The gallbladder is an organ of the digestive system that is a reservoir for the accumulation of bile. It is located under the liver and is connected to it by a complex system of bile ducts. Under the influence of certain pathological processes, the organ can become inflamed and damage other structures of the gastrointestinal tract.
If acute cholecystitis is not treated promptly, there is a high risk of developing dangerous complications, which can ultimately be fatal. Not a single organ in the human body is superfluous, including the gallbladder. But in some cases, surgery to remove an organ (cholecystectomy) helps to avoid the development of unwanted complications that pose a threat to the patient’s health and life.
If in the future a person follows the doctor’s recommendations and dietary nutrition, then the surgical intervention will not affect the quality and length of life. Open cholecystectomy is an old technique that is now rarely used. The procedure causes large post-operative wounds that leave behind a cosmetic defect.
In addition, open cholecystectomy has a long recovery period and often causes unpleasant complications. The procedure is used in acute cholecystitis complicated by peritonitis, as well as in cases where an inspection of the internal organs of the abdominal cavity is required. Recently, laparoscopy of the gallbladder has become increasingly common. This is an endoscopic treatment method.
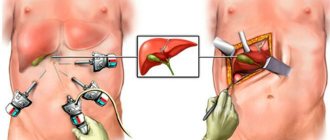
Using a special device, a high-quality image of the abdominal organs is displayed on the monitor. The surgeon makes only three to four punctures. Complications after laparoscopy are minimal. Unlike traditional surgery, patients quickly return to their normal rhythm of life. In this article we will talk in detail about laparoscopic gall bladder surgery.
Advantages
During laparoscopic surgery, the gallbladder is removed using a special device - a laparoscope. This type of surgical intervention has a number of unconditional advantages:
- low trauma;
- simple preparation steps;
- low probability of secondary infection;
- low blood loss;
- fast rehabilitation. After a few days the patient is allowed to go home. You can return to work in about a week;
- barely noticeable scars remain;
- no significant pain after surgery. Usually it is enough to take an analgesic to relieve discomfort;
- mobility of the surgical intervention, which means the patient is under anesthesia less.
Important! Laparoscopy can be diagnostic or therapeutic. The operation may mean the removal of stones in case of cholelithiasis (GSD), while the organ itself will not be removed.
How long does the operation take? Depending on the individual characteristics of the patient and the qualifications of the surgeon, its duration ranges from thirty minutes to two hours. The operation to remove the gallbladder lasts on average one hour.
No ads 1
What to take with you to the hospital?
With laparoscopic cholecystectomy, hospital stay rarely takes more than two days, so the number of things can be minimal.
Here is a list of necessary things
for hospitalization:
- 1.Passport and insurance policy
- 2.Medicines that you take regularly
- 3.Personal hygiene products
- 4.Comfortable change of clothes and linen
- 5.Anti-embolic compression stockings
- 6.Phone charger (and the phone itself)
Indications and contraindications
First of all, surgery is prescribed for patients diagnosed with the following pathologies:
- Polyps are peculiar growths on the mucous membrane of the gallbladder. They have a tendency to degenerate into atypical tumors;
- acute cholecystitis. In most cases, acute inflammation of the gallbladder is a direct indication for surgery. Patients experience severe abdominal pain, nausea, profuse vomiting, and hyperthermia. Taking antispasmodics and analgesics does not bring relief;
- cholesterosis – cholesterol deposition. More often diagnosed in young people. The reasons have not yet been studied. Nevertheless, experts talk about the role of metabolic disorders and associate cholesterosis with cholelithiasis (GSD). Digestion occurs and paroxysmal pain appears in the right side;
- cholelithiasis. Develops as a result of addiction to fatty foods and metabolic disorders. Patients are worried about nausea, bitterness in the mouth, pain in the right side. For many years, stones can lie quietly at the bottom of the organ and not bother a person. But under the influence of certain circumstances they emerge and block the lumen of the biliary tract;
- biliary dyskinesia. There is a violation of the evacuation of bile into the duodenum. With the hyperkinetic type, closure of the sphincters is observed, which causes intense colicky pain. In the hypokinetic form, the muscular wall of the gallbladder does not contract.
Diagnostic laparoscopy is performed when a malignant tumor is suspected, which cannot be diagnosed in any other way. The technique allows you to determine the stage of the process and diagnose tumor invasion into neighboring organs. Laparoscopy is also performed for ascites of unknown etiology.
Laparoscopic removal of the gallbladder is most often prescribed for acute cholecystitis
Are there any contraindications for the operation? Yes, the list of restrictions is much wider:
- pregnancy period;
- excess weight. This refers to extreme obesity;
- inflammation of the abdominal cavity;
- acute myocardial infarction;
- malignant neoplasm of the gallbladder. There is a risk of metastases;
- acute pancreatitis;
- peptic ulcer;
- cirrhosis of the liver.
In some cases, the surgeon is forced to suspend laparoscopy and proceed to open cholecystectomy:
- severe swelling of the gallbladder, which makes it impossible to carry out the procedure;
- adhesive process;
- fistula;
- suspected cancer;
- abscess;
- destruction of the organ wall;
- bleeding;
- damage to internal organs.
Several types of surgery are performed using laparoscopy. During a cholecystectomy, the surgeon removes the gallbladder. During choledochotomy, the common bile duct is opened, but the bladder itself continues to function. It is prescribed when the duct is blocked by parasites or a stone.
Anastomosis is performed when the outflow of bile is impaired. Therefore, the surgeon creates alternative ways for the secretion to drain. This is usually required for cholelithiasis and congenital pathology of the biliary ducts. How to prepare for surgery?
When is surgery needed?
Cholecystectomy is most often performed for cholelithiasis and gallbladder polyps.
Not every stone and not every polyp requires surgical treatment.
If we talk about cholelithiasis, we operate in the presence of symptoms or complications in the form of acute inflammation of the gallbladder (acute cholecystitis), migration of stones into the common bile duct (cholechodolithiasis) and subsequent cholangitis, pancreatitis, etc.
Asymptomatic cholelithiasis is not an indication for surgery,
with rare specific exceptions.
For gallbladder polyps, surgery is indicated for polyp size >10 mm, multiple polyps, or objective signs of their growth identified during observation.
Preparation
Preparation for laparoscopy consists of undergoing diagnostics. The patient undergoes a general blood and urine test, as well as hematological biochemistry. The blood type and Rh factor are determined. A blood test for viral hepatitis, HIV and syphilis is required. The patient must undergo an ECG and donate blood for a coagulogram. Before surgery, it is necessary to examine the biliary system using ultrasound and radiography.
After ten in the evening, on the eve of the operation, the patient is forbidden to eat or even drink. In the morning he is prescribed an enema and a laxative. Before the procedure, a surgeon and an anesthesiologist approach the patient and talk about the progress of the operation and the specifics of anesthesia. He must be aware of the possible consequences. The patient must give consent to undergo surgery. The patient may also be prescribed a sedative.
Important! If the patient is taking medications, he needs to ask the doctor whether they can be taken on the day of surgery.
In most cases, the operation is performed as planned. Within a week, medications that affect blood clotting are discontinued. For three days before surgery, foods that cause gas formation are excluded. The diet involves avoiding legumes, as well as fatty and fried foods.
Characteristics of the operation
The operation is performed under general anesthesia. Mask or intravenous anesthesia is used. Next, gases and liquids are removed from the stomach using a probe, and then a ventilator is connected. The surgeon fills the abdominal cavity with carbon dioxide. Then specialists make three to four small incisions through which special instruments are inserted.
Using a camera, information about the state of internal organs is transmitted to the monitor screen. The surgeon carefully cuts off the gallbladder and removes it from the abdominal cavity. At the end, an examination of the internal organs and antiseptic treatment is carried out. Stitches are applied.
Surgeons make three to four punctures on the anterior abdominal wall
How is the operation performed?
Before laparoscopy, the doctor tells the patient about the stages of the procedure, answers any questions that arise and warns about possible complications. The patient may be asked to leave contact lenses and jewelry outside the sterile area.
Gallbladder surgery requires pain relief. For this purpose, general anesthesia is used. It relieves pain and also relaxes the abdominal muscles, which facilitates the laparoscopy procedure. The effectiveness of local anesthesia for such surgery will not be enough. The drugs and dosage are selected by the anesthesiologist who is present at the operation.
When a person’s consciousness is turned off, a special probe is inserted into his stomach, with the help of which liquid and gases are removed. It is necessary to prevent vomiting or gastric secretions from entering the lungs, which is dangerous due to asphyxia. The device is left in this position throughout the entire operation.
The person is then put on a mask attached to a ventilator. Without this device, the patient will not be able to breathe on his own during laparoscopy. After performing such procedures, the patient is prepared directly for the surgical intervention itself:
- The first incision is made in the navel area
, through which the stomach is pumped with carbon dioxide to increase the volume of the peritoneum and straighten the organs. After inflation, a chamber with a flashlight is inserted. - Then the doctor makes three punctures from the right hypochondrium.
Through them, instruments are inserted to remove the bubble. - The surgeon carefully examines the organ
, determines its tension and assesses the amount of secretion inside. If necessary, excess contents are pumped out. - The doctor compresses the bile duct with the blood artery
, and after that the bladder begins to release. - The surgeon carefully and gradually cuts it out
, and if bleeding occurs, he cauterizes the area with electric current. - After complete resection of the bladder, it is pulled out through an incision in the navel
.
Possible complications
Complications are possible with any operation, and laparoscopy is no exception. Compared to open surgery, the endoscopic technique causes less unpleasant consequences, but they are still possible.
The following complications may occur after laparoscopy:
- bleeding;
- damage to the biliary ducts;
- suppuration;
- liver or intestinal damage;
- subcutaneous emphysema. Carbon dioxide accumulates under the skin due to the fact that the surgeon entered the trocar not into the abdominal cavity, but under the epidermis;
- in the presence of oncological processes, tumor spread may occur.
It is very common for patients to have a fever after surgery. This is natural, since surgery is a huge stress for the body. After piercing the skin with a needle, the integrity of the tissue is disrupted, which causes the formation of decay products, which are subsequently absorbed into the circulatory system, poisoning the body. Hyperthermia may also occur due to the presence of drainage. The immune system reacts violently to a foreign body.
After removing the drainage, the temperature returns to normal. If hyperthermia occurs immediately after the operation and there are no other symptoms, then there is no point in bringing it down; after a few days it will normalize on its own. If, in addition to fever, the patient has severe pain, it is necessary to inform the doctor. You should also be concerned if other symptoms appear:
- hyperthermia does not decrease for several weeks;
- temperature above 38 degrees;
- the surgical wound has red edges and purulent secretion is released from it;
- signs of infection: cough, wheezing in the lungs;
- intense pain in the wound;
- dry tongue;
- tachycardia;
- sweating, chills;
- nausea, vomiting.
Patients who have undergone cholecystectomy often have to deal with the following problems:
- inflammatory processes in the liver;
- disturbances in the functioning of the pancreas;
- skin rash, itching;
- disorders of the digestive tract: constipation or diarrhea, nausea, bloating, pain in the right side, flatulence.
Postoperative period
After the operation, the human body must rebuild itself, since the reservoir for the accumulation of bile secretion has disappeared. The body compensates for this loss by increasing the volume of the bile ducts. Normally, the diameter of the biliary ducts is about one millimeter, and a year after the operation it is 10–15 mm.
Diet for gallbladder removal
This process is inevitable. The ducts take on the role of the gallbladder. After removal of the organ, disturbances in digestive processes occur, and the amount of bile secreted decreases. If after cholecystectomy the patient abuses fatty and fried foods, he will be bothered by nausea, vomiting and diarrhea.
The cyclical flow of secretions is also lost, so it continuously enters the digestive system. A decrease in the concentration of bile acids leads to the loss of the bactericidal properties of bile. This entails the development of intestinal dysbiosis.
Attention! Paying attention to your health and following all medical recommendations plays a big role in successful recovery. Even if the operation was successful, it will not be possible to avoid negative complications if the patient returns to bad habits and poor diet.
On the first day after surgery, the patient is already allowed to get out of bed, walk and eat liquid food. Bandages or special stickers are applied to postoperative wounds. After the operation, the patient may experience pain for some time. Analgesics can cope with them.
Is a special bandage needed after surgery? Laparoscopy is a safe form of gallbladder removal procedure, so wearing a band is not necessary. It may still be prescribed to overweight patients who have weak abdominal muscles. The total time of the patient's stay in the hospital does not exceed ten days. The patient also requires home rest, so he is given a sick leave.
After cholecystectomy, patients can lead a full life
Typically, the patient is on sick leave for about ten days, but if necessary, this period can be extended. The maximum period of incapacity for work is thirty days. But there are severe cases when even a month is not enough for recovery. The treatment committee may decide to extend the period of sick leave.
After laparoscopy, it is important to follow three basic rules:
- Drug therapy that will help the body adapt to new circumstances. Patients are prescribed hepatoprotectors.
- Diet and nutrition regimen.
- Gymnastics for the abdominal muscles.
For the digestive system to function properly, it is simply necessary to lead an active lifestyle and exercise. If the operation was successful and no complications arose, then after a few months you can gradually increase physical activity. In the first week after surgery, walking is allowed. You can start standard sports training no earlier than six weeks later.
If the surgeon does not stitch the edges of the wound properly or they become separated, the wound may begin to ooze. If nothing is done, a noticeable defect may remain on the skin after healing. To avoid this, the skin around the wound should be treated with an alcohol solution, and the wound itself with hydrogen peroxide. At the end, apply a sterile bandage with syntomycin ointment. Until the wound stops oozing, it is not allowed to get it wet.
The healing process of sutures may be accompanied by the following clinical picture:
- aching pain at the wound site;
- humidity of the wound surface;
- bloating;
- itching;
- seal under the seam.
You can plan a pregnancy no earlier than three to six months after successful surgery. Pregnancy and childbirth are risk factors for the development of new stones, so before pregnancy it is important to pay special attention to your diet. During the period of bearing a child, it is advisable to be under the supervision of a gastroenterologist and do a preventive ultrasound of the abdominal organs.
Removal of the gallbladder through “punctures” (laparoscopic cholecystectomy)
Cholecystectomy
Cholecystectomy
(gallbladder removal) has been performed for about a hundred years. Currently, the technique of this operation has been developed and in typical uncomplicated cases does not present any difficulties for an experienced surgeon.
Indications
Calculous cholecystitis (presence of gallstones)
Gallbladder polyps
Traumatic gallbladder injury
Types of operations
Currently, gallbladder removal can be performed in two ways: 1) open (using an incision) and 2) laparoscopic (through punctures). If previously acute inflammation of the gallbladder and previous abdominal surgeries were a contraindication to removing the gallbladder “through punctures,” now almost all operations to remove the gallbladder are performed laparoscopically.
Open cholecystectomy
General anesthesia.
Drugs that relax muscles and painkillers are administered. A machine breathes for the patient through a special tube inserted into the trachea.
The incision can be made both in the right hypochondrium (a more traumatic approach, but at the same time the number of postoperative hernias after it is less), and in the midline above the navel.
The purpose of the operation is to separate the gallbladder from the liver with ligation of the artery that feeds it, as well as ligation of the cystic duct, through which it is connected to the common bile duct. At the same time, it is extremely important not to make a mistake and accidentally cross the common bile duct, which will lead to severe and often fatal consequences!
The operation in most cases ends with the placement of drainage (a small-diameter polyvinyl chloride tube to collect the resulting traumatic fluid and control possible bile leakage). The postoperative wound is sutured in layers. A cosmetic suture is applied to the skin.
One of the types of open cholecystectomy is an operation from
so-called
mini-access
. A small incision (5-6 cm) is made in the right hypochondrium. Next, the wound is expanded using a special ring.
Special curved instruments are used to manipulate the wound. The advantage of cholecystectomy from a mini-access is the low level of trauma, but at the same time, it is not possible to perform a full examination of the abdominal organs.
It should be mentioned that sometimes the surgeon is forced to complete the operation by inserting a thin tube into the common bile duct (if, for example, the presence of stones in this duct cannot be ruled out) in order to perform an X-ray examination in the postoperative period. In addition, a tube into the bile duct can be installed in case of complicated cholelithiasis.
Laparoscopic cholecystectomy.
This type of operation began to be performed since the late 80s of the 20th century and requires the use of high-tech and expensive equipment. At the development stage, this operation was accompanied by a fairly large percentage of damage to the common bile duct. Nowadays, the surgical technique has been developed and this situation is quite rare. But it should be mentioned that laparoscopic cholecystectomy (hereinafter referred to as LCE) should be performed only by an experienced surgeon or at least in his presence. Self-development of this technique is not allowed.
Laparoscopic cholecystectomy is performed under general anesthesia. After injection of carbon dioxide into the abdominal cavity (if the abdomen is not inflated and the anterior abdominal wall is not raised, the operation cannot be performed) through 4 punctures (3 in the right hypochondrium and one above the navel)
A camera and special instruments are inserted into the abdominal cavity. The meaning and stages of the operation are the same as for open surgery. The cystic duct and artery are not ligated, but are clamped with titanium clips.
After separation from the liver, the gallbladder is removed through a small incision above the navel. Drainage is usually not installed.
The difficulty for the surgeon when performing LCE is working in two-dimensional space (in fact, the operation is visible only in the monitor)
and lack of direct contact with tissues and structures. It should be remembered that in case of advanced disease or in the presence of anatomical abnormalities of the bile ducts, the surgeon may proceed to open surgery.
The patient tolerates laparoscopic cholecystectomy much easier than open surgery.
Currently, laparoscopic operations are performed not only through traditional access through four punctures, but also through the so-called monoport,
when all instruments are inserted into the abdominal cavity through one access above the navel (nowadays, this technique is increasingly recognized as inappropriate)
In addition, access to the gallbladder is carried out through the vagina (a similar operation was performed on the singer Madonna) and even through the stomach (instruments are inserted through the mouth into the stomach, its wall is dissected and thus the instruments are removed into the free abdominal cavity and then cholecystectomy is performed. An incision in the stomach wall later closed with special clips). The above-described interventions have only one advantage - no scars are left on the skin.
Postoperative period
Both after open and laparoscopic cholecystectomy, the patient in the vast majority of cases is taken to the general ward
The patient is strongly recommended to immediately perform gymnastics, and in the evening, sit down in bed and get up. Drinking is allowed immediately after the operation upon arrival in the ward. The next day, small amounts of liquid light food are allowed. They are transferred to the general table on the third or fourth day after surgery.
Discharge after open surgery occurs on days 5-7, after LCE on 2-3.
After open surgery, the patient will have to limit exercise for at least 4 months and wear a bandage. After LCE, only significant loads should be limited; wearing a bandage is not required.
The patient is usually discharged to work 15-21 days after surgery.
Complications of the operation
The worst complication of cholecystectomy for both the surgeon and the patient is injury to the common bile duct. These injuries vary from relatively minor to extremely complex (complete intersection of the duct, excision of a large part of it, excision very close to the liver), which will require a number of repeated operations, not always leading to success. That is why cholecystectomy should be performed by a surgeon with the proper experience that will allow him to understand this or that difficult situation. And remember, no real operating specialist will tell you that this operation is easy. The consequences of an error here are fatal.
In addition, after cholecystectomy, bleeding occurs (usually from the gallbladder bed) or bile leakage. These complications may require repeated emergency surgery.
In the later postoperative period, jaundice may develop - there are two reasons for it: 1) injury (ligation) of the common bile duct, 2) unrecognized stones left in it.
Finally, complications from the postoperative wound (suppuration, fluid accumulation) can sometimes occur.
Risk factors for complications:
Overweight
Long-term course of the disease, a number of previous exacerbations.
Acute cholecystitis
To summarize, let us recall that despite its apparent simplicity, cholecystectomy is fraught with a number of dangers and therefore should be performed by an experienced surgeon in a hospital setting, in which they are ready and able to treat not only the complications of the gallstone disease itself, but also possible complications of the operation (and such complications occur ABSOLUTELY IN ANY clinic). Unfortunately, now almost surgeons of any specialty and qualification are trying to perform this operation,
which, of course, is a reason for an extremely scrupulous choice of surgeon.
Tests and studies required for planned cholecystectomy:
1. General urine test.
2. General blood test.
3. Blood biochemistry (glucose, bilirubin, total protein, urea, creatinine).
4. ECG (electrocardiography).
5. FGDS (fibrogastroduodenoscopy).
6. Ultrasound of the abdominal organs.
7. Consultation with a therapist (for patients over 40 years old).
We work to ensure that every patient in need of surgical treatment gets to an experienced and competent surgeon who can perform the operation as safely as possible!
Reviews
Tatyana, 46 years old: I was diagnosed with cholelithiasis. The doctor recommended laparoscopic removal of my gallbladder. As he explained to me, several punctures will be made, after which barely noticeable scars will remain. Before the operation, I underwent an examination; no concomitant pathologies were identified. Laparoscopy was successful. The next day I was allowed to drink and eat liquid food. For some time I had abdominal pain, from which I took analgesics. The doctor said that the diet should be observed for life. I try to follow his advice and not overindulge in fatty and fried foods.
Lyudmila, 50 years old: I have been suffering from cholecystitis for a long time. During another exacerbation, the doctor advised me to remove my gallbladder. I was offered laparoscopy. The operation lasted about an hour. I didn't have any complications. The very next day I ate, got out of bed and walked. After two weeks, I returned to my usual rhythm of life and work. Once on holiday I ate fatty and fried food, after which I felt very bad. I radically changed my diet. I try to eat food at the same time in small portions.
Tatyana, 58 years old: I have been suffering from cholelithiasis for several years. When I ended up in surgery with another attack, the doctor offered me laparoscopy. He explained that this is a modern endoscopic method, which is much safer than open surgery. After the procedure, I was surprised that the scars were noticeable. The recovery period passed very quickly. A few days later I was discharged home, where I was on sick leave for another week.
So, life after gallbladder removal is possible. The operation, of course, makes adjustments to the functioning of the gastrointestinal tract, but after some time the body compensates for the loss of an important organ. Laparoscopy, compared to traditional abdominal surgery, rarely causes complications.
Patients can be home within just a few days. You can get out of bed and move around from the next day. If you want to avoid complications, follow your doctor's recommendations. Diet after surgery should become your way of life!
Doctor's comment
Have you been diagnosed with gallstones and have you been offered surgery - cholecystectomy? The laparoscopic technique today is the most gentle; the absence of pain in the postoperative period and rapid recovery are its main advantages. Moreover, laparoscopy using SILS technology allows you to achieve excellent cosmetic results, since all the surgeon’s actions are performed through a single 3-4 cm incision made along the upper contour of the navel, which after healing becomes almost invisible. In addition, SILS cholecystectomy is performed using video endoscopic equipment; all manipulations are performed under visual control, so the risk of complications during surgery is practically eliminated. But it should be noted that this method is not recommended if there are complications of gallstone disease. By the way, if you have a ventral or umbilical hernia, then during one operation you can get rid of both gallstones and the hernia. Therefore, do not delay the operation, because your hospital stay will only take one day, and after 5-10 days you will be able to return to your normal lifestyle!
Head of the surgical service at SwissClinic Konstantin Viktorovich Puchkov