The gallbladder is classified as an auxiliary organ of digestion. Its main task is the accumulation of bile, which is produced by the liver. Our body needs bile to digest animal fats. Therefore, disturbances in the functioning of the bladder are accompanied by digestive disorders and pain in the right hypochondrium. In this case, the patient undergoes an ultrasound of all abdominal organs, during which the gallbladder is examined.
- What it is?
- Who is prescribed an ultrasound of the gallbladder?
- How should you prepare for an ultrasound?
- How is the procedure done?
- What are normal indicators for the gallbladder?
- What pathologies of the gallbladder can be detected on ultrasound?
Indications
An ultrasound scan of the gallbladder and bile ducts can be performed either upon the direction of the attending physician or on personal initiative. The following symptoms may suggest the advisability of checking this body:
- regular feeling of nausea;
- unpleasant taste in the mouth after eating;
- pain in the abdominal area;
- pain in the right hypochondrium;
- regular heaviness in the stomach after eating;
- sudden loss of appetite;
- jaundice;
- acholic stool;
- biliary colic;
- palpable formation;
- heartburn.
You should undergo a diagnosis if you begin to gain excess weight, severe poisoning or injury to internal organs occurs. If you decide on your own initiative to examine your gallbladder, it is best to start your diagnostic journey with a comprehensive ultrasound of the abdominal cavity, which includes a scanning protocol for this organ.
Indications for diagnostics
A gastroenterologist may prescribe an ultrasound method for diagnosing the gallbladder in the following situations:
- repeated painful sensations on the right side of the hypochondrium, which can only be relieved with the help of painkillers;
- discomfort and feeling of heaviness in the liver area;
- bitter taste in the mouth;
- yellow color of the skin and external mucous membranes;
- irregular diet;
- abuse of fatty, smoked, spicy, fried foods;
- too frequent use of low-calorie diets;
- taking medications for too long;
- abnormal values in laboratory blood tests (AST, ALT, bilirubin and others);
- biliary dyskinesia;
- obesity;
- cholelithiasis;
- abdominal trauma;
- when prescribing and selecting female hormonal contraceptives;
- the process of monitoring the condition of the biliary tract in the presence of tumors;
- monitoring the effective effect of therapy.
What will an ultrasound of the gallbladder show?
Ultrasound examination data will detect signs of the following diseases:
- chronic and acute pancreatitis;
- cholecystitis;
- biliary dyskinesia;
- cholelithiasis;
- “porcelain gallbladder” syndrome;
- cholangiocarcinoma and Courvoisier's sign;
- gallbladder carcinoma;
- gallbladder polyps;
- cysts of the gallbladder and common bile duct;
- calcification of the gallbladder walls.
Unfortunately, ultrasound images are not accurate enough to definitively judge the malignant or benign potential of a mass, so if the ultrasound yields alarming results, the patient will be sent for further evaluation with MRI or CT cholangiography. If gallbladder polyps are detected on ultrasound, a repeat examination is usually prescribed after 2-3 weeks. If there are signs of rapid growth, then there is a possibility of their development into a malignant formation. Ultrasound scanning of the gallbladder in children reveals developmental anomalies, atypical location, double gallbladder or no gallbladder at all. Any deviations from the norm will require a repeat scanning procedure after 15-20 days to monitor the dynamics of the process or a more high-tech study - CT or MRI of the abdominal cavity for final diagnosis.
| Ultrasound service | Price according to Price, rub | Promotion price, rub |
| Ultrasound of the abdominal organs and retroperitoneal space (liver, gall bladder, pancreas, spleen) | 1500 rub. | |
| Ultrasound of one organ (liver, gall bladder, spleen, pancreas, bladder, adrenal glands) | 800 rub. | |
| Ultrasound of the abdominal organs and kidneys | 1700 rub. | |
| Ultrasound of the abdominal organs + ultrasound of the kidneys + ultrasound of the bladder | 2000 rub. | |
| Kidney ultrasound | 800 rub. | |
| Comprehensive kidney examination with a 20% discount (kidney ultrasound + tests) | 3530 rub. | 2999 rub. |
| Comprehensive ultrasound with a 20% discount (ultrasound of the abdominal organs + ultrasound of the kidneys + ultrasound of the thyroid gland) | 3200 rub. | 2599 rub. |
| Comprehensive ultrasound for women with a 20% discount (ultrasound of the abdominal organs + ultrasound of the kidney + ultrasound of the thyroid gland + pelvic ultrasound with an abdominal probe + ultrasound of the mammary glands) | 5800 rub. | 4599 rub. |
| Comprehensive ultrasound for men with a 20% discount (ultrasound of the abdominal organs + ultrasound of the kidneys + ultrasound of the thyroid gland + ultrasound of the prostate with an abdominal probe) | 4700 rub. | 3699 rub. |
Propaedeutics of radiation methods for examining the gallbladder
The leading method for diagnosing pathological changes in the gallbladder (GB) is ultrasound examination (US).
Ultrasonography
Its undoubted advantages are non-invasiveness, the ability to quickly and portablely conduct research; absence of ionizing radiation and the need for intravenous administration of contrast agents; independence from the physiological state of the gastrointestinal tract and hepatobiliary system [1–3].
Features of gallbladder syntopy - the proximity of its posterior wall in the body and fundus to the right parts of the large intestine and duodenal bulb - dictate the need to prepare patients for ultrasound examination in order to reduce pneumatization of the corresponding parts of the digestive tract. This requires at least a 6-hour fast on the eve of the diagnostic procedure, and it is optimal to conduct the study on an empty stomach after a night's sleep. Such conditions are also required for the most detailed visualization of the structure of the gallbladder wall and its contents, since it is a hollow organ filled with bile and capable of contracting in response to humoral stimulation during food intake, which leads to a decrease in its size, a sharp thickening of the walls and the inability to detail intraluminal changes [2, 3].
The anatomical structure of the gallbladder is simple. It consists of a narrow neck connecting to the cystic duct, a bladder body with almost parallel walls, and a dome-shaped bottom. At the junction of the neck and the cystic duct, the wall often forms a pouch (or diverticulum) of Hartmann, in which stones can accumulate, blocking the exit of the cystic bile [3–5] (Fig. 1).
To conduct an ultrasound examination of the gallbladder, the scanner sensor (usually with a frequency of 3.5 MHz) is placed in the right hypochondrium of the subject - the site of the anatomical projection. Visualization of the organ can be improved by placing the patient on the left side, which allows the intestinal loops to be somewhat pushed to the left; the same purpose is served by conducting the study while holding the breath with a deep breath. Visualization of the gallbladder through the intercostal spaces is the most consistent, but the least informative and is used mainly in urgent situations in unprepared patients. To better assess the nature of intravesical changes (the presence of small stones, identifying their mobility), it is possible to conduct an examination in a vertical position or with the body tilted forward [2–5].
In the diagnosis of cholelithiasis (GSD), ultrasound scanning rightfully occupies a leading position. The sensitivity of ultrasound in detecting gallstones exceeds 95%, which look like hyperechoic structures with an acoustic shadow [1, 5] (Fig. 2).
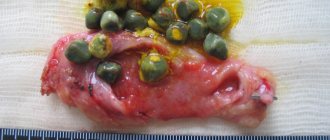
In the vast majority of cases, the stones are mobile, but can be fixed to the wall or motionless in the neck of the bladder. Other foreign bodies that mimic cholelithiasis may be blood or pus clots or parasites. Gallbladder polyps are immobile or have limited mobility if they have a pedicle, are always connected to the wall and, as a rule, do not give an acoustic shadow; usually their size does not exceed 5 mm. As a rule, against the background of a long absence of contractions of the bladder, it is possible to visualize the stratification of bile into two components with a clear interface, one of which is anechoic and occupies the upper parts of the bladder in relation to the horizontal plane, the other is more dense, located below. This phenomenon, called stagnation of bile, or sludge, occurs due to the presence of cholesterol and calcium bilirubinate crystals in it and their ability to reversibly form large aggregates (Fig. 3) .
The most common complication of cholelithiasis is acute cholecystitis, the cause of which is almost always a violation of the outflow of bile from the gallbladder. The main ultrasound signs of this pathology are:
- the presence of stones in the lumen of the bladder (the most typical finding is an “impacted” stone in the neck) - Fig. 4;
- thickening of the wall more than 3 mm with the appearance of heterogeneity of its structure, delamination (Fig. 4);
- an increase in the transverse size of the bladder by more than 4 cm; detection of the greatest pain at the site of ultrasound projection of the gallbladder (ultrasound Murphy’s symptom), which may not be detected in gangrenous cholecystitis [3, 5] (Fig. 4).
The combination of these symptoms with the detection of fluid accumulation near the bladder, especially in combination with the identification of a wall defect, indicates its perforation and, possibly, the formation of a peripysical abscess (Fig. 5). The detection of ultrasound signs of gas accumulation in the lumen of the bladder against the background of other signs of acute inflammation indicates such a severe pathology as emphysematous cholecystitis caused by gas-forming anaerobic flora [3, 5] (Fig. 6).
Another complication of cholelithiasis, manifested by a violation of the passage of bile, is choledocholithiasis. Violation of the outflow of bile along the common bile duct causes its expansion of more than 7 mm, expansion of the intrahepatic bile ducts (more than 40% of the diameter of the adjacent branch of the portal vein) (Fig. 7). Indisputable evidence of choledocholithiasis is the detection of stones, which are most often localized in the distal part of the common bile duct, but can be visualized only in 70–80% of cases [1, 4, 5].
Dilation of the intra- and extrahepatic bile ducts is also observed with such a complication of cholelithiasis as Mirizzi syndrome, which consists of obstruction of the common bile duct as a result of the volumetric effect of the inflammatory reaction of tissues to a stone located in the neck of the bladder or cystic duct, with a low confluence it in the common bile duct (Fig. [5].
Often the formation of stones in the gallbladder is accompanied by benign changes in its walls, one of the main ones being a violation of cholesterol metabolism. These changes are called hyperplastic cholecystopathy. One of its variants - cholesterol dystrophy is manifested by such ultrasound signs as the detection in the wall of the bladder of hyperechoic deposits no larger than 1 mm in size, which do not give an acoustic shadow, but are accompanied by a reverberation effect (the bubble vaguely resembles a strawberry), which are lipid deposits (Fig. 9) . More pronounced changes in the wall, called adenomyomatosis, are manifested in its thickening, the formation of intramural diverticula (Aschoff-Rokitansky sinuses), containing hyperechoic cholesterol deposits with a reverberation effect (“comet tail”) and microliths that give an acoustic shadow (Fig. 9). Hyperplastic cholecystopathy can affect both the entire bladder and part of its wall [2, 5].
It is known that removal of the gallbladder for cholelithiasis does not relieve patients from metabolic disorders, including hepatocyte dyscholia, which persists after surgery [6]. The loss of the physiological role of the gallbladder, namely the concentration of bile in the liver during the interdigestive period and its release into the duodenum during meals, is accompanied by a violation of the passage of bile into the intestine and indigestion [6, 7].
Changes in the chemical composition and volume of bile, its chaotic entry into the duodenum after cholecystectomy (CE) disrupt the digestion and absorption of fat and other lipid substances, reduce the bactericidal nature of duodenal contents, which leads to microbial contamination and impaired motility of the duodenum, the development of bacterial overgrowth syndrome in the intestine (especially in the ileum), disruption of the enterohepatic circulation and decreased synthesis of bile acids in the liver [6]. As a consequence, a syndrome of impaired digestion, the symptoms of which are often mistakenly interpreted as postcholecystectomy syndrome (PCS), is associated by surgeons primarily with mechanical obstacles to bile outflow that were not recognized before surgery or were not eliminated during cholecystectomy (stones left or emerging again in the common bile duct, stenosis of the papilla of Vater and etc.) [6].
When preparing for a cholecystectomy operation, much attention is always paid to diagnosing mechanical obstacles to bile outflow into the duodenum. The situation is completely different with preoperative verification of extrahepatic biliary dysfunctions. The absence of indirect signs of functional disorders of the sphincter of Oddi in the form of dilation of the common bile duct during ultrasound, increased liver enzymes, pain attacks, etc. does not at all exclude dysfunction of the papilla of Vater, which forms long before the patient’s admission. According to our data, in 45% of patients with cholelithiasis, radionuclide hepatobilis scintigraphy (GBSG) reveals functional disorders in the transport of radiopharmaceuticals from the common bile duct to the duodenum, which do not require retrograde cholangiopancreatography and endoscopic correction.
In some cases, radionuclide methods are simply no alternative due to the strict specificity of the inclusion of radiopharmaceuticals (RP) in various metabolic processes (GBSG). The functional state of the hepatobiliary system in any pathology of the hepatobiliary system, including cholelithiasis, is studied using standard GBSG.
Hepatobiliscintigraphy
GBSG allows you to objectively evaluate the most important processes from the standpoint of the functioning of the digestive transport conveyor: bile synthetic and bile excretory functions of the liver, as well as the transport of bile into the duodenum. The method is based on recording the passage of short-lived radionuclides Tc-99m + bromezide through the biliary tract.
The study is carried out on an empty stomach, in a horizontal position of the patient after the administration of 3 mKM Tc-99m + bromezide intravenously. The duration of the procedure is 60 minutes. As a choleretic breakfast, patients take chicken egg yolks or 200 ml of 10% cream 30 minutes from the start of the study.
Normal indicators of GBSG are considered:
1) the half-life (T1/2) of the radiopharmaceutical (RP) from the liver is less than 35 minutes; 2) the half-life (T1/2) of radiopharmaceuticals from the common bile duct is less than 50 minutes; 3) the time of receipt of radiopharmaceuticals into the duodenum is less than 40 minutes; 4) adequate supply of radiopharmaceuticals to the intestine is the predominance of radiopharmaceutical activity in the duodenum compared to that in the common bile duct by the end of the study.
The generally accepted standard method of radioisotope research with a choleretic breakfast does not always make it possible to specify the nature of functional changes in the bile outflow. This is explained by the fact that the food load exerts its effect both by activating the entry of cholecystokinin (CC) into the bloodstream upon irritation of I-cells of the duodenal mucosa and intramural nerve plexus [8]. The activity of digestive enzymes and the sensitivity of the sphincter apparatus of the biliary tract to intestinal hormones is variable and in practice difficult to determine [9]. The tone of intramural nerve fibers depends on the physiological activity of the organs of the upper digestive tract [10, 11].
In this regard, in the radionuclide diagnosis of extrahepatic biliary dysfunction (IBD), intravenous administration of the hormone cholecystokinin is often used, but the relaxing effect of this drug depends on the state of the central nervous system, the hormonal background of the patient and is disrupted in case of cholesterosis of the gallbladder, since the localization of receptors for cholecystokinin coincides with the sites of deposits cholesterol esters in the bladder wall and bile ducts, which makes it difficult to accurately determine the dose of the administered hormone [8, 10].
To clarify the nature of bile outflow disorders along the common bile duct in the Faculty Surgery Clinic named after. S. I. Spasokukotsky Russian National Research Medical University named after. N.I. Pirogov on the basis of the First City Hospital performs GBSG with amino acid cholekinetic test (GBSG-ACT) and GBSG with Buscopan® test (RF patent No. 2166333).
GBSG with amino acid cholekinetic test
The study is carried out on an empty stomach. 30 minutes after the administration of the radiopharmaceutical and the start of the study, a solution of amino acids Vamin-14 or Freamin, which does not contain glucose and electrolytes, is injected into a peripheral vein. We consider the last condition to be very important, since the hyperglycemia that occurs during glucose infusion completely or partially inhibits the secretion of cholecystokinin [8]. The dose of the drug was chosen at the rate of 1.5–2 ml/kg body weight (80–130 ml). The duration of the infusion is 5–7 minutes, since the administration of an amino acid solution for more than 10 minutes (regardless of the dose) does not lead to an increase in the release of endogenous cholecystokinin, but, on the contrary, reduces the incretion of the hormone [9]. IAP and the cause of delayed excretion of the radiopharmaceutical by hepatocytes are assessed based on the differences in the parameters of standard GBSG and GBSG-ACT (Fig. 10).
GBSG using hyoscine butyl bromide
Hyoscine butyl bromide (Buscopan®) is a derivative of the tertiary ammonium compound hyoscine. Hyoscine is an alkaloid present in plants of the genus Duboisia. It is chemically processed by adding a butyl group to produce a quaternary ammonium structure. This modification forms a molecule that still has anticholinergic properties comparable to those of hyoscine.
But unlike hyoscine, quaternary ammonium compounds such as hyoscine butyl bromide limit systemic absorption and significantly reduce the number of adverse reactions. Hyoscine butyl bromide is an anticholinergic drug with a high degree of affinity for muscarinic receptors located on the smooth muscle cells of the gastrointestinal tract, causing an antispasmodic effect. In addition, the drug binds to nicotinic receptors, which determines the effect of blocking the nerve ganglia, which determines its antisecretory effect.
The technical side of the study differs little from the above-mentioned AChT test. At the end of standard hepatobiliscintigraphy, instead of infusion of an amino acid solution, the patient takes 20 mg of hyoscine butyl bromide per os. After 20 minutes, the data is re-recorded and processed (Fig. 11). Thus, the use of the Buscopan® test reduces diagnostic time for the doctor and simplifies the diagnostic procedure for the patient.
GBSG with the Buscopan® test has proven itself to be most effective in the study of patients after cholecystectomy (Fig. 12).
The leading factors of liver dysfunction after cholecystectomy are the presence and duration of dyskinesia of the sphincter apparatus of the biliary tract. In patients, paradoxical spasm of the sphincter of Oddi significantly predominates as the cause of delay of radiopharmaceuticals in the common bile duct. Functional disorders of bile outflow are caused by cholesterosis of the biliary tract, in particular the sphincter of Oddi (Fig. 13, 14).
X-ray methods
X-ray methods for studying the gallbladder and extrahepatic bile ducts are practically not used today, so we provide a brief description of them as a historical reference.
Survey radiography
Plain radiography of the abdominal cavity is performed much less frequently than ultrasound due to radiation exposure. But, nevertheless, it was a fairly informative method for diagnosing cholelithiasis. On the x-ray you can see the presence, location and number of x-ray stones containing calcium salts (Fig. 15).
Oral cholecystography
Oral cholecystography is performed if X-ray negative (cholesterol) stones are suspected. The method is based on absorption in the gastrointestinal tract and excretion of the contrast agent with bile (Fig. 16).
If absorption in the intestine is impaired, the excretory function of the liver is reduced, the cystic duct is blocked by a stone, etc., oral cholecystography may be negative, i.e., the shadow of the gallbladder is not detected on it.
Intravenous cholecystography
Intravenous cholecystography is performed if the result of the oral radiocontrast method is negative. Using this technique, it is possible to contrast the gallbladder in 80–90% of cases (Fig. 17).
Computed tomography and magnetic nuclear (magnetic resonance) imaging
The shortcomings of classical X-ray studies of the gallbladder are successfully compensated by computed tomography (CT) and magnetic nuclear tomography (magnetic resonance imaging, MRI). In calculous cholesterosis, stones are visualized as shadows of a homogeneous structure (cholesterol stones) (Fig. 18) or are represented by heterogeneous shadows with alternating areas of mixed stones - a cholesterol core with a calcium-bilirubin shell (Fig. 19).
Computed tomography and magnetic nuclear tomography make it possible to suspect cholelithiasis in patients examined for other pathologies of the abdominal organs, since a description of the image of the gallbladder is a mandatory component of the protocol for these studies.
Literature
- Practical guide to ultrasound diagnostics. Ed. V.V. Mitkova. M.: Vidar-M, 2003. T. 1. 720 p.
- Brant WE, Helms CA Fundamentals of Diagnostic Radiology, 2nd ed. Lippincott, Williams and Wilkins, p. 836–841.
- Kurtz AB, Middleton WD Ultrasound: The Requisites. Philadeiphia, Hanley & Belfus, 1996, p. 35–71.
- Parulekar SG Transabdominal sonography of bile ducts // Ultrasound Q. 2002, (18) 3: 187–202.
- Rumack CM, Wilson SR, Charboneau JW (eds). Diagnostic Ultrasound, 2nd ed. St. Louis, Mosby, 1998, p. 172–195.
- Savelyev V. S., Petukhov V. A. Cholelithiasis and indigestion syndrome. M.: BORGES, 2010. 258 p.
- Savelyev V. S., Petukhov V. A., Boldin B. V. Cholesterosis of the gallbladder. M.: VEDI, 2002., 176 p.
- Vysotskaya R. A. Prostaglandins and gastrointestinal hormones in chronic liver diseases. Diss. doc. biol. Sci. M., 1992, 340 p.
- Houda R., Tooli J., Dodds WJ Effect of enteric hormons on sphincter of Oddi and gastrointestinal myoelectric activity in fasted conscious opossums // Gastroenterol. 1983, vol. 84, p. 1–9.
- Weechsler-JG Bedeutung der Gallenblase in der Regulation des duodenogastralen Refluxes // Z-Gastroenterol. 1987, Aug. 25, Suppl 3: p. 15–21.
- Petukhov V. A. Lipid distress syndrome. Ed. V. S. Savelyeva, M.: MAX PRESS, 2010. 544 p.
V. A. Petukhov*, 1, Doctor of Medical Sciences, Professor D. A. Churikov**, Candidate of Medical Sciences
* GBOU VPO RNIMU im. N. I. Pirogova Ministry of Health of the Russian Federation, Moscow ** State Clinical Hospital No. 1 named after. N. I. Pirogova, Moscow
1 Contact information
How is an ultrasound of the gallbladder performed?
There are two directions for performing ultrasound of the gallbladder - abdominal and ultrasound of the gallbladder with a functional test.
Abdominal ultrasound of the gallbladder
An abdominal ultrasound of the gallbladder is a simple scanning method. It takes place in one stage and requires less time. The patient will have to remove clothing from the abdominal area and lie down on the couch. The diagnostician lubricates the device's sensor and the patient's examination area with a water-based gel. This will make it easier to glide during the examination and will prevent the formation of an air gap between the body and the sensor, which in turn will increase the passage of ultrasonic waves to the organ. The ultrasound procedure usually takes place in the supine position, but if the examination is interfered with by intestinal loops that may cover the organ, the sonologist asks the patient to take a deep breath and not exhale for as long as possible. In cases where the patient needs to be checked for the presence of stones or sand, the diagnostician asks the patient to bend forward several times from a standing position.
Ultrasound of the gallbladder with functional test
The second research method is carried out to determine the function of the gallbladder in real time. This method is called ultrasound of the gallbladder with a functional test, ultrasound with a choleretic breakfast, or echocholescintigraphy. This scanning is carried out in two stages. The first, the basic stage, includes a simple abdominal examination on an empty stomach. After it, the patient eats a choleretic breakfast (250 grams of cottage cheese, 2 egg yolks), and the diagnostician repeats the scan with a time interval of 5-10-15 minutes. This gives a chance to track and analyze the contractile function of the organ.
Ultrasound after gallbladder removal
If a patient's gallbladder has been removed, ultrasound diagnostics also takes place in several steps. The first step, on an empty stomach, the doctor assesses the condition of the bile ducts and their diameter, and the second step carries out diagnostics after a food load. First, the subject drinks a sorbitol solution, and then the doctor performs an ultrasound scan half an hour and an hour after taking the drug. During the second stage, the doctor records all the patient’s complaints about pain, type and characteristics, duration, intensity or complete absence of pain.
Contraindications
This diagnostic method has no contraindications, with the exception of diseases or injuries of the skin in the abdominal area. For high-quality ultrasound diagnostics, good contact of the sensor with the patient’s skin is necessary. The presence of tuberosity of the skin does not allow this to be achieved. As a result, image quality decreases and ultrasound data may be uninformative.
Previous Next
How to prepare for an ultrasound of the gallbladder?
Preparation for an ultrasound of the gallbladder is required, but it is simple and does not differ fundamentally from the organizational issues associated with preparation for any other type of ultrasound of the abdominal cavity and retroperitoneal space. Diet. 3 days before the scan, you should start by changing your usual diet to a special diet that excludes foods that cause gas formation in the intestines. You should not eat yeast-based baked goods, carbonated and alcoholic drinks, kefir, milk and other fermented milk products, peas and legumes, raw fruits and vegetables, and coffee. Boiled foods, porridge cooked without milk, lean meat, chicken or fish are suitable for the menu these days. Drugs. On diet days, you should start taking activated carbon at the rate of 1 tablet per 10 kg of weight. You can take charcoal at once or divide it into several servings. As an alternative to activated carbon, such drugs as Smecta, Mezim-Forte, Espumisan, and Motilium are suitable. The choice of enzyme preparations in pharmacies is large. Colon cleansing. It is advisable to cleanse the intestines naturally on the day of screening. Only in case of constipation, a small enema can be used for cleaning. Starvation. An ultrasound scan of the gallbladder is performed strictly on an empty stomach, since even a small amount of water drunk will cause the gallbladder to contract, and this will significantly complicate the diagnostic process. If the scan is scheduled in the morning, then breakfast should be canceled; if in the afternoon, a small snack is allowed 6 hours before the procedure. This can be unsweetened tea and a small cracker.
Decoding and norm
Normally, on ultrasound, the gallbladder should have a pear-shaped or oval shape with smooth and clear contours.
Any deformation of the shape or contour of an organ will indicate pathology. For example, acute cholecystitis will manifest itself as increased blood flow, thickening of the walls, multiple internal partitions and enlargement of the organ itself. In chronic cholecystitis, the size of the gallbladder will be smaller than normal, the walls are thickened and deformed, the contours are not clearly visible, and there are small inclusions. If a bend in the gallbladder and increased wall tone are visualized, this indicates dyskinesia. The final diagnosis based on the screening results can only be made by a specialized specialist. It is to him that the patient should go after the sonologist gives him the examination protocol.
Author: Telegina Natalya Dmitrievna
Therapist with 25 years of experience
>
Decoding the results
During the procedure, the following indicators are assessed:
- organ location and mobility;
- shape, dimensions, wall thickness;
- diameter of the bile ducts;
- contractile function;
- the presence of stones, polyps, neoplasms.
Normal gallbladder parameters
Norm of the gallbladder on ultrasound in adults:
- length – from 7 to 10 cm;
- width – up to 3 cm;
- transverse size – from 3 to 3.5 cm;
- volume – from 30 to 70 cm3;
- wall thickness – up to 4 mm;
- the common bile duct in diameter is up to 6 mm in the presence of a gallbladder; with a removed gallbladder - up to 9 mm;
- internal diameter of the lobar bile ducts – up to 3 mm;
- gallbladder shape – pear-shaped or oval;
- the contours are clear;
- the bottom of the bladder may protrude from under the lower edge of the liver by 1-1.5 cm.
What does an ultrasound of the gallbladder show?
An ultrasound will show deformation of the gallbladder. The following gallbladder diseases can also be detected using ultrasound:
- acute cholecystitis;
- chronic cholecystitis;
- gallbladder dyskinesia;
- cholelithiasis (cholelithiasis);
- gallbladder polyps;
- tumors (formation larger than 1-1.5 cm);
- congenital anomalies (agenesis - absence of the gallbladder, ectopic localization - atypical location of the gallbladder, for example, retroperitoneal or between the diaphragm and the right lobe of the liver).
results of the gallbladder
, decoding, norms are individual in nature and therefore you should entrust this to doctors and not try to interpret the results yourself. To clarify the detected pathologies and monitor the dynamics after the first ultrasound, a repeat ultrasound may be prescribed in 1-3 months.