Anomalies of the biliary tract in children
Anomalies of the development of the biliary tract, which according to modern concepts mean the gallbladder, bile ducts, sphincters, are one of the most common anomalies of the digestive organs. Interest in them has recently increased due to the introduction into clinical practice of modern methods of medical intrascopy - ultrasound (US), computed tomography (CT), magnetic resonance imaging (MRI), dynamic hepatobilis scintigraphy (GBSG), endoscopic retrograde cholangiopancreatography (ERCP). There is no unambiguous attitude towards developmental anomalies (AD).
From a clinical point of view, it is advisable to divide morphological changes in the biliary tract (BT) into: 1) development variant in which all the functional capabilities of the organ are preserved; 2) a developmental anomaly, when the existing individual characteristics in the structure of an organ practically do not affect its function or manifest themselves in the form of easily compensated disorders, but at the same time, under certain conditions, can be the basis for the development of a secondary pathological process; 3) defect (deformity) - gross changes in the structure of an organ, excluding its normal functioning.
If developmental options and defects (deformities) are diametrically opposed conditions, then developmental anomalies are often interpreted differently. It is proposed to distinguish minor developmental anomalies (MDA), for example, minor deformations of the gallbladder, which occur in every 4-5 healthy child and do not have any clinical manifestations. On the other hand, such anomalies of the bile ducts, such as a cyst of the common bile duct, are classified as major developmental anomalies (MAD), since, without being recognized in a timely manner, they occur under the “masks” of pancreatitis, hepatitis, cholecystitis, etc.
In pediatric practice, the following ARs are distinguished: 1) gallbladder; 2) bile ducts - intra- and extrahepatic; 3) combined.
Anomalies of gallbladder development
Anomalies in the development of the gallbladder (GB) are: 1) anomalies of quantity (agenesis, duplication), 2) anomalies of position, 3) deformations. In healthy children, various anomalies of the gallbladder are detected with a frequency of 17-20%. With diseases of the biliary tract, they are detected in every second child. In particular, among children with cholelithiasis, according to our data, every third child has anomalies of the gallbladder, and combined anomalies of the gallbladder and ducts in half of the cases. The frequency of detection of developmental anomalies of the biliary tract depends primarily on the resolution of a particular research method, which is determined by such indicators as sensitivity and specificity.
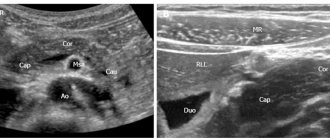
The higher the specificity, the more reliably the presence of a disease can be confirmed using a particular method. Thus, the sensitivity of ultrasound in detecting anomalies of the gallbladder is 88%, and the specificity is 98%. At the same time, in the diagnosis of anomalies of the ductal system, these indicators are 0%. The resolution of computed tomography in diagnosing bile duct abnormalities is significantly higher than that of ultrasound: sensitivity is 44% and specificity is 72%. For ERCP these figures are close to 100%. Based on this, ultrasound can be classified as a screening method for diagnosing gallbladder abnormalities. To clarify the anatomical and topographic relationships of the biliary tract and duct anomalies, it is necessary to use radiological methods.
Gallbladder agenesis is a fairly rare anomaly, occurring in 1 in 1600 autopsies. Hypoplasia (underdevelopment) of the gallbladder is also rare. It is necessary to differentiate congenital hypoplasia from hypoplasia caused by sclerosis - a “wrinkled” gallbladder. Final verification of the diagnosis is possible only on the basis of a morphological examination of the removed gallbladder. Agenesis, as well as hypoplasia of the gallbladder, have virtually no clinical manifestations in childhood. In the absence of a gallbladder, the common bile duct takes over the function of a bile reservoir. In the case of preserved functioning of the sphincter of Oddi, the disease is asymptomatic for a long time.
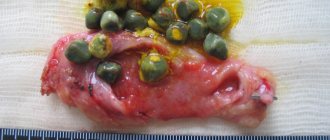
Gallbladder duplication occurs with a frequency of 1:3000-4000. There may be complete (true) doubling, when there are two fully formed bladders with separate cystic ducts. Sometimes the accessory bladder is rudimentary and hypoplastic. In such a bladder, conditions are created for stagnation of bile, which can lead to the development of inflammation and the formation of stones. The types of duplication include the gallbladder, divided by a longitudinal septum into two chambers, united by a single cystic duct. Duplication of the gallbladder is accompanied by various variants of the development of the cystic duct. The double ducts can separately or, after merging, simultaneously flow into the common bile or hepatic duct. Also, the accessory bladder can communicate with the liver through a separate duct.
Anomalies in the position of the gallbladder are also variable. The most common intrahepatic position is when the gallbladder is located in the falciform ligament of the liver; a mobile (“wandering”) gallbladder is also isolated. If in adults the intrahepatic location of the gallbladder is extremely rare, then in children, the younger the child, the larger part of the bladder is deepened into the thickness of the liver parenchyma. The intrahepatic location of the gallbladder can also occur for a long time without any clinical manifestations. But when an inflammatory process occurs in an intrahepatic gallbladder, the pathological process may spread to the adjacent tissue of the liver parenchyma, which leads to the appearance of “liver” symptoms: pain in the liver, hepatomegaly, increased blood levels of transaminases, alkaline phosphatase, etc. The clinical picture resembles hepatitis, which makes the diagnosis of this developmental anomaly difficult. There are also certain methodological difficulties when performing surgical operations on the intrahepatic gallbladder.
The mobile “wandering” gallbladder has practically its own mesentery and its location can be very diverse. This anomaly can be complicated by gallbladder volvulus, which is difficult to diagnose. Impaired blood and lymph circulation leads to the development of an inflammatory process with the formation of such severe complications as phlegmonous-gangrenous cholecystitis up to perforation of the gallbladder wall. Children, as a rule, are admitted with a clinical picture of an “acute abdomen.” Most often in childhood, various deformations of the gallbladder occur (from 59% to 74%). Most often these are kinks. Their occurrence is associated with a disproportion in the growth of the gallbladder and its bed. In this case, the kinks are usually localized in the area of the bottom and body of the bubble. With age, especially during periods of physiological traction, such deformations can be leveled out. According to our data, bends of the gallbladder occur in 41% of cases. At the same time, intravesical connective tissue constrictions can lead to kinking of the gallbladder. More often they are single, but multiple ones are also possible, when the cavity of the gallbladder is divided into several interconnected chambers. The presence of constrictions in the neck of the gallbladder is an obstacle to the outflow of bile and over time can cause the development of inflammatory changes in this area.
Gallbladder diverticula are a fairly rare developmental anomaly and their diagnosis today is only possible by performing ERCP, when the diverticulum cavity is filled with a contrast agent. During ultrasound examination, it is difficult to differentiate it from an inflection in the fundus, and when the shadow of a diverticulum is superimposed on the image of the gallbladder, it is mistakenly interpreted as a calculus. The clinical picture of a diverticulum does not have clear symptoms, but at the same time it can be the basis for bile stagnation and the formation of a chronic inflammatory process.
Increased surgical activity on the biliary tract, primarily for cholelithiasis (GSD), requires knowledge of the clinical features of the course of developmental anomalies. According to our data, the majority of children with AR, such as diverticulum, gastric deformities, etc., have vague abdominal pain, unstable stools with a tendency to constipation, and dyspeptic symptoms. However, it must be emphasized that these children often have concomitant gastroenterological diseases - gastroduodenitis, esophagitis, colitis, etc., accordingly, in-depth examination is required to diagnose abnormalities of the biliary tract.
Anomalies in the development of the bile ducts
Anomalies in the development of the bile ducts are very diverse. Their diagnosis has become possible recently thanks to the use of CT, MRI, ERCP and other research methods in clinical practice. AR of the bile ducts in 30-40% of cases is combined with anomalies in the development of the gallbladder, but can also be manifestations of other diseases, in particular polycystic disease.
Anomalies of the cystic duct (CD) are one of the most commonly observed in childhood. The options for PP anomalies are very diverse. These are, first of all, changes in the level of confluence of the bile duct, when the duct runs parallel to the common bile duct and flows into it closer to the duodenum. The extreme manifestation of AR is the direct opening of the PP into the duodenum. Often a change in the course or tortuosity of the PP is determined. The cystic duct can intersect with the common bile duct in front, behind, flow into it from the right, left, into the front or back walls. These PP deviations do not manifest themselves clinically, but may cause disruption of bile passage. A more pronounced AR is the absence of PP, while the gallbladder directly passes into the common bile duct. A double cystic duct may be present. Particular importance is attached to hypoplasia and fibrosis of the cystic duct, the presence of which plays an important role in impaired emptying of the gallbladder, as well as in the pathogenesis of its metabolic and inflammatory diseases (cholecystitis, cholelithiasis, cholesterosis).
Anomalies of the hepatic ducts are characterized by the confluence of the right or both hepatic ducts into the cervical part of the gallbladder, as a result of which hepatic bile enters the duodenum through the cystic duct. These features must be kept in mind when assessing the results of fractional duodenal intubation. Frequent anomalies are accessory bile ducts that drain individual segments of the liver. Their recognition, which is possible during ERCP, is important for preventing errors during surgical interventions, in particular laparoscopic cholecystectomy.
Bile duct cysts can be in any part of the biliary system and, according to location, are divided into intra- and extrahepatic. Among the extrahepatic cystic formations, a common bile duct cyst, choledochocele, and congenital diverticulum are distinguished.
Common bile duct cyst (CBD) is the most common anomaly of the extrahepatic biliary tract. The saccular shape predominates; fusiform expansion occurs in older children. Among the patients, girls predominate (80%). AR is based on congenital underdevelopment of the muscle fibers of the bile duct wall. An infectious process in the biliary tract in the antenatal and postnatal periods cannot be excluded. Most often, cystic dilatation of the CBD is observed, but the common hepatic duct can also be dilated. The cyst develops due to constant intraductal pressure due to an obstruction in the distal part of the common bile duct. The size of the cyst varies depending on the amount of bile - from 10-15 cm to 30 cm or more. In addition to thickened, putty-like bile, the cyst may contain stones. In severe cases, the clinical picture of congenital CBD expansion is characterized by the classic triad: abdominal pain, intermittent jaundice, and the presence of a tumor-like formation in the right upper abdomen. A tumor-like formation is palpable in the majority (2/3) of children and is a cardinal sign of the triad of symptoms. It has clear boundaries; compacted, smooth, painless, displaced to the sides of the liver. The pain is localized in the right hypochondrium, epigastric region or around the navel, which is typical for preschool children. It is dull, but can be paroxysmal like hepatic colic; not related to food intake. Jaundice is intermittent and accompanied by itchy skin. Bilirubin is detected in urine. The levels of bilirubin in the blood are increased due to the conjugated fraction, alkaline phosphatase, leucine aminopeptidase, and β-glutamyl transpeptidase.
The severity of each symptom, their sequence and combinations can be very different, which makes it difficult to diagnose a CBD cyst. The triad of symptoms is detected only in 20-60% of patients, although individual signs of the disease occur constantly. Most often, disorders associated with a CBD cyst occur suddenly. In some patients, the course of the disease is chronic with periods of exacerbations and remissions. Complications are varied: pancreatitis, cholecystitis, development of liver cirrhosis. In the presence of cholelithiasis, obstructive jaundice may develop. Diagnosis, in addition to clinical signs, is based on the results of ultrasound, GBSG, CT, and ERCP. CBD cyst is differentiated from diseases accompanied by abdominal pain and jaundice: viral hepatitis, cholelithiasis, cholecystitis, biliary atresia. When identifying a tumor-like formation in the abdomen, it is necessary to exclude liver echinococcosis, right-sided hydronephrosis, tumors, mesenteric cysts, enlarged lymph nodes due to lymphogranulomatosis, etc. Treatment is surgical, and the prognosis with correct diagnosis and timely surgery is favorable.
Congenital diverticulum, a rare AR, is usually connected by a pedicle to the CBD, hepatic ducts or gallbladder. The clinical picture is characterized by abdominal pain and periodic jaundice. ERCP and laparoscopy are indicated. Since upon examination the diverticulum externally resembles an additional gallbladder, a histological examination is necessary. The inner surface of the diverticulum is lined with epithelium of the bile ducts. Treatment is surgical, the prognosis is favorable.
Choledochocele is a cystic expansion of only the intraduodenal part of the common bile duct. Above the cyst, moderate dilatation of the bile ducts is possible. The pancreatic duct flows into the cyst, which opens into the duodenum. Thus, with an increase in intraduodenal pressure and the simultaneous presence of duodenobiliary reflux, the contents of the duodenum can enter the pancreatic duct with the subsequent development of pancreatitis. At the same time, pancreatic secretions, entering the proximal parts of the biliary tract, contribute to the development of enzymatic cholecystitis. There is a high risk of stone formation in the gallbladder. Clinical manifestations are the same as in patients with a CBD cyst, although they are less pronounced. Treatment is surgical. Sometimes there may be cystic lesions of both the extra- and intrahepatic bile ducts, which necessitates differential diagnosis.
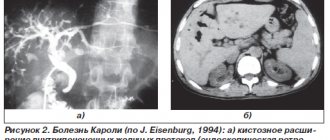
Cystic dilatation of the intrahepatic bile ducts (Caroly's disease) is characterized by the presence of multiple cysts, which are a continuation of the primary branches of the intrahepatic biliary ducts. The disease is a hereditary AR and can be observed in family members or relatives. The cysts, shaped like cherries, are lined with cuboidal epithelium. Manifestation of AR is possible in children of any age. Paroxysmal pain in the right hypochondrium, skin itching, rise in body temperature, and yellowness of the skin appear. Elevated levels of bilirubin, transaminases, and alkaline phosphatase are detected in the blood. The liver is enlarged, but there is no portal hypertension. Cystic expansion is assumed when multiple focal hypo- or anechoic formations are detected in the liver parenchyma as a result of ultrasound. The final diagnosis is based on ERCP data and the results of liver puncture biopsy. Caroli disease is often combined with cystic fibrosis of the liver, abnormalities of the extrahepatic bile ducts; in these cases, portal hypertension develops. Treatment is symptomatic; liver transplantation is promising.
Atresia of the extra- and intrahepatic bile ducts, formally referred to as AR of the biliary tract, is essentially a defect, without correction of which children quickly die. It occurs on average once every 20-30 thousand births and is often (30%) combined with other developmental anomalies. The possibility of atresia must always be taken into account in the case of an increase in the child’s jaundice of the skin, icterus of the sclera, further development of hepatosplenomegaly, signs of portal hypertension, and hepatocellular failure. Atresia is differentiated from physiological jaundice of newborns, bile thickening syndrome, fetal hepatitis, sepsis, cytomegaly, toxoplasmosis, CBD cysts, Rotor and Crigler-Nayyar syndrome, hemolytic anemia, etc. For atresia of extrahepatic bile ducts, surgical treatment with reconstructive interventions is indicated. The only way to save a child with atresia of the intrahepatic bile ducts is currently orthotopic liver transplantation.
The establishment of biliary tract ARs of different nature and severity in childhood raises a number of questions for the pediatrician regarding the observation and further management of patients. This especially applies to children suffering from metabolic and inflammatory diseases such as cholelithiasis and cholecystitis. Our own long-term experience indicates more pronounced manifestations of cholelithiasis, combined with AR of the gallbladder or bile ducts. The disease itself, as a rule, manifests itself at an earlier stage (even in children of the first three years of life), has a progressive course and does not respond to conservative therapy, including the use of ursofalk. If children have bipolar disorder and especially pronounced (severe) changes in the biliary tract, treatment tactics should be carried out in collaboration with pediatric surgeons. For example, diagnosing a common bile duct cyst using both ultrasound and other instrumental research methods is always regarded as a high risk of developing diseases of the hepatobiliary system and pancreas.
A feature of the vast majority of AR of the biliary tract in childhood is the absence of pathognomonic clinical signs. The presence of periodic abdominal pain or moderate dyspeptic disorders is usually associated with functional disorders of the digestive organs, especially since the majority of children with AR experience neurovegetative changes and psychoemotional disorders. It is important to take into account that the pathogenetic significance of AR of the biliary tract in children increases in the presence of hereditary burden, metabolic disorders, especially lipids, allergic and gastroenterological diseases, side effects of drugs, mainly in relation to the liver and biliary tract. The use of modern research methods in clinical practice, on the one hand, significantly expands diagnostic capabilities; on the other, it poses challenges for the correct interpretation of various morphofunctional changes in the biliary tract, including its developmental anomalies.
Anatoly ZAPRUDNOV,
Head of the Department of Pediatrics with Childhood Infections, Faculty of Advanced Training for Physicians.
Lyudmila BOGOMAZ,
department assistant.
Lyubov KHARITONOVA,
professor of the department.
Russian State Medical University.
Symptoms of major diseases
The clinical picture and signs of disease vary slightly. If these are cramping attacks of organ disease, then pain appears in the right side with a return to the back to the right, then moves to the shoulder and under the shoulder blade. Dyspeptic disorders include vomiting and nausea. The abdominal muscles are very hard and tense. But there are similar symptoms of gallbladder disease :
- yellowing of the mucous membranes of the eyes and skin,
- sharp or increasing pain on the right side; when you breathe, there is a cramping pain,
- body temperature +38 degrees,
- bloating of the peritoneum,
- diarrhea,
- pain when wanting to go big,
- convulsions, chills.
Diagnostics
First of all, during the initial diagnosis of diseases of the gallbladder and biliary tract, the gastroenterologist collects anamnesis, palpates the abdominal area, prescribes blood, urine, stool, and ultrasound tests. If necessary, a laparoscopic diagnostic method is used: if there is suddenly a suspicion of cholecystitis or cancer.