Causes of disturbances in the formation of the gastrointestinal tract in the fetus, statistics
Anomalies in the structure of the gastrointestinal tract are associated with a violation of embryogenesis at the stage of 4-8 weeks of pregnancy, when the opening of the digestive tube is formed. Initially, it ends at both ends, but by the end of the 8th week, channels are formed, and the mucous epithelium closes the lumen of the intestinal tube. Among the most common pathologies are stenosis (narrowing or stretching of the walls) or atresia (fusion).
The duodenum suffers the most, which is due to the peculiarities of its embryogenesis. 1/2 of cases are accompanied by defects of other internal organs - heart, blood vessels, rectum, liver, stomach. Some cases are so severe that the baby will have to undergo many operations during his lifetime, and they will not guarantee his normal existence.
Abnormalities of the gastrointestinal tract are visible on ultrasound at 11 weeks. Ultrasound diagnostics is not a 100% guarantee that the baby will have serious abnormalities, so its results are the basis for a more detailed examination of the woman.
A pregnant woman undergoes karyotyping to detect chromosomal abnormalities. She also undergoes an amniotic fluid test, and based on the results of the examination (if they are bad and the diagnosis is confirmed), she is recommended to terminate the pregnancy
Intestinal pathologies
Anomalies of the duodenum include:
Atresia.
Occurs in 1 case out of 10,000. It consists of complete intestinal obstruction due to pathological fusion of the walls of the organ. In 37% of cases, it is accompanied by other anomalies - cauda equina, fusion of the cervical vertebrae, asymmetrical position of the ribs, etc.
In another 2% of cases, intestinal atresia is accompanied by esophageal atresia, anal hygroma, incomplete rotation of the stomach, etc. This is mainly typical for a fetus with chromosomal abnormalities, in particular with trisomy 21.
90% of pregnancies end in miscarriage or failure to thrive during the first 2 trimesters. The remaining 10% of pregnancies with duodenal pathology result in the birth of children suffering from various defects: 31% have airway obstruction (blockage by a foreign body such as a cyst, tumor), 24% have facial nerve paresis (impaired functionality of facial muscles).
Only 1% of children lead a relatively normal life after undergoing a complex operation, provided there are no chromosomal abnormalities.
Intestinal membrane
. This is a film that blocks the intestinal lumen, resulting from a violation of the growth of the inner layer of the duodenum. Occurs in 1 case out of 40,000. On ultrasound it is visualized as a weakly echogenic formation. The intestinal lumen is narrowed by several millimeters, the contours of the mucous membrane are clear.
Pathology is not an indication for termination of pregnancy. Depending on the location of the membrane, it is removed after the birth of the baby using duodenotomy (opening the intestinal lumen and then removing the membrane). Malrotation.
It consists of a violation of the normal rotation and fixation of the duodenum. If the midgut has made a full rotation on the blood-feeding pedicle, this can lead to cessation of blood supply and death of the midgut.
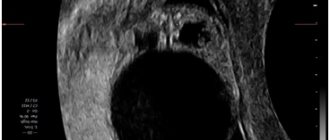
Prenatal diagnosis can be made from 24 weeks, and polyhydramnios was observed in 61.5% of pregnancies. Ultrasound reveals an anechoic double-buble 3 consequence of dilatation of the intestine and stomach.
Although even a slight expansion at 16-22 weeks should cause alarm. Normally, the duodenum is visible on ultrasound only from 24 weeks. Additionally, in 62% of cases, malformations of the heart, genitourinary system, and other gastrointestinal organs are detected in the fetus. After karyotype testing, chromosomal abnormalities are detected in 67% of cases, of which Down syndrome ranks first. Stenosis.
It is detected in 30% of newborns, mainly in boys. This is a partial obstruction of the duodenum, localized in one place. It is mainly observed in the upper sections and is accompanied by anomalies of the pancreas. It is clearly visible on ultrasound from 24 weeks when using the Doppler method to study intestinal blood flow.
Stenosis is successfully eliminated and has more favorable prospects than atresia. Does not require termination of pregnancy. Megaduodenum
.
This is an increase in the size of the duodenum to a size that sometimes exceeds the size of the stomach. Occurs in 1 case out of 7500. It may be a consequence of an annular pancreas, when the head of the organ encircles the intestine in a ring, or atresia or stenosis of the duodenum. Diagnosed by ultrasound at 24 weeks. The upper part of the abdominal cavity is very swollen, while the lower part is sunken. Hyperechogenicity of the intestine.
The higher the density of the tissue being examined, the greater the echogenicity. On ultrasound, the echogenicity of the fetal intestine should be lower than that of bones, but higher than that of porous organs such as the liver, lungs or kidneys. When the echogenicity of the intestine is equal in density to the echogenicity of bone tissue, they speak of hyperechogenicity.
Pathology is detected no earlier than 16 weeks. It indicates a deviation in the development of the fetus. Increased echogenicity occurs with premature aging of the placenta, internal infections, discrepancy between the size of the fetus and the gestational age, endocrine disease cystic fibrosis, intestinal obstruction (stenosis).
An ultrasound scan should be performed in several different clinics to avoid specialist errors. Only when the diagnosis is finally confirmed, the woman is sent for a more detailed examination - biochemical screening, analysis for TORCH infections, cordocentesis and amniotic fluid analysis. The final diagnosis is made on the basis of a comprehensive analysis, and not just an ultrasound examination. Diverticula (cysts).
They have different names - duplication cysts, double colon, enterogenous diverticulum. It consists of budding from the intestinal walls of a formation during the embryonic period. They form not only in the intestines, but throughout the gastrointestinal tract from the larynx to the anus.
It is believed that the cause of bifurcation of the walls is a violation of the blood supply to the fetal digestive tube. Cysts on ultrasound are hypoechoic and can be either single-chamber or multi-chamber. The walls of the cysts are two-layered and have increased peristalsis, and are hyperechogenic if they contain blood.
Intestinal cysts are visualized in the 2nd trimester and are often combined with other pathologies. The accuracy of visualization of intestinal cysts in the fetus is 66.6%. This pathology is not an indication for termination of pregnancy, because in uncomplicated cases it is operated on and eliminated. Abnormalities in the shape, size, position and mobility of the intestine. By the 2nd trimester of pregnancy, it should turn around the mesenteric artery counterclockwise by 2700. If embryogenesis is disrupted, the following pathologies can be distinguished: lack of rotation, failed rotation and incomplete rotation.
On ultrasound, with anomalies of intestinal rotation in the fetus, polyhydramnios and dilation of intestinal loops without peristalsis are noted. In case of intestinal perforation, myconium peritonitis occurs - infection due to the release of intestinal contents. The pathology is detected late, only in the 3rd trimester, which requires immediate preparation of the woman for delivery.
Screening for detection of congenital fetal diseases during pregnancy
Category: Reminders for the public.
Screening during pregnancy is a whole range of studies that allows parents and doctors to obtain the most complete information about the health of their unborn baby. Screening reveals many congenital and physical characteristics. How and when is screening done during pregnancy?
What is screening during pregnancy and why is it done?
Screening during pregnancy is a set of examinations that includes ultrasound and biochemical analysis of venous blood for hormones. As a rule, screening is carried out three times - in the first, second and third trimester.
Early detection of pathologies is very important. This makes it possible to begin treatment of genetic diseases as early as possible and, if not completely cure them, then at least relieve the symptoms as much as possible. If during the examination the doctor notices any abnormalities, the pregnancy is monitored especially carefully, which makes it possible to prevent the development of complications or premature birth. If the detected pathologies turn out to be too severe and incompatible with life, the doctor will refer the patient to terminate the pregnancy for medical reasons.
Screening during pregnancy is harmless for both mother and baby. This is a fairly accurate study, although it should be clearly understood that it does not provide a 100% guarantee. The accuracy of screening depends on many factors - the professionalism of the researchers, the woman’s compliance with the rules for preparing for the examination, and other factors.
First screening during pregnancy
The first screening during pregnancy is carried out between the 11th and 13th weeks. There is no point in undergoing this examination earlier - until the 11th week of pregnancy, many indicators are practically impossible to determine.
The study includes two medical tests - an ultrasound and a blood test.
Ultrasound
Using an ultrasound, the doctor determines the exact duration of pregnancy, evaluates the child’s physique, its size (head circumference, length of limbs, height), the functioning of the heart muscle, the symmetry of the brain, the volume of amniotic fluid, the structure and size of the placenta, as well as the condition and tone of the uterus. For each of these parameters there are normal indicators with which the doctor will compare the results. For an 11-13 week pregnancy these norms are:
- CTP (coccygeal-parietal size, that is, the length of the fetus from the crown to the coccyx) is 43–65 mm. If this figure is higher than normal, it means the child will be large. A deviation to the smaller side indicates slow development (the reason for this state of affairs is often a hormonal imbalance or infectious diseases suffered by the expectant mother), genetic pathologies or fetal death (in this case the heart will not be heard). However, this may also be due to a banal error in determining the timing of pregnancy.
- BDP (biparietal size, that is, the distance from temple to temple) - 17–24 mm. A high BDP means a large fetus, but only if all other indicators indicate the same. Otherwise, we may be talking about a brain hernia or hydrocephalus. A low BDP indicates slow brain development.
- TVP (thickness of the collar space) - 1.6–1.7 mm. Deviation from this norm (TVP above 3 mm) is considered a sign of some severe chromosomal pathologies - Down syndrome, Edwards syndrome, etc. However, one should not panic ahead of time - no one will make such a serious diagnosis only on the basis of TVP. To confirm, you need to take a blood test for hormones and do a biopsy of the outer dense membrane of the embryo for subsequent research.
The length of the nasal bone is 2–4.2 mm. A nasal bone that is too small may indicate a pathology or simply that the baby will have a snub nose. HR (heart rate) - 140–160 beats per minute. A slight (up to 40 beats per minute) deviation in one direction or another is considered normal.
The size of the chorion, amnion and yolk sac. The chorion is the outer membrane of the fetus, which will eventually become the placenta. If it is located on the lower wall of the uterus, they speak of chorion presentation. This is a potentially dangerous situation that can lead to miscarriage, in which case bed rest is recommended for the pregnant woman.
Amnion is the inner membrane that holds amniotic fluid. The normal volume of amniotic fluid at 11–13 weeks is 50–100 ml.
The yolk sac is an embryonic organ that, in the first weeks of the fetus’s life, plays the role of some internal organs that will be formed later. By the time of the first screening, the yolk sac should practically disappear (then the examination form will indicate “not visualized”). If its size is about 6 mm, then the fetus may have certain pathologies.
Cervix. Normally, its length at the time of the first screening is 35–40 mm. A shorter cervix means a risk of premature birth.
Ultrasound is performed in two ways - transabdominal, in which the ultrasound machine sensor is located on the abdomen, and transvaginal, in which it is inserted into the vagina. Transvaginal ultrasound provides more complete and accurate information, but is usually performed only in the first trimester. This method is usually used when examining overweight women, since the fat layer in the abdominal area does not allow a detailed examination of the fetus and uterus.
It is necessary to prepare accordingly for an ultrasound. Before a transabdominal ultrasound, it is advised to drink about a liter of water so that at the time of the examination the bladder is full - then the uterus will shift slightly towards the abdomen and the picture will be clearer. With a transvaginal ultrasound, the degree of bladder fullness does not matter at all, but before the examination it is better to go to the toilet - it will be more comfortable. Before the examination, you need to take a shower or freshen up with wet wipes. The accumulation of gases can distort the results of ultrasound, no matter what method it is performed. Therefore, expectant mothers suffering from flatulence are advised to take anti-flatulence medications the day before the examination and not eat anything that produces gas.
Blood analysis
Biochemical screening, also called a dual test, is done to determine the level of two hormones (hence the name) - free b-hCG and PAPP-A.
- b-hCG (human chorionic gonadotropin) begins to be produced from the first days of pregnancy. Its amount gradually increases until about the 9th week, and then begins to gradually decrease. On average, for a period of 11–13 weeks, 50,000–55,000 mIU/ml is considered normal. An elevated level of hCG may indicate a multiple pregnancy, or, in the worst case, genetic pathologies of the fetus or the presence of diabetes mellitus in the mother. Reduced hCG is typical for frozen pregnancy, ectopic pregnancy, fetal death, or certain malformations (Patau syndrome and Edwards syndrome).
- PAPP-A is plasma protein A. The maintenance norm for a period of 11–13 weeks is 0.79–6.01 mU/l. Low PAPP-A is a sign of chromosomal pathologies such as Down syndrome and Edwards syndrome, fetal death and miscarriage, fetal malnutrition (underweight) and preeclampsia.
- High PAPP-A is a sign of multiple pregnancy, large fetal size or low placenta.
In order for the blood test to provide the most accurate information, it must be taken on an empty stomach, at least 8 hours after the last meal. 2-3 days before the test, you should refrain from fried, fatty, spicy, smoked foods, chocolate, nuts, and seafood. It is also recommended not to have sexual intercourse. All this is not so significant, but it can affect the result in one way or another.
Second screening during pregnancy
The second screening during pregnancy is carried out at 16–20 weeks. Like the first one, it consists of the same two stages - ultrasound and blood tests.
Ultrasound
This time, the doctor determines not only the size, but also the position of the fetus and its bone structure, the condition of the internal organs and the place of attachment of the umbilical cord, as well as the volume of amniotic fluid. Here are the approximate basic indicators of the norm for a period of 16–20 weeks:
- BPR - 26–56 mm.
- DBC (femur length) - 13–38 mm.
- KDP (humerus length) - 13–36 mm.
- OG (head circumference) - 112–186 mm.
AFI (amniotic fluid index, that is, the volume of amniotic fluid) - 73–230 mm. Oligohydramnios can negatively affect the condition of the child’s bone structure and the development of his nervous system.
Localization of the placenta. There is some risk only when the placenta is located on the anterior wall of the uterus - with such a localization, placental abruption is possible.
Umbilical cord. One of the most important parameters is the location of the umbilical cord attachment. Marginal, split or membrane attachment is fraught with fetal hypoxia and difficulties during childbirth; it often becomes an indication for cesarean section. The umbilical cord is supplied by 2 arteries and 1 vein, although sometimes only one artery is present. This can cause fetal hypoxia, heart defects, disturbances in the child’s cardiovascular system, and cause low body weight in the baby. However, if all other tests and examinations do not show deviations from the norm, there is no need to worry.
Cervix. The length of the cervix at this stage should be 40–45 mm. A short cervix means a risk of miscarriage.
Visualization. Unsatisfactory visualization can be caused both by the position of the fetus or the excess weight of the expectant mother, as well as by edema or hypertonicity of the uterus.
Blood analysis
As during the first screening, during the second a blood test is taken for b-hCG, and the level of free estriol and AFP is also checked. Here are the norms for their maintenance at 16-20 weeks of pregnancy:
- b-hCG - 4.67-5-27 ng/ml.
- Free estriol is a hormone, the level of which can be used to judge the condition of the placenta. The normal range is 1.17–3.8 ng/ml. Elevated estriol is typical for multiple pregnancies or a large fetus. Reduced - for the threat of miscarriage, placental insufficiency, anencephaly and Down syndrome.
- AFP is a protein produced in the fetal gastrointestinal tract. The norm is 15–27 U/ml. A slightly lower AFP may mean that the gestational age was determined incorrectly (slightly underestimated). If the AFP is very low, the cause may be Edwards or Down syndrome, the threat of miscarriage or fetal death. High AFP is characteristic of neural tube pathologies, esophageal atresia, and Meckel's syndrome. High AFP is also possible in women who have had an infectious disease during pregnancy.
Third screening during pregnancy
The third screening during pregnancy is carried out at 30-43 weeks. Based on the results of this screening, the doctor decides on the need for a cesarean section or the possibility of a natural birth. The basis of the third screening is the same ultrasound. Sometimes Doppler sonography is prescribed - a study of the functioning of blood vessels. Here are the approximate norms for this stage of pregnancy:
Ultrasound
- BPR - 67–91 mm
- DBK - 47–71 mm
- WPC - 44–63 mm
- Exhaust gas - 238–336 mm
- IAZh - 82-278 mm
The thickness of the placenta is 23.9–43.8. A placenta that is too thin is not a particularly dangerous deviation from the norm. The reason may be the woman’s miniature physique, infectious diseases she has suffered, or hypertension. An excessively thick placenta is a sign of anemia, diabetes, and Rh conflict. An indicator such as the degree of maturity of the placenta is also taken into account - at a period of 30–35 weeks, the 1st degree of maturity is considered normal. If the placenta thickens and ages too quickly, premature birth, fetal hypoxia and slow development are possible.
Prenatal screening is very important and should not be neglected. Timely identified pathologies and deviations from the norm can save the life and health of your child. This is worth remembering, especially for those parents who refuse an examination for fear of finding out that the baby’s development is not going according to plan.
Liver pathologies in the fetus
The liver is visualized by ultrasound examination already at the 1st screening. At 11-14 weeks, a hypoechoic formation in the form of a month can be seen in the upper part of the abdominal cavity. By week 25, echogenicity increases and becomes the same as that of the intestine, and before birth it exceeds the density of the intestine.
Assessing the state of liver blood flow is very important. The fetal umbilical cord vein enters the liver, and in the 2nd trimester the portal vein is visualized. Its diameter is normally 2-3 mm, and by childbirth it increases to 10-11 mm. Bile ducts should not normally be visualized in the fetus. One of the most common pathologies of the fetus is hepatomegaly of the liver - an increase in the size of the organ. To detect anomalies, a 3D sensor is used that can visualize the slice in longitudinal, transverse and vertical sections. You can also see an increase in the size of the liver on a regular ultrasound machine through a protruding tummy, the coverage of which significantly exceeds the norm.
At the same time, various hyperechoic inclusions are visible on the screen. As a rule, the anomaly is complemented by an enlarged spleen.
Among the reasons leading to an increase in the size of the digestive organs are hidden infections (toxoplasmosis, syphilis, chickenpox), as well as chromosomal mutations (Down, Zellweger, Beckwet-Wiedemann syndromes).
- With Zellweger syndrome, abnormalities of the limbs, distortion of the chest, and kidney cysts are visible. Analysis of amniotic fluid reveals a deficiency of dihydroxy-acetone-phosphate acyl-transferase.
- Chickenpox, herpes, and cytomegalovirus cause calcification of hepatic vein thrombi, which is reflected on the ultrasound monitor screen as hyperechoic round calcifications. They are also formed during meconium peritonitis - poisoning with the contents of the fetal intestines, which enters as a result of damage to the walls.
In 87.5% of cases, the cause of liver enlargement and the formation of calcifications is intrauterine infections. Also, most pregnant women are diagnosed with hyperechoic intestines, changes in the structure of the placenta, and a large spleen. Pathology in the 3rd trimester occurs in case of Rh conflict between mother and child. Metabolic disorders are also possible. Liver enlargement occurs with galactosemia (a genetic disorder of carbohydrate metabolism, due to which galactose is not converted into glucose), trypsinemia (lack of production of the digestive hormone trypsin), methylmalonic acidemia (lack of conversion of D-methylmalonic acid into succinic acid), and disorders of urea excretion. Single large hyperechoic inclusions are much better than multiple scattered formations in combination with other pathologies. In almost 100% of cases, large hyperechoic inclusions are eliminated before the baby is born or in the first year of life. In some cases, abdominal organ defects are diagnosed incorrectly. This happens if the baby’s abdominal cavity is compressed by the walls of the uterus, myometrial pathologies or other factors.
The monitor screen shows a pseudoomphalocele - an erroneous visualization of the exit of the abdominal organs beyond the abdominal wall. Sometimes ultrasound does not “see” significant defects. Thus, a hernia in shape and echostructure resembles intestinal loops; in this regard, Doppler ultrasound is of great help, allowing one to see the blood flow.
Our clinic has an excellent 4D device, equipped with all modern capabilities that eliminate diagnostic errors.
Fetal development by week in the first trimester
The conception of a child occurs during the period of ovulation, after the fertilization of the egg by the sperm. As a rule, ovulation coincides with days 10-16 of the menstrual cycle.
Human intrauterine development is divided into two stages: embryonic and fetal. The first stage is the period from the moment of fertilization of the egg to the tenth week of pregnancy.
During the embryonic stage, important processes occur: crushing and implantation of the embryo into the uterine cavity, the formation of the neural plate (the rudiment of the central nervous system) and its closure into the neural tube, the formation of organs and the placenta.
It is worth distinguishing between embryonic and obstetric stages of pregnancy. The first is counted from the moment of conception, the second - from the beginning of the last menstruation. As a rule, the difference between these periods is two weeks.
It turns out that the formation and ontogenesis of the embryo begins only in the third week of pregnancy. Let's take a closer look at how the fetus develops week by week during the first trimester.
3rd week of gestation
After the sperm penetrates the egg, a zygote is formed - a diploid cell with a set of chromosomes equally obtained from female and male gametes. The duration of formation of a diploid cell is 25-30 hours.
The zygote begins dividing and moving towards the uterus. At the beginning of division, the zygote splits into 2-4 blastomeres (round-shaped cells that form the embryo). The number of blastomeres increases every day.
On the fourth day after conception, the zygote consists of 12-14 blastomeres. The density of embryonic cells increases, and they are closely connected with each other. The embryo enters the uterine cavity.
A blastocyst is formed (an early stage of embryo development), which is implanted into the endometrium of the uterus. During implantation, a pregnant woman may experience uterine contractions and spotting, which is often mistaken for menstruation. However, unlike menstruation, bleeding during implantation is mild and short-lived.
4 week
Implantation accelerates the development of the embryoblast (internal cells of the embryo), resulting in the formation of extra-embryonic organs:
- chorion is a membrane that performs excretory, respiratory and protective functions. After implantation of the embryo, the first chorionic villi begin to appear on its surface. Subsequently, some of the chorion cells destroy the uterine wall and participate in the formation of the placenta;
- amnion is a water membrane that provides the fetus with optimal development conditions and protects it from mechanical stress. Amnion fluid consists of proteins, sugars, mineral salts and other substances;
- the yolk sac, which performs a hematopoietic function. At first, its size exceeds the size of the embryo. After the 12th week of gestation, this temporary organ decreases in size and completely disappears.
The formation of the primary intestine occurs. The organs of the digestive system will subsequently develop from its departments. In the fourth week of gestation, the formation of the liver and pancreas occurs.
After implantation of the embryo into the uterine cavity, placenta rudiments form at the site of attachment of the embryo. The process of its formation will be completed by the 16th week of gestation. The placenta provides the fetus with the necessary oxygen and nutrients, protects against infections, and removes metabolic products.
By the end of the fourth week of gestation, a woman notices that the expected menstruation does not occur. During this period, mood swings, fatigue, and increased sensitivity of the mammary glands may occur.
5 week
By the fifth week, the neural tube appears - the basis of the spinal cord and brain. The heart forms from the bulge in the central part of the fruit. During this same period, hemoglobin begins to form, so the rate of iron consumption by the embryo increases.
The umbilical cord begins to form, which will become the connecting link between the embryo and the placenta. As the fetus grows, the umbilical cord also increases in size.
During this period, a woman may experience the first signs of toxicosis: nausea, vomiting, intolerance to certain foods and odors.
week 6
The embryo’s heart begins to beat, and the thymus gland, which is responsible for immunity, is formed. Formed:
- rudiments of arms and legs;
- cerebral hemispheres;
- eye sockets and ear canals;
- organs of the excretory system.
Vessels are actively growing, blood circulation is established.
week 7
Nerve fibers, esophagus, stomach, and pharynx develop. The embryo develops semblances of hands and primary germ cells. The pancreas begins to produce insulin. The respiratory system is currently represented only by the trachea.
A woman may experience increased signs of toxicosis, so it is important to drink plenty of fluids.
8 week
This period is characterized by the formation of facial features in the embryo, as well as the development of the lower and upper limbs. The retina forms in the eyes, the upper limbs are able to bend at the elbows, and the lower limbs at the knees.
The genitals acquire a characteristic appearance, but this is still not enough to determine the sex of the unborn child.
Week 9
Left and right atria and ventricles appear in the heart. Large blood vessels and endocrine glands develop. The placenta begins to produce hormones. The fingers on the lower and upper extremities are fully formed.
10 week
If the genotype of the embryo contains a gene that initiates the development of the male body, then in the tenth week of gestation the testicles actively develop and they begin to produce the hormone testosterone.
At the same time, the fetus develops the optic nerve, and urine begins to form in the kidneys. The strength of bone tissue increases. The diaphragm forms between the abdominal and thoracic cavities.
11 week
From the 11th week the fetal period of intrauterine development begins. The state of health of most pregnant women stabilizes: the symptoms of toxicosis, irritability, and fatigue disappear.
The fetus has formed the most important organs, the face, and the hemispheres of the brain. Muscle tissue develops. The fetus begins to make movements, but the woman does not feel them yet.
12 week
Taste buds on the tongue are formed. The cerebellum is actively developing - the part of the brain that is responsible for performing targeted movements, their speed and maintaining muscle tone. The rudiments of nails and teeth appear.
The thymus gland is a full-fledged organ in which T-lymphocyte differentiation occurs. The body proportions of the fetus are still incorrect: the head is large, the arms are long, and the legs are short and bent at the knees.
The intestines enlarge and begin to fold into loops. Leukocytes appear in the blood, which protect the body from external and internal pathogenic agents.
The formation of the gonads continues. By the end of the 12-13th week of pregnancy, it becomes possible to determine the sex of the fetus.
Stomach
At 16-20 weeks, the fetal stomach is visualized as an anechoic formation of a round or oval shape in the upper abdominal cavity. If the stomach is not filled with amniotic fluid, then we can talk about esophageal atresia (complete absence of lumen).
With a diaphragmatic hernia, the stomach is displaced and also cannot be detected on an ultrasound. Also, amniotic fluid is absent when the central nervous system is damaged in the fetus. If the fetus swallows blood along with liquid, hyperechoic inclusions are visualized in the stomach. They are also seen in stomach tumors, but they are usually accompanied by other malformations. The size of the organ increases with intestinal obstruction, polyhydramnios, thickening of the walls, and absence of the lesser curvature. A decrease in the size of the stomach is typical of microgastria, which occurs due to the absence of a bladder or abnormal position of the liver. In 52% of cases, the fetus dies before the 24th week of pregnancy, and the child is born non-viable. A slit-like stomach is characteristic of underdevelopment in the early stages of pregnancy. This pathology is corrected after the baby is born: a stomach is constructed for the child from part of the small intestine. The operation is extremely complicated, but the anomaly is not an indication for an abortion. Gastric atresia is characterized by the absence of echoshadow and involves the formation of a film with or without an opening located across the walls of the stomach. If this is an isolated pathology, then in 90% of cases it is eliminated surgically. But usually gastric atresia is combined with fusion of the esophagus, ascites (excessive accumulation of fluid), and underdevelopment of the lungs. Gastric agenesis involves the complete absence of the organ. This is typical for severe chromosomal abnormalities that cause fetal death during the prenatal period. Ultrasound at week 22 is of great importance in diagnosis. some abnormalities disappear on their own, while others require immediate intervention.