Published: 07/30/2021 12:45:00 Updated: 07/30/2021
Gilbert's syndrome is the most common form of hereditary pigmentary hepatosis, characterized by impaired bilirubin metabolism due to a genetic defect in microsomal liver enzymes. Often the disease is asymptomatic for many years, but under the influence of provoking factors intermittent jaundice, dyspeptic and asthenovegetative disorders can occur.
Diagnosis requires collecting a family history, laboratory and instrumental studies. In the treatment of Gilbert's syndrome, medications of different groups are used.
Gilbert's syndrome according to the ICD corresponds to code E80.4. Men suffer from this disease four times more often than women. In general, the prevalence of pathology in European and Asian countries does not exceed 5%.
General information
There are many diseases that are manifested by increased levels of bilirubin - this is a bile pigment (component of bile), which is formed during the breakdown of hemoglobin and myoglobin (proteins containing heme).
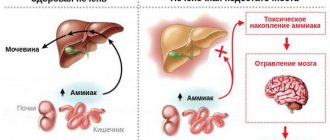
Among such diseases can be called Gilbert's syndrome (ICD-10 code E80.4). During the day, the body produces 200-450 mg of bilirubin, which is present in the blood in two forms - indirect (formed in the amount of 250 mg during the daily breakdown of red blood cells) and direct (formed in the liver by binding and excreted in bile). Indirect bilirubin, entering the liver cells, binds to glucuronic acid under the influence of an enzyme. Its combination with glucuronic acid becomes soluble in water, so it easily passes into bile and is excreted in feces, some in urine. Indirect bilirubin is toxic, direct bilirubin is less toxic because it binds to glucuronic acid in the liver (it is also called bound). The key in the process of binding bilirubin is the liver enzyme glucuronyltransferase, with a deficiency of which indirect bilirubin does not bind in the liver and its level in the blood increases (bilirubinemia).
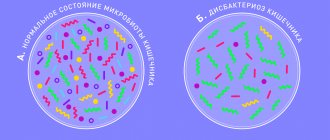
Gilbert's syndrome, what is it in simple words? This is a hereditary disorder of bilirubin metabolism, which is associated with a deficiency or decrease in the activity of glucuronyl transferase. The disease belongs to the class of enzymopathies. A mutation in a certain gene A(TA) 7TAA causes enzyme deficiency and impaired bilirubin uptake, resulting in impaired conjugation of indirect bilirubin and an increase in its level in the blood - benign bilirubinemia due to unconjugated bilirubin. An increase in its level in the blood promotes accumulation in tissues and this explains jaundice. To put it in very simple words, Gilbert's syndrome is a periodically occurring moderate icteric discoloration of the skin, sclera of the eyes and oral mucosa.
Photo showing yellowing of the sclera
Benign (functional) hyperbilirubinemia , which includes Gilbert, Crigler-Nayjar, Rotor, Meulengracht syndrome, are congenital enzymopathies without pronounced changes in the structure of the liver, without signs of hemolysis and cholestasis .
Gilbert's syndrome is characterized by high prevalence - every tenth inhabitant of the globe suffers from it. The ratio of men to women is 3:1. The disease refers to hidden metabolic defects that appear from 3 to 13 years, but mainly in adolescence. The latent form does not manifest itself with any symptoms and is detected by chance during examination. There is a “congenital” version of the syndrome (manifestations develop at 12-30 years of age) and Gilbert’s syndrome, in which clinical manifestations manifest after acute viral hepatitis .
The manifestation of the congenital variant of the disease occurs after physical stress, errors in diet, diseases associated with fever (ARVI, influenza), as well as after mental stress and fasting. The intensity of jaundice in any variant of the disease during an exacerbation is low. In this article we will take a detailed look at Gilbert's disease: what it is, how to treat it, what dangers may be associated with it, and how to prevent exacerbations.
Treatment of pathology
Treatment of Gilbert's syndrome involves reducing physical and psycho-emotional stress, diet therapy and drug support. To lower the level of bilirubin in the bloodstream, a comprehensive therapeutic approach is required.
The doctor recommends not going to the gym, giving up alcohol, limiting time spent in the open sun, and also stops taking hepatotoxic drugs.
The athlete must strictly control the load, otherwise progression of the disease cannot be avoided. It is regularly required to undergo preventive examinations to analyze the activity of the pathological process. Even during remission, sports activities should be carried out in a gentle manner.
Another contraindication for young men with Gilbert's disease is military service. According to the order of the Ministry of Defense, the place and conditions for its holding are separately specified for conscripts. The army and sports can be present in a man’s life, but in a strictly limited volume and with a specially selected regime.
Medication
To reduce the amount of pigment in the bloodstream, you must take the following medications:
- enzyme inducers, such as phenobarbital, zixorin, whose action is aimed at reducing the amount of bilirubin;
- sorbents (atoxyl, polysorb) necessary to accelerate the excretion of pigment in feces.
For preventive purposes, to prevent exacerbation of pathology, the following are recommended:
- hepatoprotectors (Essentiale, Karsil) to protect liver cells;
- choleretics (allochol) stimulate the formation of bile;
- cholekinetics (holosas) have a choleretic effect and facilitate outflow;
- B vitamins
Of the physiotherapeutic procedures, preference is given to phototherapy, which helps reduce the yellowness of the skin. Another possible method of influencing pathology is unconventional treatment. The folk approach involves taking decoctions based on choleretic plants, as well as using herbal baths. The recipe may include rose hips, corn silk, milk thistle, calendula and immortelle.
Diet for Gilbert's syndrome
In case of exacerbation of the disease, a diet is prescribed that corresponds to table No. 5. Meals should be fractional (up to six times a day), in small portions. Every day you should drink at least one and a half liters of liquid (non-acidic compotes, herbal tea, rosehip decoction).
The prohibited list of foods includes fatty, fried foods, hot spices, legumes, sorrel, coffee, soda, baked goods and chocolate. Daily calorie content should not exceed 2800 kcal. Vegetable fats, low-fat fish, milk and vegetables (pumpkin, potatoes, carrots) are recommended.
Dishes must be pureed and served warm.
Example of table menu No. 5:
| Eating | Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | Sunday |
| Breakfast | protein omelette, porridge (rice), optional with milk, with 5 g of butter, weak tea with a slice of lemon | meat cutlets with milk sauce, fresh salad (apples/carrots, grate), weak coffee with milk | low-fat cottage cheese with 60 gr. sour cream, light tea, oatmeal with milk | tea with milk, pasta, ground beef | light coffee with milk, homemade cottage cheese, buckwheat without milk | weak tea, meat cutlets, buckwheat (boil) | light tea, rice, a piece of herring soaked in milk |
| Lunch | cottage cheese casserole | apple | baked apple | lazy dumplings | apple | carrot puree, apple jam | rosehip decoction |
| Dinner | vegetable soup (mash vegetables), soufflé (boiled meat), carrots (stew), compote | potato soup, berry jelly, piece of boiled fish | piece of boiled chicken, side dish (boiled rice), vegetable soup, compote of ground dried fruits | cabbage rolls, a glass of jelly, vegetable soup (grind potatoes) | pasta, borscht in water, jelly, soufflé (boiled meat) | compote, curd pudding, milk soup with noodles | pasta, soup (cereals, vegetables), milk sauce, steamed meat cutlets, compote |
| Afternoon snack | tea with cookies | rosehip decoction with cookies | fruits | kefir | tea with jelly cookies | cookies, kefir | |
| Dinner | vermicelli with cheese, still mineral water | buckwheat, still mineral water | steamed fish cutlet, mashed potatoes, rosehip broth, milk sauce | tea, cheese, rice milk porridge with 6 gr. oils | piece of boiled fish, mashed potatoes, fresh vegetable salad, mineral water | semolina porridge with milk, mineral water | steamed protein omelette, mineral water, cheesecakes |
Is homeopathy effective?
Treatment for Gilbert's disease may include homeopathy. Hepel is often prescribed. The drug has a hepatoprotective effect, protects liver cells from the aggressive effects of environmental factors.
In addition, homeopathy has choleretic, anti-inflammatory and antispasmodic effects. The drug is produced in tablet form for sublingual absorption (under the tongue). It is prescribed to restore liver function in cases of cholestasis, cholecystitis, cholelithiasis and hepatitis.
Contraindications include individual intolerance to the components of the drug. The tablet should be dissolved three times a day half an hour before meals.
Pathogenesis
The process of binding bilirubin in the liver cell is complex and disturbances at any stage affect the development of the disease. The role of the liver in the metabolism of bilirubin is primarily to capture it from the blood by liver cells and deliver it inside the hepatocyte using transport proteins and the enzyme bilitranslocase. Deficiency of this enzyme, which controls the uptake and transport of bilirubin into the liver cell, leads to impaired uptake of bilirubin by hepatocytes and is important in the pathogenesis of the disease. Inside the hepatocyte, bilirubin must be transferred to microsomes, within which it binds to glucuronic acid. Another enzyme is responsible for this transfer - glutathione-S-transferase , the deficiency of which will impair delivery to microsomes.
Finally, the enzyme glucuronyltransferase transports glucuronic acid to bilirubin for binding within microsomes. The deficiency of this main enzyme is associated with mutations in the UGT1A1 gene—in patients, the gene has one extra TA repeat. As a result of such a mutation, enzyme activity decreases by 10-30%. Impaired binding of indirect bilirubin in the liver leads to an increase in its level in the blood - hyperbilirubinemia , the visual manifestation of which is jaundice.
Prognosis and prevention
The prognosis of the disease at any age is favorable.
Hyperbilirubinemia in Gilbert's syndrome persists for life, but is benign in nature, is not accompanied by progressive changes in the liver and does not affect life expectancy. Source of statistical data: Visual pediatric gastroenterology and hepatology: textbook. allowance — Kildiyarova R. R., Lobanov Yu. F. 2013. — 124 p. : ill. (Chapter 6. Liver diseases (vmede.org).
Author:
Pugonina Tatyana Alekseevna, Therapist
Classification
According to flow options, there are:
- Dyspeptic.
- Asthenovegetative.
- Icteric.
- Latent.
In the dyspeptic variant, the following come to the fore: nausea, possible vomiting, heartburn , pain in the right hypochondrium. The asthenovegetative variant occurs with severe weakness, fatigue, headaches, insomnia , sweating , anxiety , and discomfort in the heart area. With the icteric variant, icteric discoloration of the skin of the face, palms, feet and sclera appears, while the color of urine and feces is not changed. In persons with heterozygous status, a latent form of the disease is observed, which manifests itself only during stress tests (test with fasting, taking phenobarbital , administration of nicotinic acid ).
30% of individuals with the homozygous type of gene carriers have high levels of bilirubin and severe clinical manifestations with jaundice of varying severity. The first episode of jaundice appears after overwork or excessive physical activity, most often at puberty, which is associated with an increase in the level of sex hormones. The disease is characterized by a certain seasonality - from February to July. The surge in exacerbations in February is associated with acute respiratory diseases, and at the beginning of summer - with increased insolation, which causes increased pigment formation. Patients are characterized by a decrease in the detoxification function of the liver.
Why is Gilbert's syndrome dangerous? In general, the disease has a favorable course and is not complicated by liver cirrhosis . Gilbert's syndrome is relatively dangerous, since dysfunction of the biliary system may worsen, chronic cholecystitis , duodenitis and gastroesophageal reflux disease . This syndrome is also dangerous because cholelithiasis may develop. Gilbert's syndrome is often combined with other hereditary diseases (Ehlers-Danlos and Marfan syndrome). These patients have an increased risk of developing adverse reactions when taking certain medications.
In accordance with the schedule of illnesses, which contains health requirements for conscripts, the army is not contraindicated for young men with Gilbert's syndrome, they are not given a deferment, and they are not discharged. However, the soldier needs to organize appropriate conditions: good nutrition and lack of excessive physical activity. But in a military unit it is difficult to fulfill these requirements. These medical prescriptions can be fulfilled while serving as a soldier at headquarters. But people with this disease are denied study at military universities.
An inherited disorder of pigment metabolism is also noted in Crigler-Najjar syndrome , which occurs in two variants. Crigler-Najjar syndrome type I is associated with the absence of glucuronyl transferase in liver cells. It is characterized by intense jaundice, which occurs in the child from the first days of life. The level of indirect bilirubin is 15-50 times higher than normal and there is no direct fraction of bilirubin. Prescribing phenobarbital for this type is ineffective. The disease occurs with bilirubin damage to the brain nuclei and can be fatal. Liver transplantation is the only treatment option.
Crigler-Nayjar syndrome type II is associated with a decrease in enzyme activity, therefore the intensity of jaundice is less than in the previous case and, accordingly, indirect bilirubin is increased no more than 20 times and its direct fraction is determined. An important feature is the good response to treatment with phenobarbital . The development of bilirubin encephalopathy is very rare. In terms of prognosis, type II disease is more favorable.
Main causes of the disease
The main reason for the development of Gilbert's syndrome is a hereditary mutation of a gene that is located on the second chromosome and is responsible for the synthesis of a specific enzyme called glucoronosyltransferase. This biologically active compound is formed in liver cells and is a stimulator of the interaction of free bilirubin with glucuronic acid, as a result of which the resulting complex leaves the body without problems.
A decrease in glucuronosyltransferase in the blood serum to 80% of the required amount is a prerequisite for the enzyme to stop performing its direct function and, accordingly, to transform unconjugated bilirubin into a bound form.
To understand the mechanism of development of the disease, it is important to understand that the yellow pigment bilirubin appears in the blood as a result of the destruction of red blood cells that have existed for 120 days. The fat-soluble substance (unconjugated bilirubin) is transported to hepatocytes, where it is converted into a water-soluble form under the influence of the enzyme glucuronosyltransferase. After this, bilirubin accumulates in the gallbladder and, together with bile, takes part in digestion at the level of the small intestine. Having fulfilled its main function, this compound leaves the body naturally.
With glucuronosyltransferase deficiency, unconjugated bilirubin ceases to accumulate in liver cells and therefore continues to circulate in the blood. During the life of the body, the substance accumulates in the bloodstream in large quantities, causing hyperbilirubinemia. This condition is characterized by bilirubin intoxication and toxic effects on internal organs.
For a person to develop the disease clinically, he must receive defective genes from both parents. The syndrome does not develop if altered hereditary material is received on only one side. But such people are capable of transmitting the mutagen to their children and thereby contributing to the spread of pathology among the population.
Causes
The cause is a genetic disorder, and provoking factors include:
- Infections, colds.
- Emotional and physical stress.
- Vomit.
- Errors in diet and fasting.
- Drinking alcoholic beverages.
- Drug loads ( ampicillin , chloramphenicol , glucocorticoids, vitamin K , caffeine , paracetamol , rifampicin , anabolic steroids, androgens , salicylates ).
- Various operations.
- Trauma.
- Excessive influence of insolation.
- Premenstrual syndrome.
- Poor sleep, lack of sleep.
Gilbert's disease: treatment
Gilbert's syndrome is not a reason to prescribe any specific treatment. A nutritious, high-calorie diet with sufficient fat content is recommended. Drinking alcohol is prohibited, emotional and physical stress, and taking medications that can induce jaundice should be avoided. With frequent episodes of hyperbilirubinemia, phenobarbital is used to treat patients with Gilbert's syndrome, which is prescribed at 0.05-0.1 g 2-3 times a day for 1-2 weeks. Typically, after 7-10 days, the level of bilirubin in the blood decreases to normal.
Symptoms of Gilbert's syndrome
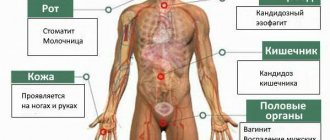
As we found out, the main symptom of Gilbert's syndrome is yellowness of the skin. The triad of symptoms that was initially described by the author: “liver mask” ( jaundice ), xanthelasma of the eyelids , the frequency of occurrence is distinguished by Gilbert’s disease. Symptoms and treatment depend on bilirubin levels.
As for the yellowness of the skin, it is moderate, has a lemon tint, there is a slight yellowness of the mucous membrane of the mouth, palate and more pronounced yellowness of the sclera. Particular attention is paid to coloring the face, ears, feet, palms, armpits and nasolabial triangle. Jaundice can be constant or intermittent, which is more common and appears when bilirubin rises to 50 µmol/l.
Other symptoms include general weakness, fatigue, sweating , irritability, emotional lability, sleep disturbance. Less common are belching, bitterness in the mouth, bloating, heartburn , nausea, and loss of appetite. Patients become sensitive to cold and often develop goose bumps. When examining a patient, a moderate enlargement of the liver and spleen is sometimes revealed. The latent form does not appear for a long time and can be identified by conducting provocative tests.
These episodes are accompanied by weakness, increased fatigue, emotional lability, dyspepsia (discomfort and unexpressed pain in the right hypochondrium, epigastric region). It is also possible that there are no complaints and/or visual manifestations of the disease at all. The presence of bile acids in the blood may not be accompanied by jaundice.
What complications can there be?
The disease is dangerous due to its complications, which arise as a result of the toxic effect of free bilirubin on internal organs. Some scientists do not regard Gilbert's syndrome as a full-fledged disease, calling it a collection of certain symptoms. But this is far from true. This nosological unit has its own characteristics, cause of development and characteristics, which allows us to call it a separate disease.
Hyperbilirubinemia leads to toxic damage to many internal organs, which as a result lose their function. This condition is most dangerous for the structures of the central nervous system. With Gilbert's syndrome, patients often complain of deterioration or loss of memory, impaired physiological reflexes, and mental disorders.
Tests and diagnosis of Gilbert's syndrome
How is Gilbert's syndrome diagnosed? If you suspect this disease, there is a certain algorithm:
- Diagnosis of all patients begins with examination and clarification of complaints and causes that provoke the manifestation of jaundice.
- General clinical examinations include a clinical blood test. With this disease, in 30% of cases, patients have high levels of red blood cells and increased hemoglobin (160 g/l or more), in 15% - mild reticulocytosis . An increase in hemoglobin is associated with its excessive synthesis under conditions of increased bilirubin in the blood and tissues.
- Biochemical blood test, including: total bilirubin and its fractions, liver transaminases, total protein, alkaline phosphatase , albumin , cholesterol and triglycerides . These studies diagnose the type of jaundice and the functional state of the liver, including its protein-forming function. The results of studies in patients indicate an increase in total bilirubin (it ranges from 21 to 51 µmol/l and sometimes an increase to 85-130 µmol/l is recorded). An important indicator is an increase in the content of the indirect bilirubin fraction (most often a moderate increase of 18.8-68.4 µmol/l). Liver function tests were unchanged.
- Ultrasound of the abdominal organs - minor changes in the liver are possible.
- Conducting provocative tests.
- The determining factor in diagnosis is a genetic analysis for Gilbert's syndrome, which objectively confirms or excludes the diagnosis. Genetic analysis is based on determining the mutation of the UGT1A1 gene, which encodes the glucuronyl transferase . This gene is located on chromosome 2. Venous blood is taken for analysis and a direct DNA diagnosis of the gene is carried out. A mutation in the promoter region of this gene is manifested by an increase in the number of TA repeats (normally there are 6); if there are 7 or 8 of them on both chromosomes, the functional activity of the enzyme decreases. In homozygous carriers of the mutation, the syndrome occurs with higher levels of bilirubin, severe manifestations, and they are more likely to have cholelithiasis or bile sludge. Heterozygous carriers have a latent form of the disease, but even carriage in this variant requires changes in lifestyle and a more serious attitude towards the choice of medications taken. Homozygous for a trait is a carrier who has the same allelic genes (AA, OO or aa, oo) on both homologous chromosomes. If these alleles are different (AO, ao), this is a heterozygous carrier.
You can get tested for Gilbert's syndrome in many medical laboratories: Hemotest, Invitro, Optimum, DNAcom, CityLab, turnaround time is 10 days. The price of analysis for Gilbert's syndrome varies in different laboratories and ranges from 3300-4610 rubles. You can keep an eye out for promotional offers when the price is halved.
Genetic analysis is important in order to know the possibility of transmitting Gilbert's syndrome to offspring. In the case where both parents suffer from this disease, all their children will also be sick. If one parent is a carrier and the other is healthy, then half the children will be healthy and half will be affected. If one parent is a carrier of the gene and the other is sick, then the child has a 50% chance of having the disease.
How is the disease determined?
The most important methods for diagnosing Gilbert's syndrome are laboratory tests, including:
- general blood and urine tests - there is an increased number of immature red blood cells and slightly decreased hemoglobin in the blood, bilirubin may be present in the urine;
- biochemical blood test - sugar level may be slightly reduced, protein content is within normal limits, ALT and AST are within normal limits, negative result of thymol test;
- blood test for bilirubin - the total content is increased due to an increase in indirect bilirubin;
- blood test for coagulation - no abnormalities;
- analysis for markers of viral hepatitis is negative.
- Serum iron and other blood iron tests are possible.
In addition, the patient must undergo a liver ultrasound to exclude the possibility of other liver pathologies. The size of the liver may increase slightly during periods of exacerbation. Molecular genetic testing of venous blood is rarely performed due to its high cost, but it can identify defective DNA that is the cause of Gilbert's syndrome.
To confirm the diagnosis, stress tests are performed:
- with fasting - with complete fasting or with caloric restriction, the level of free bilirubin increases 2-3 times;
- with phenobarbital - after five days of taking the level of free bilirubin decreases;
- with nicotinic acid - intravenous injection of the drug increases the level of free bilirubin by 2-3 times;
- with rifampicin - administration of the drug leads to an increase in the amount of bilirubin.
To exclude chronic hepatitis or cirrhosis, a liver puncture may be prescribed.
Hyperbilirubinemia in newborns
The term hyperbilirubinemia refers to any increase in the level of bilirubin in the blood above normal. Taking into account the differences in indicators in newborns who were born at different times, hyperbilirubinemia in full-term newborns is considered when the OB level is more than 256 µmol/l, and in premature ones - more than 171 µmol/l. In newborns, direct and indirect bilirubin ; therefore, two types of hyperbilirubinemia : free (or unconjugated) and associated (synonymous with conjugated).
Hyperbilirubinemia code according to ICD-10 is P59. Any hyperbilirubinemia leads to the development of jaundice, but associated bilirubinemia is a pathological condition. Jaundice syndrome in children occurs under various conditions. Jaundice of the newborn period often requires emergency measures, since indirect bilirubin is a neurotoxic poison, especially in prematurity and in a state of hypoxia. Such children are at risk of central nervous system damage (bilirubin encephalopathy).
There are various types of jaundice in newborns, which are caused by physiological pathological reasons.
Physiological hyperbilirubinemia is a moderate transient (transient) increase in unconjugated bilirubin that occurs in the neonatal period. Hyperbilirubinemia can occur in every newborn, but 50-70% manifest as jaundice (more common in premature and immature newborns).
Physiological jaundice is characterized by:
- Appears after 36 hours of a newborn’s life.
- The peak increase in total bilirubin in a full-term baby occurs on the 3-4th day and on the 5-6th day in a premature baby.
- The child's condition does not suffer: he is active, has a good sucking reflex, normal temperature, there are periods of sleep and wakefulness, the liver and spleen are not enlarged, urine and feces are normally colored.
- A decrease in indicators by the 14th day in a full-term baby and by the 21st day in a premature baby.
Physiological jaundice has no cure, but children should receive exclusive breastfeeding, which helps to overcome jaundice faster. The child should suck often and for as long as he wants, at any time of the day and at least 8-12 times. In the vast majority of cases, jaundice in newborns is physiological, but pathological jaundice must not be missed.
Pathological jaundice has the following features:
- Appears during the first day or is detected on the feet and palms immediately after birth.
- Possible appearance on the 7th day.
- The rate of increase in OB is 85 µmol/l/day.
- The condition of the newborn is unsatisfactory, pathological symptoms are present.
- Enlarged liver and spleen.
- Discolored stool (or dark urine).
- Prolonged jaundice without a tendency to decrease - after the 14th day of life and the 21st day, respectively, in full-term and premature infants.
Pathological hyperbilirubinemia can be caused by various conditions and diseases, including:
- Caused by increased production of bilirubin (these are so-called hemolytic jaundices) in hemolytic disease of the newborn, drug hemolysis , polycythaemic syndrome , ingestion of maternal blood, hemoglobinopathies .
- Arose against the background of polycythemia .
- Developed during infectious diseases.
- Conjugation: hereditary functional bilirubinemia (Gilbert, Arias, Crigler-Nayjar syndromes), metabolic disorders, impaired bilirubin conjugation in intestinal obstruction and pyloric stenosis .
- Caused by drugs or toxins.
- Caused by immaturity of the liver (for example, late onset of conjugation, when the AB count of the indirect fraction increases).
- Mechanical jaundice due to abnormal development of the biliary tract, bile thickening syndrome, familial cholestasis , cystic fibrosis , compression of the biliary tract by various formations.
Among congenital functional bilirubinemias, Gilbert's syndrome ranks first. In newborns, this disease is similar to transient jaundice. The child has hyperbilirubinemia for a long time, but there are no other pathological changes, and there are no cases of kernicterus.
Diagnosis is made based on family history. Prescribing phenobarbital gives good results. The prognosis is favorable. Apparently healthy parents in whom the syndrome is latent may give birth to a child with this syndrome. In this regard, if there have been cases of the disease in the family, the parents need to undergo a genetic examination.
In terms of time of manifestation and severity, the first place is occupied by Crigler-Nayjar syndrome type I. This is congenital familial non-hemolytic jaundice associated with the complete absence of the enzyme glucoronyltransferase , necessary for the conjugation of bilirubin. With this syndrome, liver function is normal, there is no hemolysis and Rh conflict. This syndrome manifests itself in the first days of life with a significant increase in unconjugated bilirubin (up to 400-450 mg/l) and severe kernicterus: muscle hypertonicity , nystagmus , suppression/absence of the sucking reflex, hypotension , convulsions , lethargy .
Clinically, jaundice is noted. Unconjugated bilirubin can reach a concentration of fecal urobilinogen of no more than 100 mg/l. The use of phenobarbital has no effect. The prognosis is very poor, children rarely live beyond 1.5 years.
Crigler-Nayjar syndrome type II proceeds favorably, since the activity of the enzyme glucoronyltransferase is only reduced and liver function is not impaired. The level of unconjugated bilirubin ranges from 60-250 mg/l, especially high in the first months of life, and bilirubin encephalopathy can be observed. There was a positive response to treatment with phenobarbital.
Hemolytic disease of newborns develops when the blood of mother and child is incompatible according to the Rh factor or blood groups. The disease can occur in icteric, edematous and anemic forms. Edema is the most severe and often children are not viable. The icteric form is more favorable, but can also threaten the health of the newborn. In mild cases (indirect bilirubin level less than 60 µmol/l), conservative treatment is carried out. For moderate to severe hemolytic disease, a replacement blood transfusion may be required, and photo and infusion therapy is used before the procedure.
Jaundice in hemolytic disease is either congenital or appears on the first day of life. It has a pale yellow tint, constantly progresses and symptoms of bilirubin intoxication (CNS damage) appear. The liver and spleen are enlarged, the color of feces and urine does not change. Damage to the central nervous system develops when the level of indirect bilirubin is more than 342 µmol/l; for premature and extremely preterm infants this figure is almost 2 times lower. The depth of damage to the central nervous system also depends on the time of exposure of bilirubin to brain tissue.
To prevent hemolytic disease of newborns, women with Rh-negative blood and with group 0(I) are carefully observed, their level of Rh antibodies is determined, and, if necessary, they are delivered early. All women with Rh negative blood are given anti-D globulin . In cases of obstructive jaundice in newborns, various surgical operations are performed to remove obstacles to the outflow of bile.
Factors provoking the development of the syndrome
Today there are a number of factors that are likely to provoke an exacerbation of Gilbert's syndrome or its exacerbation:
- Frequent consumption of fatty foods.
- Alcohol intoxication or regular drinking of alcoholic beverages.
- Long courses of treatment with antibiotics, non-steroidal anti-inflammatory drugs, uncontrolled use of anabolic steroids and the like.
- Treatment with hormonal drugs.
- Strict diets, fasting, refusal to drink water.
- Surgical interventions of varying complexity and localization, medical manipulations.
- Exhausting physical work, intense physical training.
- Stress, psychological disorders.
- Acute infectious diseases.
- Inflammatory processes in the liver.
- Diseases of the digestive tract.
- General hypothermia, overheating of the body, excessive insolation.
- Hormonal imbalance, menstruation.
These factors are not capable of causing a gene mutation. They can only aggravate the clinical situation of an existing disease and provoke its relapse. If you avoid harmful effects on the body in every possible way, then you can live with Gilbert's syndrome all your life and not encounter its clinical manifestations.
Background liver diseases, in particular hepatitis and cirrhosis, can aggravate the course of the disease. In such cases, when the concentration of free bilirubin in the blood reaches 60 µmol/l, the substance penetrates into the cells and affects the mitochondria. Such disorders are manifested by a lack of cellular respiration and lead to energy deficiency.
When the concentration of bilirubin is more than 60 µmol/l, it penetrates into the cells of the head of the central nervous system, affecting the centers of the respiratory and cardiovascular systems. The described disorders are not characteristic of Gilbert's syndrome and are diagnosed only if it is combined with liver diseases.
Gilbert's syndrome and pregnancy
Pregnant women with this disease should be observed by obstetricians-gynecologists, gastroenterologists, and also undergo consultation with a medical geneticist. Women suffering from this disease undergo a molecular diagnostic test that differentiates the heterozygous form of carrier of the gene and homozygous forms of the gene. The risk of a child inheriting the disease will be increased only if the husband carries this gene, so before planning a pregnancy, both parents need to be examined.
During pregnancy, the disease is detected based on clinical symptoms. In most cases, it is benign and during pregnancy there is a decrease in bilirubinemia, which is explained by the induction of the enzyme glucoronyl gransferase by estrogens. Gilbert's disease is not a contraindication to pregnancy and does not have a negative effect on the fetus or pregnancy.
The woman successfully carries the child to term and gives birth. If you follow a dietary regimen, exacerbations are extremely rare and not pronounced. In some women, this syndrome is detected only during the second or third pregnancy, and in previous pregnancies there was no increase in bilirubin. And only some develop itchy skin , yellowing of the sclera, urticaria or atopic dermatitis .
Specific treatment is not carried out during pregnancy (or is carried out in exceptional cases with a significant increase in bilirubin - sorbents, ursodeoxycholic acid ), however, the woman should follow general recommendations:
- physical activity is excluded;
- alcohol;
- strict adherence to a diet with the exception of fatty, fried, smoked foods, canned food, products with dyes and flavor enhancers;
- eating regularly, without skipping;
- It is recommended to avoid stressful situations;
- sufficient sleep;
- limited sun exposure.
Diet
Diet 5th table
- Efficacy: therapeutic effect after 14 days
- Duration: from 3 months or more
- Cost of products: 1200 - 1350 rubles per week
It has already been said above that the diet of patients should be regular (long breaks between meals and fasting are prohibited), moderate (do not overeat) and dietary. Patients are prescribed Diet No. 5 , excluding fatty and spicy foods, fried foods, cooking fats, canned food, smoked foods, products with cream, coffee, cocoa, and chocolate.
Prevention
Parents who have had a child with this disease should definitely consult and be examined by a geneticist before planning their next pregnancy. This also applies to married couples planning to have children if their relatives are diagnosed with this syndrome.
To prevent exacerbations, it is important for the patient to:
- Compliance with the diet and quality of nutrition.
- Dietary food within table No. 5.
- Moderate physical activity without overload.
- Compliance with the work and rest regime.
- Hardening and a healthy lifestyle.
- Sanitation of chronic foci of infection.
- Treatment of pathology of the biliary tract.
- Rational use of medications. This primarily concerns the intake of glucocorticoids, anabolic steroids, Rifampicin , Streptomycin , Cimetidine , Levomycetin , Ampicillin , caffeine , paracetamol , diacarb .
- Consumption of alcoholic beverages is prohibited.
- Conducting preventive courses of ursodeoxycholic acid for biliary sludge .
List of sources
- Diseases of the fetus and newborn, congenital metabolic disorders / ed. R. E. Berman, V. K. Vaughan. M.: Medicine, 1991. 527 p.
- Podymova S. D. Liver diseases. M.: Medicine, 1993. - 544 p.
- Kolyubaeva S.N., Kulagina K.O., Petrova I.S., Krivoruchka A.B., Ivanova A.M. Molecular genetic diagnosis of Gilbert's syndrome using pyrosequencing. Laboratory of health care facilities. 2016; 8:4–6.
- Goncharik I.I. Gilbert's syndrome: pathogenesis and diagnosis / I.I. Goncharik, Yu.S. Kravchenko // Clinical medicine. - 2001. - No. 4. - P. 40-44.
- Kuznetsov A.S., Fomina I.G., Tarzimanova A.I., Oganesyan K.A. Differential diagnosis of benign hyperbilirubinemia // Clinical medicine. - 2001. - No. 3. - P. 8-13.