Bitterness in the mouth, nagging pain in the right hypochondrium, nausea may indicate cholelithiasis. Why can't you just remove the stones and save the gallbladder? And how does life change after cholecystectomy? Frequent questions from patients are answered by Mikhail Vladimirovich Kosachenko, laparoscopic surgeon, candidate of medical sciences, head of the operating unit of the City Clinical Hospital named after. V.V. Vinogradova.
Why does the gallbladder become inflamed?
Inflammation, or cholecystitis, occurs due to a violation of the outflow of bile and the presence of pathogenic microflora in the wall of the bladder. The flow of bile can be disrupted for two reasons:
Gallstones.
They are formed due to hormonal imbalance and/or bile acid metabolism and high cholesterol content in bile.
Biliary dyskinesia.
Violation of their contractile function leads to stagnation of bile - cholestasis. Against this background, cholecystitis can also develop.
Treatments for Nausea and Vomiting
- Drink more - eat less. Remove rich foods: cheese, pasta, meat (cooked in oil, steamed, grilled). According to my mother, porridges that provide energy for the whole day should be excluded from the menu. Curd cheeses, fruits (bananas, raisins, dried fruits). Borscht, spicy seasonings. Drink more still water, 0 sugar if possible. Drinking water, making you feel fainter, is stupid, stay in moderation - if you feel thirsty, then go drink water.
- Bed rest is the primary treatment. Place a pillow under your head, think about something good, switching your consciousness from focusing on the state of your body to building castles in the air. Make plans for the day, week, month. Reading or watching a movie will brighten up the moments of waiting for improvement.
- Calm down. Focusing on raising the root of the tongue, tense mouth, feeling the body as a whole becomes a great stress for the body. The subconscious worries, overthinks, causing a backlash that increases vomiting and nausea. Relax, drink a sedative, breathe in ammonia.
- Black tea with lemon, a cold cooling shower is an ideal medicine to eliminate a bad condition.
Folk remedies for treating illness
- Green, black tea, adding mint and mint extract will calm the stomach.
- Ginger in light foods.
- Basil tincture. Pour boiling water over the leaves for 20 minutes, strain. Use during attacks of nausea.
- Constantly warm the right side, hypochondrium. The liver is the direct initiator of lightheadedness.
- Dissolve a teaspoon of soda in boiling water and take orally. Carefully! Children under 10 years of age are not recommended to use this product.
- White layer of lemon, small amounts during urge.
- Maple leaf tincture, maple syrup.
- Clove extract mixed in water, ratio 1:5, frequency – 3 times a day.
- Powdered chicory dissolved in water.
- Herbs: rhizomes of valerian officinalis, chamomile flowers, peppermint leaves, cudweed.
- Alcohol must not be used! The urge will increase, putting a heavy load on the liver, stimulating complications due to stagnation of bile: heartburn, diarrhea, flatulence.
Is it possible to remove only the stones and leave the gallbladder itself?
No you can not. There is no such treatment method anywhere in the world. If stones have formed in the gallbladder, then its functioning is no longer adequate, and there is a chronic infection in it. Conservative therapy can be prescribed for a while, but such practice will not lead to a cure.
Don't let things get to the point of acute cholecystitis. If something bothers you, you should not take painkillers, but deal with the cause. In acute inflammation, the bladder is damaged to the point of necrosis of the wall. These are completely different conditions for the surgeon’s work and the patient’s recovery than during a planned operation.
Some general recommendations
Consumption of fatty foods is kept to a minimum
There is no need to worry: you will be able to continue eating normally shortly after surgery. Most people start eating the same day. You may be asked to cut down on fatty foods in the weeks before surgery, but this does not mean you have to continue to do so after surgery.
On the contrary, to ensure rapid recovery and well-being, it is worth eating a healthy, balanced diet that includes some fats.
The amount of fat eaten per meal directly affects digestibility: a small amount is much easier to digest, while a large amount may remain undigested and cause gas, bloating and diarrhea.
Doctors usually do not prescribe special diets, because problems after surgery and their tolerance are extremely individual. However, there are some general guidelines to avoid problems after removing a blister:
- No matter how trivial it may sound, you need to eat more often, but in smaller quantities. This will help the available bile to cope with food. Introduce some simple proteins into your diet, such as poultry and fish, low-fat dairy products along with vegetables, fruits and grains.
- Don't overeat on fatty foods. Avoid eating foods high in fat. Read labels and look for foods with 3 grams of fat or less per serving.
- Gradually increase the fiber content of your diet. This can help normalize bowel movements, reducing cases of diarrhea or constipation. On the other hand, it can worsen flatulence and cramps. It's best to slowly increase your fiber intake over several weeks.
- Consider the fact that many people who have had surgery find that caffeinated drinks and dairy products are difficult to digest.
A little talk about cholesterol
Like everyone else, your body produces more cholesterol than you take in in your diet. Since you no longer have a bladder, you don't have to worry about stones forming in it, which means you don't have to limit the amount of cholesterol you eat.
Now you can eat what you couldn’t afford before: eggs, meat, certain types of seafood, liver.
However, do not forget that cholesterol is formed from fat, and if you suffer from high levels, you will still have to set a limit on the total fat content in your diet, avoid fried foods, fast food and trans fats. Be sure to contact your doctor if you have severe symptoms that do not improve or last longer than expected, or if you are losing a lot of weight or feeling weak.
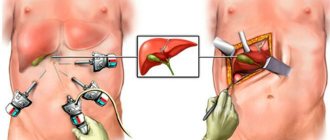
How is gallbladder removal surgery performed?
In most cases, laparoscopic cholecystectomy is performed. This is the removal of the gallbladder through four punctures in the abdomen, 5 to 10 millimeters wide. The second option is a classic open cholecystectomy through an incision in the right hypochondrium.
And another option, which is used in few places except our hospital, is mini-laparoscopic cholecystectomy. In this case, the minimum puncture size is 3 millimeters. The maximum cosmetic effect is achieved and there is virtually no pain. It is important to note: the choice of surgical method remains with the surgeon, depending on the specific situation.
Initial period
The pain syndrome - and this is the first thing a patient who has undergone any surgical intervention encounters - gradually disappears within a week. In the future, pain may appear only in case of straining when lifting heavy objects, difficulty defecating, etc.
For the first two days after the operation, the patient is under the supervision of the attending surgeon in a comfortable hospital room at the Center. Within 4-6 hours after surgery, the patient is able to move around and perform simple self-care activities. You are allowed to eat food the next day - in small portions, but often (5-7 times). Food should be low-fat and soft (for example, porridge, yogurt, cottage cheese, boiled meat, broth, etc.).
After two days, the patient is allowed to leave the hospital. The stitches are removed on the 10th day. At first, it is recommended to wear soft underwear so as not to irritate post-operative wounds. To speed up their healing, the doctor may prescribe a course of physical therapy.
Within a week after the operation, it is necessary to contact a gastroenterologist for correction of treatment and rehabilitation. In any case, patients will need:
- adhere to a special diet;
- abstain from sexual activity for 2-4 weeks after surgery;
- exclude heavy physical (including sports) loads, do not lift more than 3 kg in the first three months after surgery and more than 5 kg in the subsequent months.
How is it possible to remove a gallbladder with stones through such small holes?
We make a centimeter incision above the navel and inflate the abdomen through it to create sufficient volume. We insert a special tube (trocar) into the same incision and install endovideosurgical optics. With its help we see everything that happens inside.
At the top of the abdomen we make three more incisions of 3 millimeters each and install thin trocars. Through them we insert instruments of the same diameter. Next, the cystic duct, cystic artery and the posterior wall of the gallbladder are separated from the bed by a third. Only then do we cross these structures.
The gallbladder is removed from the liver bed, and then, using certain surgical techniques, is removed from the abdominal cavity.
Introduction
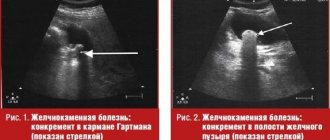
The incidence of cholelithiasis (GSD) remains high among both elderly and senile people, as well as young patients. In Russia, the number of patients with cholelithiasis has doubled over the past 10 years and, depending on the region, amounts to 5 to 20% of the adult population [1, 2, 4].
Cholecystectomy still remains the main treatment method for patients with cholelithiasis. More than 2.5 million operations are performed worldwide every year. In Moscow, up to 7,000 operations are performed per year per 100,000 population; in Russia as a whole, cholecystectomy ranks second among all operations performed [5, 9].
To the traditional treatment of cholelithiasis using open cholecystectomy, laparoscopic variants of this intervention and low-traumatic operations using minilaparotomy access have been added.
Despite the widespread use of surgical removal of the gallbladder, performed in various modifications, and extensive experience with these interventions, the results of this treatment do not satisfy the surgical community due to the relatively high rates of postoperative complications (1.5-35%) and mortality (1.1- 5.4%) [3].
The most common complications of the early postoperative period are prolonged bile leakage into the abdominal cavity or through the drainage of the common bile duct (CBD) and obstructive jaundice. After open cholecystectomy (OCE) they are observed in 5-15% of cases, after cholecystectomy from a mini-access (MEMD) - in 3.6%, after laparoscopic cholecystectomy (LCE) in 2-5% of cases [6, 8, 10-12] . These complications not only increase the suffering of patients, but can also lead to death.
The purpose of this study is to evaluate the capabilities of endoscopic methods in the diagnosis and treatment of early biliary complications after the use of various types of cholecystectomy in patients with cholelithiasis.
Material and methods
The study is based on the results of 4856 cholecystectomies performed from 2000 to 2007 at the clinical bases of the Russian State Medical University, City Clinical Hospital No. 12 and City Clinical Hospital No. 13 of Moscow. Of the total number of operations, classical cholecystectomy occurred in 2122 cases, CEMD - in 1024 cases, LCE - in 1710 cases. Early biliary complications in the form of postoperative bile leakage and obstructive jaundice syndrome developed in 135 (2.8%) patients (47 and 88 patients, respectively).
Among the patients there were 91 (67.4%) women and 44 (32.6%) men. The age of the patients ranged from 21 to 81 years (mean 58±14 years). The majority of patients (64.7%) were people of working age.
Of the 135 patients, 113 (83.7%) were admitted to the hospital on an emergency basis for various forms of acute cholecystitis, while 79 (58.5%) patients were operated on urgently, 29 (21.5%) - on an emergency basis.
In the preoperative period, all patients underwent a complex of diagnostic measures, which included: general and biochemical blood tests with determination of the level of cholestasis markers; ultrasound examination of the abdominal cavity; laparoscopy (in patients with suspected destruction of the gallbladder wall or pancreatic necrosis); computed tomography (to assess the condition of the liver and pancreas if there are signs of a pathological process in these organs according to ultrasound data); diagnostic endoscopic retrograde cholangiopancreaticography (ERCP), supplemented, if necessary, with therapeutic interventions. Particular importance in the preoperative examination of patients was given to performing dynamic hepatobilioscintigraphy with a pharmacological test, which made it possible to differentiate functional and organic changes in the sphincter apparatus of the major duodenal papilla (MDP) and thereby clarify the indications for therapeutic ERCP [7].
results
Bile leakage in the early postoperative period occurred in 47 (0.97%) patients. In table 1
The frequency of development of bile leakage after various types of surgery is presented.
In 13 cases, external bile leakage stopped spontaneously on days 2-4 after surgery. In the remaining 34 patients, bile leakage was prolonged, which required the use of special diagnostic and treatment methods.
In 41 (87.2%) of 47 cases, external bile leakage from the abdominal cavity drainage (33 patients) or CBD drainage (8) was noted. In 6 (12.8%) patients it was internal and was diagnosed by ultrasound (Table 2).
Most often in the postoperative period, external bile leakage was observed through the abdominal drainage (p≤0.01), and its frequency did not depend on the type of cholecystectomy.
The source of bile leakage was determined based on data obtained by contrasting the bile ducts by performing ERCP or cholangiography through the CBD drainage. The diagnostic performance of other methods was high.
In 17 of 34 patients, bile outside the ductal system came from the incompetent stump of the cystic duct, much less often - from the damaged main (in 2) or aberrant (in 3) bile duct (Table 3).
If the diagnosis of incompetence of the cystic duct stump usually does not cause difficulties, then the detection of damaged aberrant bile ducts during ERCP is very difficult and is based on identifying the flow of contrast agent beyond the accessory duct from the right lobe of the liver. In this case, bile does not enter the abdominal cavity constantly, but in portions when a certain level of pressure in the ducts is reached. Bile leakage from the gallbladder bed due to damage to Luschka's ducts cannot be diagnosed with ERCP; the conclusion about this type of bile leakage was established by exclusion, as well as by performing control video laparoscopy with examination of the area of the removed gallbladder. In case of iatrogenic damage to the main bile duct, ERCP revealed the release of the contrast agent beyond the biliary ducts. If the wall defect was small in size and was marginal, then it is very difficult to detect the entry of a contrast agent into the abdominal cavity. In a number of observations, a solution of methylene blue was added to the contrast agent and coloring of the bile secreted through the safety drainage was observed.
In 25 of 34 patients, the causes of bile leakage were associated with the presence of pathological changes in the bile ducts that were not identified before or during surgery. In 7 out of 34 patients with postoperative bile leakage, pathological changes in the bile ducts were excluded during ERCP. In 4 of these patients, the failure of the cystic duct stump was due to poor application of clips due to the anatomical features of the cystic duct or difficulties encountered during its isolation; in 3 patients, there was damage to the aberrant bile duct. In table 4
The reasons that led to bile leakage in the early postoperative period are presented.
In most cases, bile leakage due to incompetence of the cystic duct stump was caused by the presence of CBD stones, stenosis of the BDK, or a combination of these pathological conditions. In 12 of 25 cases with pathological changes in the extrahepatic bile ducts detected by ERCP, bile leakage was caused by incorrect interpretation or underestimation of available laboratory or ultrasound data before surgery. In the remaining 13 patients, according to the preoperative examination, no diseases of the biliary ducts were detected.
Of the 4856 operated patients, the development of obstructive jaundice syndrome in the postoperative period was noted in 88 (1.8%), in most of them on days 2-5 after surgery.
Diagnosis of obstruction of the bile ducts, as a rule, does not present great difficulties. The presence of complaints and corresponding clinical manifestations allows in most cases to suspect the inadequacy of sanitation of the bile ducts during cholecystectomy. Indicators of a clinical blood test are not decisive in the diagnosis of obstructive jaundice syndrome. Changes in biochemical blood parameters were more decisive. An increase in the level of bilirubin due to its associated fraction allows us to confirm the diagnosis of obstructive jaundice, and if there is an increase in the level of blood α-amylase, this may indicate the presence of stenosis of the BDK or acute occlusion of the ampulla of the BDK by a calculus.
Ultrasound examination of the abdominal cavity to assess the condition of the bile ducts in the early postoperative period is one of the mandatory components of the diagnostic algorithm for suspected biliary complications. It was performed in all patients within 2 to 4 days from the moment of surgery. In 12 (13.6%) patients, the ultrasound picture of the condition of the bile ducts was normal. In 32 (36.4%) cases, dilatation of the CBD (more than 9 mm) and lobar bile ducts (more than 4 mm) was diagnosed; in 26 (29.5%) cases, in addition to dilatation of the ducts, CBD stones were detected. In 18 (20.5%) patients, CBD could not be detected, which was due to increased intestinal pneumatization or severe obesity.
Of no small importance in the diagnosis of early biliary complications in the postoperative period is the performance of gastroduodenoscopy with examination of the BDK. The study allows for timely detection of acute occlusion of the ampulla of the ampulla of the ampulla or the terminal part of the CBD by a calculus, which in our observations was noted in 7 (8.0%) of 88 patients.
ERCP was the main method for diagnosing the causes of obstructive jaundice in patients in the early stages after various types of cholecystectomy. This study was performed on all 88 patients with obstructive jaundice syndrome (Table 5).
ERCP in the presence of obstructive jaundice syndrome allowed us to establish its cause in all cases and perform interventions aimed at its elimination. In 2 cases, on the 2nd day after LCE, complete bile duct transection was diagnosed; the patients underwent emergency reconstructive surgery. In 2 patients, changes were detected at the mouth of the BDDC, which were regarded as signs of independent migration of the stone into the duodenum; there were no other stones in the lumen of the CBD.
All patients with prolonged bile leakage and obstructive jaundice syndrome, which developed in the early stages after performing various variants of cholecystectomy, underwent endoscopic transpapillary interventions aimed at stopping bile leakage and restoring the outflow of bile into the duodenum.
A pathogenetically substantiated method of treating early postoperative bile leakage is decompression of the biliary ducts. This is due to the fact that the throughput of the terminal section of the CBD, even with the intact function of the sphincter apparatus of the BDK, is not enough to create the necessary pressure gradient between the bile ducts and the duodenum. The presence of stenotic changes in the cystic duct or choledocholithiasis further complicates the outflow of bile; there is a rapid increase in intraductal pressure, which in certain situations leads to leakage of the cystic duct stump and the flow of bile into the abdominal cavity or the development of obstructive jaundice syndrome.
To decompress the biliary ducts and thereby create optimal conditions for the outflow of bile into the duodenum, and not through the damaged bile duct or the incompetent stump of the cystic duct into the abdominal cavity, in most cases it was sufficient to perform endoscopic papillosphincterotomy (EPST). However, in a number of patients, despite its implementation, bile leakage continued, which was due not only to the large hole through which bile was discharged, but also to the impossibility of making an adequate papillotomy incision. In such situations, we considered it advisable to perform bilioduodenal stenting.
The stent diameter was typically 9-11 Fr with petal retainers. The duration of stay of the stent in the bile duct during bile leakage depends on the size of the defect through which bile is discharged outside the duct system, and in case of stump failure, it averages 5-7 days. Stenting in case of bile leakage from the Luschka tract or in case of marginal damage to the main bile duct may take longer (7-14 days). In order to decompress the bile ducts, it is possible to use nasobiliary drainage, however, compared to bilioduodenal stenting, this method is inferior due to unreliable fixation of the drainage in the duct.
Of the 122 patients with bile leakage and obstructive jaundice syndrome, 115 underwent endoscopic interventions (Table 6).
Diagnostic ERCP was performed in 7 patients, and in 1 observation, when there were indications for EPST, this intervention could not be performed for technical reasons (in a patient after gastric resection). EPST “in its pure form” was performed in 34 patients, including 23 with obstructive jaundice syndrome due to stenosis of the lateral bile duct and terminal CBD, 11 with bile leakage and in the absence of pathological changes in the extrahepatic bile ducts for the purpose of decompression of the biliary system. In 98 (85.2%) cases, endoscopic intervention was performed in one stage, in 14 (12.2%) - in two and in 3 (2.6%) - in three stages. In 4 out of 5 cases, bilioduodenal stenting was performed due to prolonged bile leakage in the early stages after cholecystectomy.
After ERCP and endoscopic interventions, complications occurred in 4 (3.3%) patients. In one observation, bleeding from the incision area was noted, which was stopped after local endoscopic hemostasis. In 3 (2.5%) patients, acute edematous pancreatitis developed, which was relieved by conservative measures within 2-4 days.
Thus, the analysis showed that the main reasons for the development of biliary complications in the early postoperative period after various types of cholecystectomy were pathological changes in the extrahepatic bile ducts that were not diagnosed before surgery or incorrect interpretation of laboratory and instrumental data. Much less frequently, they were caused by intraoperative situations that led to iatrogenic damage to the bile ducts and unreliable clipping of the cystic duct. The main method for diagnosing these complications was ERCP, based on the data of which treatment tactics were determined and endobiliary interventions were performed.
Memo before surgery
Pre-operation memo for patients
- click on the image to download.
Before surgery
before hospitalization
Before hospitalization, you will need:
- come to an appointment with the surgeon to receive a reminder and instructions
- undergo all necessary examinations before hospitalization
- bring compression stockings of class 1 compression, if necessary (the doctor decides) - class 2
on the eve of hospitalization
- make sure that all original examinations necessary for hospitalization are available
- Check with your doctor for the exact time of arrival at the emergency department
on the day of hospitalization (the day before surgery)
- in the morning before leaving for the hospital, take a shower (you can use antibacterial agents)
- undergo a hospitalization procedure, examination by a surgeon and an anesthesiologist in the hospital
- the evening before surgery - a light dinner until 20:00, then only liquids are allowed
- before bed - shower
On the day of surgery
- immediately after waking up, without getting out of bed, put on compression stockings
- In the morning before surgery you cannot eat or drink. An exception is taking a sip of water to wash down the medicine.
- honey. the staff will help with shaving the surgical area and guide you to the operating room
- in the operating room, the anesthesiologist will once again explain the anesthesia procedure and actions after the operation
- In preparation for the operation, you will have a venous catheter and, if necessary, an epidural analgesia system installed.
- you will come to in the operating room or intensive care unit
- If an epidural catheter is present, it will be removed in the intensive care unit
- after that you will be transferred to a ward
Chronic cholecystitis: symptoms and treatment
Chronic cholecystitis is a constant inflammation in the gallbladder, occurring with periods of exacerbation and remission (imaginary recovery). Sometimes the activity of the inflammatory process decreases sharply and nothing bothers the patient. But when exposed to provoking factors, the signs of chronic cholecystitis reappear, bringing considerable suffering to the patient. The disease can begin before the age of 30. Chronic cholecystitis worsens with errors in diet (eating fatty, spicy foods, drinking alcoholic beverages). In most cases, chronic cholecystitis is accompanied by the presence of cholelithiasis (cholelithiasis).
Symptoms of the disease
- Pain. In chronic cholecystitis, symptoms manifest primarily as pain. It is described by patients as aching, bursting. The location of pain may create some difficulties during diagnosis. These can be the supraclavicular fossa, the subscapular region, and the area behind the sternum. The latter localization causes it to simulate angina in coronary artery disease (coronary artery disease), accompanied by arrhythmias and palpitations. This symptom complex is called cholecystocardial syndrome, and it arises, among other things, from a toxic effect on the heart muscle. The intensity of pain may change when the solar plexus is involved in the inflammatory process (solar syndrome). Burning, unbearable pain appears in the navel area, radiating to the back.
- Nausea in chronic cholecystitis is a common symptom, as is vomiting. They occur in half of patients with concomitant gastroduodenitis and pancreatitis. Usually there is an admixture of bile in the vomit.
- Bitterness in the mouth, bitter belching is the most common complaint.
- Skin itching. Appears in case of bile excretion disorders, from skin irritation with bile acids.
- During exacerbations, fever, chills, jaundice, and activation of allergic diseases may occur.
How to treat chronic cholecystitis?
For chronic cholecystitis, treatment always begins with nutritional correction. The diet is the same as for the acute form of the disease. Bed rest is prescribed in the first days of an exacerbation, after which the restrictions are gradually lifted. It is mandatory to take antibacterial drugs and anti-inflammatory therapy. According to the doctor’s recommendations, in some cases you will also need to take antispasmodics, anticholinergics, agents that help normalize the flow of bile and painkillers.