- home
- general surgery
- Barrett's esophagus
Barrett's esophagus
- This is a precancerous condition that is asymptomatic and is discovered accidentally during a gastroscopic examination.
Columnar epithelium in the esophagus was first described in 1950 by N. Barrett, who mistakenly interpreted this situation as a congenital shortened esophagus. Further in 1953, P. Allison and A. Johnstone established that the described changes relate directly to the mucous membrane of the esophagus, and are a consequence of the replacement of squamous epithelium with columnar epithelium. Then, in 1970, C. Bremner, in scientific work on animals, demonstrated the occurrence of columnar cell metaplasia of the esophageal epithelium in experimentally induced gastroesophageal reflux, proving the acquired nature of such changes and the connection with hiatal hernia or GERD.
The relevance of this problem is that the probability of glandular cancer in patients with columnar cell (intestinal) metaplasia is 0.5-0.8% per year or 5-8% throughout life.
The prevalence of esophageal metaplasia in European residents, according to various sources, ranges from 2% to 5%. At the same time, in the presence of gastroesophageal reflux disease (GERD) with or without hiatal hernia, columnar cell metaplasia of the esophageal mucosa is diagnosed in 10-15% of patients. Adenogenic cancer of the esophagus, which developed against the background of metaplasia, was first described in 1952 by B. Morson and J. Belcher, and in 1975, A. Naef theoretically substantiated the development of adenocarcinoma from metaplastic epithelium of the esophagus. Esophageal adenocarcinoma is a fatal disease with a five-year survival rate of less than 20%, diagnosed in Russia in late stages. Among patients with Barrett's esophagus, the risk of tumor lesions is 30-120 times higher.
In 1983, D. Skinner, using extensive clinical material, proved the presence of a pathogenetic chain: gastroesophageal reflux - columnar cell metaplasia - adenogenic cancer of the esophagus.
The above considerations force us to consider columnar cell metaplasia of the esophageal mucosa as an important surgical problem that requires a thoughtful approach to solving it.
The use of a correct and modern algorithm in the treatment of gastroesophageal reflux disease, which occurs with the development of columnar cell metaplasia of the esophagus, allows, using surgical endoscopic technologies, not only to achieve a significant improvement in the quality of life of patients, but to prevent the development of esophageal adenocarcinoma.
Causes and symptoms of the disease
Barrett's esophagus is a disease that occurs throughout life, often due to the following factors:
- insufficiency of the lower esophageal sphincter, due to which the contents of the stomach (acidic environment) enter the esophagus;
- double reflux - when gastroesophageal reflux disease (GERD) and duodenogastric reflux disease (DGR) develop simultaneously;
- weakened contractile function of the esophagus;
- increased secretion of hydrochloric acid;
- exogenous factors - smoking, dietary errors, excess weight, alcohol abuse, combination chemotherapy.
The most common forms of pathological changes in the mucous membrane of the esophagus, which can lead to BE:
- Dysplasia is a disorder of the normal structure of the mucous membrane, in which cell aging occurs and the tendency to their uncontrolled division increases. This condition is called precancer, since there is a risk of degeneration into oncology, although small. Moderate and severe degrees of dysplasia are distinguished; in severe cases, the risk of developing BE is higher. If provoking factors are excluded, the disease does not progress.
- Metaplasia - in this condition, the normal mucous membrane of the esophagus is replaced by cells unusual for this zone, most often gastric or intestinal. The condition is persistent, it does not disappear even if risk factors are excluded. There is evidence that with a metaplasia length of 3 cm or more, the likelihood of developing a malignant tumor - adenocarcinoma of the esophagus - is higher.
- Erosive form - the presence of erosions and erosive-ulcerative defects (both acute and epithelial) on the mucous membrane of the esophagus in the lower third (usually in the projection of the transition of the esophagus to the stomach).
Main patient complaints and signs of Barrett's esophagus
- pain during swallowing food throughout the esophagus, behind the sternum or in the epigastrium;
- belching with sour contents, especially after eating, heartburn;
- sore throat that occurs after eating, worsens when bending over, hoarseness of voice;
- dysphagia, when the patient complains that it is difficult or painful for him to swallow food, especially solid food;
- nausea and regurgitation after eating, especially when straining or belching;
- thinning of tooth enamel.
You should not ignore the listed symptoms and put off going to the doctor; it is better to prevent the disease and start treatment in the early stages, because the processes occurring at the cellular level are not reversible.
Prices
| Disease | Approximate price, $ |
| Prices for examinations for stomach cancer | 5 730 |
| Prices for diagnosing Crohn's disease | 3 560 — 4 120 |
| Prices for diagnosing gastrointestinal cancer | 4 700 — 6 200 |
| Prices for hepatitis C diagnostics | 5 700 — 6 300 |
| Prices for treatment of Vater's nipple cancer | 81 600 — 84 620 |
| Prices for colorectal cancer treatment | 66 990 — 75 790 |
| Prices for treatment of pancreatic cancer | 53 890 — 72 590 |
| Prices for treatment of esophageal cancer | 61 010 — 81 010 |
| Prices for treatment of gallbladder cancer | 7 920 — 26 820 |
| Prices for treatment of nonspecific ulcerative colitis | 5 670 |
| Prices for treatment of stomach cancer | 58 820 |
| Prices for diagnosis and treatment of gallstone disease | 9 000 — 11 950 |
| Prices for the treatment of gastroenterological diseases | 4 990 — 8 490 |
| Prices for diagnosing Crohn's disease | 5 730 — 9 590 |
| Prices for treatment of viral hepatitis C and B | 5 380 — 7 580 |
| Prices for treatment of gastrointestinal cancer | 4 700 — 6 200 |
Diagnosis of Barrett's esophagus
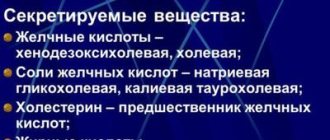
The main and most effective method for diagnosing Barrett's syndrome is endoscopic. Its purpose is to obtain biopsy material. In this case, the morphological study is aimed at:
- confirmation of metaplasia of the esophageal mucosa;
- detection of dysplasia;
- detection of malignant cells, most often adenocarcinoma.
To determine more precise boundaries of the changed mucosa during endoscopic examination, chromoscopy is used; this is the coloring of the mucosa. Lugol's solution is usually used; if you are allergic to iodine, use methylene blue or acetic acid.
Classification
Depending on the location of metaplastic changes, Barrett’s esophagus is divided into three groups:
- Metaplasia in the long segment of the esophagus; about 1% of all pathologies occur in this zone. This type is typical for men aged 55-65 years.
- Metaplasia in the short segment zone, corresponding to a distance of no more than 3 cm from the stomach to the esophagus.
- Localization in the cardiac zone of the esophagus; This is where Barrett's syndrome develops in most cases, but malignancy is less common than in the area of the long segment of the esophagus.
Treatment of Barrett's esophagus
The following treatment methods for Barrett's esophagus are used:
- Medication . Conducted by gastroenterologists. Antacids that reduce acidity, prokinetics that stimulate motility and the movement of food through the gastrointestinal tract, and proton pump inhibitors are often prescribed.
- Endoscopic . And here the endoscopist has a large choice, it all depends on the volume of the lesion, the severity of dysplasia, the depth of invasion (penetration) and other factors.
- argon plasma coagulation;
- endoscopic resection (dissection) of the mucous membrane;
- endoscopic ablation of the esophageal epithelium with a bipolar electrode;
- photodynamic therapy;
- cryodestruction;
- laser ablation.
- Surgical . To prevent the development of Barrett's esophagus, a Nissen fundoplication is performed. The essence of the operation is that a cuff is made around the esophagus from the bottom of the stomach, which should prevent the reflux of stomach contents into the esophagus.
Another commonly used and very radical method is removal of the lower part of the esophagus.
Columnar cell metaplasia of the esophagus
Metaplasia is a process of incomplete regeneration when, as a result of prolonged action on tissue by damaging factors (chemical, thermal, mechanical), it is replaced by another differentiated tissue that is not characteristic of a given anatomical structure, but is more adapted to withstand the action of damaging factors.
Thus, with prolonged action of refluxate on the esophageal mucosa, the squamous cell epithelium is transformed into a more stable columnar cell epithelium. Thus, metaplasia is based on compensatory and adaptive processes that protect the organ from destruction. Metaplastic tissue is highly differentiated and is not dangerous in terms of tumor development. But metallized tissue cannot be completely normal, since it develops in an anatomically unusual place. Often there are foci of dysplasia.
Dysplasia is a changed type of tissue. Dysplasia is characterized by an increase in polymorphism of cells and nuclei, mitotic activity, and disruption of cell orientation in tissues.
This process is not accompanied by any clinical symptoms.
Prevention
There is no specific prevention for Barrett's syndrome.
Timely diagnosis and treatment of gastroesophageal reflux disease, regular and timely visits to a gastroenterologist, examinations and consistent follow-up help prevent its development.
- For dysplasia of the esophageal mucosa, FGDS control with biopsy is required once every 6 months.
- For metaplasia - FGDS control once a year.
After effective conservative and surgical treatment of Barrett's esophagus, all patients should undergo annual endoscopic examination with epithelial biopsy.
Answers to questions from patients with Barrett's esophagus
Can Barrett's esophagus be cured?
Barrett's esophagus is a precancerous condition; if a patient with such a diagnosis has completed the necessary course of treatment, regularly visits a doctor to monitor the situation, and follows all his recommendations, then the likelihood of a cure is very high. This disease, especially in the early stages, responds well to treatment, provided that it is prescribed individually by a competent specialist and is carried out comprehensively. The complex must include all the necessary methods - medication, dietary, endoscopic and surgical. Thus, to completely cure Barrett's esophagus, the joint efforts of the treating physician and the patient are necessary.
How to treat Barrett's esophagus?
In the treatment of Barrett's esophagus, the most important factor is the timely detection of pathology. If the patient undergoes regular examinations, the doctor will be able to detect the disease at an early stage. After effective treatment, the risk of possible malignant cell degeneration will be virtually eliminated.
Treatment is carried out comprehensively and, depending on the specific situation, includes both surgical and conservative methods. The therapeutic program is compiled individually for each patient, taking into account the characteristics of his body and clinical picture. As a result, the risk of further development of pathology and complications that are dangerous to the patient’s life is eliminated, his well-being improves, and his quality of life increases.
If the situation allows only conservative treatment to be prescribed, the patient must be prepared to carefully follow the prescribed medication regimen for a long time (from 3 months to 2 years). In addition, for the success of treatment, a certain correction of the patient’s diet and lifestyle will be required - immunity-strengthening procedures, reasonable dosing of work and rest, weight loss, giving up bad habits (alcohol, smoking, chocolate, soda, tea, coffee).
Many patients, on the recommendation of a doctor, immediately undergo a session of radiofrequency ablation (RFA) of the esophageal mucosa, during which dosed destruction of the altered mucosa is carried out during gastroscopy. As a result of this procedure, the metaplastic epithelium is replaced by normal mucosa. The duration of conservative drug treatment is shortened several times.
If the disease has developed against the background of hiatal hernia and has already entered a stage requiring the use of surgical treatment methods, our clinic uses laparoscopic methods, which are not only effective, but cause a minimum of trauma, and therefore are quite easily tolerated by the patient.
The goal of a complex of surgical and conservative methods is to minimize the risk of cancer and restore the mucous membrane of the esophagus. Also, surgical treatment is prescribed if conservative treatment does not bring the expected results.
How long do people live with Barrett's esophagus?
If treatment is successful, which is most of the time, patients diagnosed with Barrett's esophagus live normal lives.
That is why it is important to identify the disease at an early stage and follow all the recommendations of your doctor. It is not the syndrome itself that is life-threatening, but its complications. Unfortunately, the number of patients with esophageal cancer increases every year. Treatment of esophageal cancer is only surgical and is accompanied by a long and very voluminous surgical intervention with removal of the entire esophagus and plastic surgery with the stomach.
How often does Barrett's esophagus develop into cancer?
Barrett's esophagus differs from ordinary chronic diseases in that the degeneration of cells can become malignant at any time. A seemingly calm disease can suddenly turn into esophageal cancer. Moreover, the oncological process is characterized by rapid development.
Currently, world medicine is noticing a significant increase in the number of patients suffering from esophageal cancer, which is a consequence of advanced Barrett's esophagus. The probability that this syndrome will develop into cancer, according to the World Health Organization, varies in different countries, from 0.5% to 10%. Considering that in our country people tend to pay insufficient attention to their health and attribute alarming symptoms to malaise, the likelihood that the disease will be diagnosed in the later stages and the process of cell degeneration will take on a malignant nature is inclined towards higher numbers.
Therefore, at the slightest suspicion of Barrett's esophagus disease, it is necessary to consult a highly qualified specialist. You can also always write to my personal email: [email protected]
Localization of Barrett's esophagus in the gastroesophageal junction
Visual picture during endoscopy, variants of the mucosa in Barrett's esophagus
Visual image during endoscopy, length of mucosal lesion in Barrett's esophagus
What is allowed to eat with this pathology?
It must be said that not everything is as sad as it might seem. In fact, it is not the products that matter, but the dishes that are prepared from them. So, in case of pathology, the following foods and dishes are allowed to be consumed:
- Yesterday's wheat bread, which is slightly dried along with crackers, dry biscuits, marshmallows and marmalade.
- Puree soups, first courses of well-boiled and pureed vegetables.
- Butter with milk, yogurt and cottage cheese.
- Kefir is not prohibited for a diagnosis of Barrett's esophagus, but it can cause heartburn in some people, so you should be careful with it.
- Vegetable oil, and in addition, viscous porridge cooked in water with the addition of a small amount of milk. Rice, buckwheat, semolina and non-instant oatmeal porridges are suitable for this.
- Chicken along with veal and rabbit. Occasionally, you can cook lean varieties of beef, and also introduce milk sausages (preferably the highest grade) into your diet.
- Boiled eggs, as well as river fish.
- Boiled potatoes along with beets, carrots and non-acidic fruits and berries.
Complications
Replacing esophageal tissue with single-layer columnar epithelium can cause a number of serious complications, including:
- Transformation of foci of metaplasia into malignant neoplasms. The most common form of esophageal cancer is adenocarcinoma.
- Hemorrhagic syndrome localized in foci of metaplasia and damage to the esophagus.
- The appearance of peptic-type strictures. These are adhesions of connective tissue that narrow the lumen of the esophagus at their location and provoke the development of dysphagia, which consists in disrupting the process of swallowing food.
To prevent such complications, it is important to diagnose metaplasia in time and receive appropriate treatment aimed at reducing the size of the lesions and their number.
Forecast
The concept of columnar cell metaplasia includes a wide range of changes: from lesions without dysplasia to initial forms of cancer. Consequently, the treatment and prognosis of these forms will be different.
Even the size and number of lesions do not always determine the prognosis of the disease. Multiple foci of metaplasia with highly differentiated, although altered, tissue may remain stable for many years, and a single foci with undifferentiated tissue may require urgent surgery.
A good prognosis of the disease is observed in the case of complete remission of GERD and the absence of histological signs of dysplasia. A poor prognosis is a high degree of dysplasia against the background of persistent reflux. For a long time, the presence of complete and incomplete intestinal metaplasia (which differs from complete intestinal metaplasia by the presence of gastric cells in the biopsy specimen) on a long segment was considered a bad prognostic sign (but even this sign is now not recognized by all scientists).
And between these polar states there are a lot of other states. Therefore, it is possible to say unambiguously what the prognosis of the disease is only by looking at a specific case.
Of course, the first question that worries all those who get sick is: “How long can they live with this?”
Here it should be remembered that columnar cell metaplasia is not cancer, but only an increased likelihood of its development, therefore, with adequate treatment and dynamic monitoring of the condition of the tunica mucosae of the esophagus, most patients continue to lead a normal life and live to a ripe old age.