hot
Ice cream is excluded from the menu; cold temperatures are a stomach irritant. Among the prepared dishes, the diet does not allow everything that contributes to increased secretion of gastric juice. You should not eat anything that causes increased fermentation, mechanical and chemical effects on the mucous membrane. Raw vegetables are allowed only in pureed form.
Irritating foods include: fried fish and meat, smoked meats, pickled and canned vegetables, industrial juices (especially tomato), spices, hot seasonings, sauces, baked goods, fatty dishes, rich broths.
It is better to give up strong coffee and tea, chocolate, carbonated drinks, and choose low-fat dairy products. During exacerbations of gastroduodenitis, all dishes are prepared only in pureed form or from minced meat. The salt content is normal, unless there are contraindications due to other diseases.
Meat and fish are steamed, in the form of cutlets and meatballs. It is recommended to make stews from vegetables, and compotes and jelly from fruits and berries. If the disease occurs without intense pain or heartburn, there is no need for strict mechanical treatment in the diet, but fried foods remain contraindicated.
The diet is expanded as digestion improves. In case of acute gastroduodenitis, table No. 1 is sequentially expanded (first 1 “a”, then 1 “b”). In the chronic course of the disease, the patient will have to forever adapt to strict nutritional requirements.
Is it possible to cure gastroduodenitis only with medications without diet? This question worries people who are not accustomed to restrictions on food and catering at work. Our answer is that no matter how wonderful and expensive medications are prescribed, if there is no sparing of the stomach, a focus of continuous inflammation is created.
The process moves to deeper layers, causes ulcers, stimulates cancerous degeneration of cells
The use of medicinal methods
Since gastroduodenitis is most often accompanied by an increase in acidity, we will dwell in more detail on the treatment of this type of disease. To reduce acidity, drugs of different effects are used:
- Acid binders (antacids) - support the alkalization process, the group includes Almagel A, Phosphalugel, Maalox, De-Nol.
- Blocking synthesis by glandular cells of the antrum - Cimetidine, Omeprazole, Ranitidine.
- Increasing the activity of anti-acid-forming hormones - Gastal.
Antispasmodics - No-shpa, Platiphylline help reduce pain. Patients need to use a maximum of drugs by injection, unless there is a need for direct action on the mucous membrane.
In order to normalize nervous regulation, mild sedatives, infusions of plants, medicinal herbs (motherwort, valerian, ready-made drug Novopassit) are prescribed. To improve the protection of the mucous membrane, the recovery and healing processes, a course of biostimulants is prescribed (Aloe injectables, Actovegin, Solcoseryl).
If reduced acidity is detected in chronic gastroduodenitis, agents are used that stimulate the formation or replace gastric juice (ready-made preparation from gastric juice, Acidin-pepsin, Betacid.
For patients with identified Helicobacter pylori infection, therapy must get rid of the main cause. The treatment regimen includes antibiotics (Amoxicillin, Sumamed) in combination with Metronidazole and drugs based on bismuth compounds.
When identifying infection using the tank method. analysis for acute gastroduodenitis, a full course of antibacterial therapy is prescribed.
During periods of remission, physiotherapy, mud applications from healing springs, and mineral water intake are indicated. This is best done at resorts. Gastroduodenitis, complicating the postoperative period of gastric resection, needs to be monitored by the surgeon in terms of healing time and cause. Not all drugs are suitable for treatment with this option.
Basic principles of treatment
It is necessary to follow the doctor's advice, follow a diet, and take prescribed medications. You should also introduce a protective regime and lead a healthy lifestyle. You can use traditional folk remedies and physiotherapeutic procedures.
Basics of diet therapy for gastroduodenitis
When choosing food products, you must adhere to the principles of gentle effects on the digestive organs. Food should be at normal temperature, not chemically aggressive, not hard. They eat little by little; the diet should be as varied as possible. Have dinner a couple of hours before bedtime. Avoid both overeating and starvation. It is contraindicated to eat dry food.
If an exacerbation begins, then the diet is made more stringent (table No. 1). The diet during such a period is gentle, with a simultaneous increase in the amount of animal proteins consumed. This generally leads to an increase in calorie intake. It is advisable that the body receives 10–20% more calories than usual. For this purpose, the content of vegetable fats in food is also increased. But the amount of carbohydrates should be reduced by one and a half times.
If the condition is characterized by an increased secretion of hydrochloric acid, then baked goods, fatty, including fatty meat, acidic foods, especially juices, berries, coarse fiber (vegetables, fruits of this consistency), carbonated drinks, coffee, spices, chocolate, are removed from the diet. pickled food.
If, on the contrary, the acidity is low, carbonated water, baked goods, canned food, and slimy soups are prohibited. As soon as the condition begins to stabilize, the menu should be expanded, regardless of the type of disease.
Drug therapy
Diagnosis of superficial gastroduodenitis
To treat gastroduodenitis, two groups of drugs are used: antacids, antisecretory agents. Antacids are needed to reduce acidity. The current generation of drugs are non-absorbable; they normalize the condition due to the ability to react appropriately with hydrochloric acid. These include:
- phosphalugel, alphagel (this is an aluminum salt of phosphoric acid);
- tisacid, gastal, maalox (products with magnesium or combining magnesium with aluminum);
- Almagel A, Megalak (preparations that combine not only magnesium with aluminum, but also anesthetics);
- topal, topalkan (magnesium, aluminum, alginate);
- vikalin, gastrfarm;
- talcid, rutacid (aluminum, magnesium with additives, presented in a layered mesh structure)
Antisecretory agents are also very diverse. First of all, these are M-anticholinergics. They have two varieties: selective, non-selective. Non-selective drugs have an aggressive effect on the body, so they are not used to treat gastroduodenitis. Selective agents are pirenzepine, gastrocepin. These drugs suppress the synthesis of hydrochloric acid and reduce the release of pepsinogen. At the same time, blood supply improves and there is a cytoprotective effect.
How to cure gastroduodenitis using folk methods?
Popular recommendations are supported by doctors only for the treatment of the stage of fading exacerbation or remission. You should not try to be treated with herbs during exacerbations. The main purpose of decoctions and infusions is to soothe the mucous membrane, activate local immunity, and blood circulation in the area of inflammation.
Suitable for this:
- chamomile (flowers);
- yarrow;
- oatmeal jelly;
- flaxseed oil and seed decoction;
- plantain juice;
- rosehip compote.
It is necessary to know exactly the effect of plants on acidity in a particular case, so as not to provoke an exacerbation
Simultaneous damage to the initial parts of the digestive tract affects the functioning of other organs. The consequences of an untreated disease can be chronic pancreatitis and cholecystitis. You can’t let the disease progress and violate your doctor’s recommendations.
Prevention
Prevention of the disease is simple and consists of the following:
- nutritious meals at least 4-5 times a day;
- exclusion of fasting, overeating, dry food, snacks on the run;
- moderate physical activity and regular walks in the fresh air;
- timely and correct treatment of all gastroenterological pathologies;
- regular examinations by specialized medical specialists.
At the first signs of the disease, you should consult a doctor and not self-medicate.