Bitterness in the mouth, nagging pain in the right hypochondrium, nausea may indicate cholelithiasis. Why can't you just remove the stones and save the gallbladder? And how does life change after cholecystectomy? Frequent questions from patients are answered by Mikhail Vladimirovich Kosachenko, laparoscopic surgeon, candidate of medical sciences, head of the operating unit of the City Clinical Hospital named after. V.V. Vinogradova.
Why does the gallbladder become inflamed?
Inflammation, or cholecystitis, occurs due to a violation of the outflow of bile and the presence of pathogenic microflora in the wall of the bladder. The flow of bile can be disrupted for two reasons:
Gallstones.
They are formed due to hormonal imbalance and/or bile acid metabolism and high cholesterol content in bile.
Biliary dyskinesia.
Violation of their contractile function leads to stagnation of bile - cholestasis. Against this background, cholecystitis can also develop.
Laparoscopic cholecystectomy
Cholecystectomy is an operation to remove the gallbladder. During cholecystectomy, the pathologically altered gallbladder is completely removed through surgery.
The question often arises: is the gallbladder really so unnecessary for a person that it can be painlessly removed? A healthy gallbladder is a truly necessary organ that takes part in digestion. When food enters the duodenum from the stomach, the gallbladder contracts and 40-60 ml of bile is injected into the intestine. It mixes with food, taking part in digestion. However, a pathologically altered gallbladder does not function normally, but, on the contrary, causes more problems: pain, maintaining a chronic reservoir of infection, dysfunction of both the biliary (biliary) system and the pancreas. Therefore, cholecystectomy, performed according to indications, improves the patient’s condition and does not significantly affect digestive function.
According to foreign and domestic literature, in 90-95% of patients, cholecystectomy completely cures the symptoms that were observed before surgery.
People with a removed gallbladder observe certain food restrictions (diet) for the first 2-4 months while the body adapts to changes in the functioning of the biliary system. During this period, it is possible (but not necessary) for stool to loosen or become more frequent up to 2-3 times a day. 4-6 months after surgery, a person can lead a normal life, with virtually no restrictions. However, in some patients in whom the disease has lasted a long time and is complicated by damage to associated organs (chronic pancreatitis, cholangitis, etc.), some of the symptoms cannot be eliminated by cholecystectomy and they require further treatment. This is another argument in favor of timely surgical treatment of gallbladder diseases.
Indications for laparoscopic cholecystectomy
The main indications for removal of the gallbladder are complicated forms of cholelithiasis, as well as some other diseases of the gallbladder:
Acute cholecystitis
Mortality in acute cholecystitis reaches 1-6%; as the disease progresses without adequate treatment, serious complications may develop: necrosis and perforation of the gallbladder wall; purulent inflammation of the peritoneum (peritonitis); formation of intra-abdominal abscesses; sepsis. The presence of acute cholecystitis against the background of cholelithiasis most often requires urgent surgery.
Choledocholithiasis
Choledocholithiasis occurs in 5-15% of patients with cholelithiasis, it leads to the development of severe complications: obstructive jaundice (blockage of the bile ducts with impaired outflow of bile); cholangitis (inflammation of the bile ducts); biliary pancreatitis. Concomitant choledocholithiasis in cholelithiasis requires expanding the scope of surgical intervention: performing sanitation of the bile ducts (either endoscopically or intraoperatively), with the possible leaving of bile duct drainages for a long time.
Symptomatic cholelithiasis
The presence of painful attacks of biliary colic against the background of cholelithiasis is an absolute indication for surgical treatment. This is due to the fact that 69% of patients have a second attack of biliary colic within 2 years, and 6.5% of patients develop severe complications within 10 years after the first attack.
An indication for surgical treatment is also gallstone disease with so-called “minor” symptoms (a feeling of heaviness in the hypochondrium after eating, bitterness in the mouth, periodic aching pain in the right hypochondrium). Conditions requiring emergency surgery occur in 6-8% of such patients per year, and serious complications occur in 1-3% of patients per year.
Asymptomatic gallstone disease
Stone-carrying or asymptomatic cholelithiasis is much more common than thought 30-40 years ago, which is primarily due to improved diagnosis, as well as the nutritional and lifestyle characteristics of modern humans. Some time ago, the indication for cholecystectomy for asymptomatic cholelithiasis was considered to be the risk of developing gallbladder cancer, but in most countries (with the exception of Chile) it is low and is not considered a significant factor. 1-2% of patients per year become symptomatic and 1-2% per year develop serious complications. Most patients with asymptomatic stones live without surgical treatment for 15-20 years. Currently, indications for surgical treatment of patients with asymptomatic cholelithiasis are: hemolytic anemia; stones larger than 2.5-3 cm (due to the risk of pressure sores of the gallbladder wall), combined operation during surgical interventions for obesity (due to the risk of worsening the course of the disease with rapid weight loss); The patient's life expectancy is more than 20 years (due to a cumulatively high complication rate).
For asymptomatic stones, cholecystectomy is contraindicated in patients with diabetes mellitus and liver cirrhosis; in patients during and after organ transplantation (due to the increased risk of complications).
Gallbladder cholesterosis
Gallbladder cholesterosis is the deposition of cholesterol in the wall of the organ. Cholesterosis against the background of cholelithiasis is an indication for surgical treatment; non-calculous cholesterosis without dysfunction of the gallbladder is subject to conservative drug treatment, with dysfunction - cholecystectomy.
A separate nosology, which is an absolute indication for surgery, is calcification (calcification) of the gallbladder wall, or “porcelain gallbladder.” This is due to the high risk of developing cancer (25%).
Gallbladder polyps
Gallbladder polyps up to 10 mm in size detected by ultrasound are subject to dynamic monitoring, with ultrasound control once every 6 months. Indications for surgery are polyps associated with cholelithiasis, polyps larger than 10 mm in size or having a vascular pedicle (their malignancy rate is 10-33%).
Functional gallbladder disorder
A common indication for cholecystectomy (about 25% of all operations) abroad is a functional disorder of the gallbladder, which consists of the presence of pain symptoms in the absence of gallstones, biliary sludge or microlithiasis. Moreover, according to international standards (Rome III consensus), a change in gallbladder ejection fraction of less than 40% should be detected when using a continuous intravenous infusion of cholecystokinin octapeptide over a 30-minute period and a positive therapeutic response with no relapse more than 12 months after cholecystectomy.
In our country, the majority of gastroenterologists and surgeons are of the opinion that it is inappropriate to perform operations on such patients.
Contraindications to laparoscopic cholecystectomy
If open cholecystectomy can be performed for health reasons in the vast majority of patients, then laparoscopic cholecystectomy has both absolute and relative indications.
Absolute contraindications to laparoscopic cholecystectomy are terminal conditions of the patient, decompensation of the functions of vital organs and systems, uncorrected blood clotting disorders.
Relative contraindications are usually determined by the experience of the surgeon, the equipment of the clinic and the individual characteristics of the patients. These are acute cholecystitis with a disease duration of more than 72 hours, widespread peritonitis, pregnancy in the 1st and 3rd trimester, Mirizzi syndrome, scleroatrophic gallbladder, previous operations on the upper floor of the abdominal cavity, infectious diseases, large hernias of the anterior abdominal wall.
The issue of contraindications to laparoscopic cholecystectomy is decided jointly by the surgeon and anesthesiologist.
Comparative characteristics of cholecystectomy techniques.
Currently, our hospital performs several cholecystectomy technologies:
- Laparoscopic
- Minimally invasive open
- Traditional open
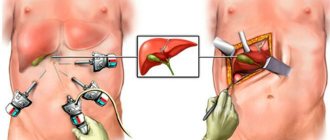
Laparoscopic cholecystectomy is the “gold standard” in the treatment of chronic cholecystitis and the option of choice in the treatment of acute cholecystitis. It is performed using special instruments through 3-4 punctures in the abdominal wall with a diameter of 5-10 mm. Special tubes (trocars) are inserted into these punctures, and carbon dioxide is injected into the abdominal cavity using an insufflator (pump) - pneumoperitoneum is applied. The introduced gas creates space for the tools to work. Through trocars, with the help of a video camera and special clamps and electrodes, the anatomical elements of the gallbladder - the cystic artery and cystic duct - are isolated, special metal brackets (clips) are placed on them and crossed. Modern video systems provide excellent image quality and visualization of structures, far superior to those in open operations. The gallbladder is separated from the liver and removed through one of the punctures in the abdominal wall.
The advantages of laparoscopic cholecystectomy are minimal trauma to the abdominal wall, virtually no pain, a quick recovery period after surgery, a short hospital stay (1-2 days), quick recovery and return to daily activities and work.
Unfortunately, in 1-5% of cases it is impossible to perform cholecystectomy from a laparoscopic approach. Most often this is due to anatomical abnormalities of the biliary tract, a pronounced inflammatory or adhesive process, and the development of intraoperative complications. In such cases, a transition to open surgery (conversion) is performed, most often to minimally invasive surgery, or, less commonly, to traditional open surgery.
Minimally invasive open cholecystectomy has been used since the 70s of the last century to minimize trauma to the abdominal wall. The gallbladder is removed from a 3-7 cm long incision in the right hypochondrium.
Its advantages are: significantly less trauma to the anterior abdominal wall than with open cholecystectomy; the possibility of performing the intervention in patients who have previously undergone abdominal surgery; direct visual control and the use of traditional techniques of surgical tissue dissection, which allow relatively safe manipulation in conditions of severe infiltration.
Minimally invasive open cholecystectomy is indicated in cases where, due to concomitant diseases, the application of pneumoperitoneum and, therefore, laparoscopic surgery is contraindicated.
With any version of cholecystectomy from a mini-access, the length of stay of patients in the hospital is usually longer than with laparoscopy, and is 3-5 days. The postoperative rehabilitation period is also longer.
Traditional open cholecystectomy is performed through an upper median laparotomy or oblique subcostal incisions such as the Kocher and Fedorov approaches, which provide wide access to the gallbladder, extrahepatic bile ducts, liver, pancreas, and duodenum. With such approaches, all methods of intraoperative inspection of the extrahepatic bile ducts are feasible, including measuring their width, probing the ducts, intraoperative cholangiography, intraoperative ultrasound, choledochotomy with intraoperative choledochoscopy, etc.
Currently, cholecystectomy from a wide laparotomy approach is most often performed in patients with acute cholecystitis, which is complicated by widespread peritonitis, or in complex forms of bile duct pathology.
Its disadvantages are: significant trauma to the structures of the anterior abdominal wall, a significant number of early and late wound complications (in particular, postoperative ventral hernias); moderate surgical trauma leading to the development of postoperative intestinal paresis, impaired external respiration function, and limitation of the patient’s physical activity; significant cosmetic defect; long period of post-anesthesia and post-operative rehabilitation and disability.
Fundamentally, in all technologies, the only thing that is different is access. With any method of cholecystectomy, the cystic duct and cystic artery are surgically isolated, crossed and ligated or clipped, the gallbladder is separated from the liver, the gallbladder bed is treated, the gallbladder is removed from the abdominal cavity, and, if necessary, the abdominal cavity is drained.
The main question that patients ask and the surgeon asks himself is what surgical technology to choose? There is no definite answer to this; it is necessary to select the optimal technology for each individual patient, depending on the characteristics of his disease, concomitant pathology, and general health. The most general recommendations are: for chronic cholecystitis and gallbladder polyps, the method of choice is laparoscopic cholecystectomy, for an acute process - laparoscopic or minimally invasive open, for the development of peritonitis (purulent inflammation of the peritoneum) - open. In patients for whom laparoscopy is contraindicated due to concomitant pathology or previous abdominal surgery, the method of choice is cholecystectomy from a mini-access. In case of pathology of the biliary tract, it is possible to use different cholecystectomy technologies in combination with endoscopic sanitation of the bile ducts.
The choice of surgical intervention technology is made jointly by the surgeon, anesthesiologist and patient.
Necessary examinations for surgery.
Before the operation, you must undergo a series of examinations that will assess your body’s readiness for intervention and identify possible complicated forms of gallstone disease and concomitant diseases. The scope of examinations includes:
- General physical examination.
- Determination of blood group and Rh factor.
- Express tests for syphilis, hepatitis B and C.
- General clinical blood and urine tests.
- Blood glucose.
- Biochemical blood test (total protein, creatinine, bilirubin, liver tests - ALT, AST, GGTP).
- Coagulogram.
- Ultrasound examination of the liver, bile ducts and pancreas.
- Electrocardiography.
- Fluorography or radiography of the chest organs.
- Examination by a therapist and other specialized specialists (as indicated).
- Esophagogastroduodenoscopy.
- Colonoscopy according to indications.
Also, if indicated, a more in-depth examination of the condition of the bile ducts is possible: magnetic resonance cholangiography, endoultrasonography, endoscopic retrograde cholangiopancreatography.
Preparing for surgery.
Preparation for surgery includes:
- Light food on the day before surgery with the last meal before 19.00.
- Cleansing enema (possibly using the drug Normacol) in the evening and morning before surgery.
- Espumisan 1 tablet 3 times a day two days before surgery (according to indications).
- Shower (in the morning before surgery).
On the day of the operation, consuming food and drinks is prohibited. If you need to take medications, you should consult your doctor.
In some cases, special preoperative treatment of concomitant diseases is necessary.
Brief description of the operation and its possible options.
Laparoscopic cholecystectomy is performed under general anesthesia: the patient falls asleep before the intervention begins and wakes up after its completion.
The duration of laparoscopic cholecystectomy can be from 20 minutes to 1.5-2 hours, depending on the complexity of the intervention, the characteristics of the anatomy and pathological process, and the experience of the surgeon. On average, the operation lasts about 40 minutes.
First, using a special instrument - a Veress needle - carbon dioxide is injected into the abdominal cavity (carboxyperitoneum is applied). This is necessary in order to raise the abdominal wall and create space inside the abdomen for using instruments. Pressure in the abdominal cavity is maintained by an insufflator, a device that pumps CO2 into the abdomen and maintains a constant pressure of the gas, usually 12 mmHg. Then trocars are inserted - special tubes with valves that pierce the abdominal wall and allow the insertion of instruments without loss of gas. A laparoscope, an optical tube to which a video camera is connected, is inserted into the umbilical area. The surgeon, his assistant and the entire operating team see the entire progress of the operation on special monitors. The laparoscope provides a 40-fold magnification, so the visibility of organs and structures, and the features of the operation during laparoscopic surgery is better than during open operations. Instruments for manipulation are inserted into the remaining 3 trocars: clamps that hold the gallbladder, and a special electrode, with the help of which the gallbladder, the cystic artery (supplying it with blood) and the cystic duct (connecting the gallbladder with the bile ducts) are isolated by electrocoagulation. After isolating and clearly identifying all anatomical structures, the cystic artery and duct are clipped (clamped with special titanium latches - clips). Clips are a reliable and safe replacement for threads used to bandage these structures during open operations. After crossing the clipped structures, the gallbladder is separated from the liver, the reliability of stopping possible bleeding is checked, the subhepatic and suprahepatic spaces are washed, and the gallbladder is removed. The gallbladder is removed through the trocar insertion site in the upper abdomen, under the xiphoid process, or, in some cases, through an umbilical incision. In most cases, a 10-12 mm incision is sufficient to remove the gallbladder, but in some situations the incision size must be expanded to 20-30 mm. Most often, the stones are crushed into small pieces in the lumen of the gallbladder, so the patient during laparoscopic cholecystectomy cannot always see them after the operation (unlike the open technique).
It is possible to complete the operation without draining the abdominal cavity, however, in many cases, surgeons leave a polyvinyl chloride or silicone tube in the subhepatic space, brought out through the side of the abdominal wall. The tube (drainage) serves to drain fluid that may accumulate in the abdomen after surgery as a result of surgical trauma.
The postoperative period is a stay in the hospital.
After a routine uncomplicated laparoscopic cholecystectomy, the patient is transferred from the operating room to the intensive care unit, where he spends the next 2 hours of the postoperative period to monitor adequate recovery from the state of anesthesia. In the presence of concomitant pathology or characteristics of the disease and surgical intervention, the duration of stay in the intensive care unit may be increased. The patient is then transferred to a ward where he receives the prescribed postoperative treatment. During the first 4-6 hours after surgery, the patient should not drink or get out of bed. Until the morning of the next day after the operation, you can drink plain water without gas, in portions of 1-2 sips every 10-20 minutes with a total volume of up to 500 ml. The patient can get up 4-6 hours after surgery. You should get out of bed gradually, first sit for a while, and, in the absence of weakness and dizziness, you can get up and walk around the bed. It is recommended to get up for the first time in the presence of medical personnel (after a long stay in a horizontal position and after the action of medications, orthostatic collapse - fainting) is possible.
The next day after the operation, the patient can move freely around the hospital, begin to take liquid food: kefir, oatmeal, diet soup and switch to the usual regime of drinking liquids. In the first 7 days after surgery, the consumption of any alcoholic beverages, coffee, strong tea, drinks with sugar, chocolate, sweets, fatty and fried foods is strictly prohibited. The patient's diet in the first days after laparoscopic cholecystectomy may include fermented milk products: low-fat cottage cheese, kefir, yogurt; porridge with water (oatmeal, buckwheat); bananas, baked apples; mashed potatoes, vegetable soups; boiled meat: lean beef or chicken breast.
In the normal course of the postoperative period, the drainage from the abdominal cavity is removed the next day after surgery. Removing the drainage is a painless procedure; it is performed during dressing and takes a few seconds.
Young patients after surgery for chronic calculous cholecystitis can be sent home the next day after surgery; other patients are usually in the hospital for 2 days. Upon discharge, you will be given a certificate of incapacity for work (if you need one) and an extract from the inpatient card, which will outline your diagnosis and features of the operation, as well as recommendations on diet, physical activity and drug treatment. A certificate of incapacity for work is issued for the duration of the patient’s stay in the hospital and for 3 days after discharge, after which the issue of its extension is decided by the surgeon at the clinic at your place of residence.
Postoperative period – the first month after surgery.
In the first month after surgery, the functions and general condition of the body are restored. Careful adherence to medical recommendations is the key to full recovery of health. The main areas of rehabilitation are adherence to physical activity, diet, drug treatment, and wound care.
Compliance with physical activity regimen.
Any surgical intervention is accompanied by tissue trauma and anesthesia, which requires restoration of the body. The usual rehabilitation period after laparoscopic cholecystectomy ranges from 7 to 28 days (depending on the nature of the patient's activity). Despite the fact that 2-3 days after the operation the patient feels satisfactory and can walk freely, walk on the street, even drive a car, we recommend staying at home and not going to work for at least 7 days after the operation, which is required for the body to recover. . At this time, the patient may feel weakness and increased fatigue.
After surgery, it is recommended to limit physical activity for a period of 1 month (do not carry weights of more than 3-4 kilograms, exclude physical exercises that require tension in the abdominal muscles). This recommendation is due to the peculiarities of the formation of the scar of the muscular aponeurotic layer of the abdominal wall, which reaches sufficient strength within 28 days from the moment of surgery. 1 month after surgery there are no restrictions on physical activity.
Diet.
Compliance with the diet is required for up to 1 month after laparoscopic cholecystectomy. It is recommended to exclude alcohol, easily digestible carbohydrates, fatty, spicy, fried, spicy foods, and regular meals 4-6 times a day. New foods should be introduced into the diet gradually; 1 month after surgery, dietary restrictions may be lifted on the recommendation of a gastroenterologist.
Drug treatment.
Minimal medical treatment is usually required after laparoscopic cholecystectomy. Pain syndrome after surgery is usually mild, but some patients require the use of analgesics for 2-3 days. Usually this is ketanov, paracetamol.
In some patients, it is possible to use antispasmodics (no-spa or drotaverine, buscopan) for 7-10 days.
Taking ursodeoxycholic acid preparations (ursofalk) can improve the lithogenicity of bile and eliminate possible microcholelithiasis.
Taking medications should be carried out strictly as directed by the attending physician in an individual dosage.
Care of postoperative wounds.
In the hospital, special stickers will be applied to postoperative wounds located at the places where instruments are inserted. It is possible to take a shower with Tegaderm stickers (they look like a transparent film), while Medipore stickers (a white patch) must be removed before showering. You can shower starting 48 hours after surgery. Getting water on the seams is not contraindicated, but you should not wash the wounds with gels or soaps or rub them with a washcloth. After taking a shower, you should lubricate the wounds with a 5% iodine solution (or betadine solution, or brilliant green, or 70% ethyl alcohol). Wounds can be treated using the open method, without dressings. Taking baths or swimming in pools and ponds is prohibited before the sutures are removed and for 5 days after the sutures are removed.
Sutures after laparoscopic cholecystectomy are removed 7-8 days after surgery. This is an outpatient procedure, the sutures are removed by a doctor or a dressing nurse, and the procedure is painless.
Possible complications of cholecystectomy.
Any operation may be accompanied by undesirable effects and complications. Complications are possible after any cholecystectomy technology.
Complications from wounds.
These may be subcutaneous hemorrhages (bruises) that go away on their own within 7-10 days. No special treatment is required.
There may be redness of the skin around the wound and the appearance of painful lumps in the wound area. Most often this is due to wound infection. Despite the ongoing prevention of such complications, the incidence of wound infection is 1-2%. If such symptoms appear, you should consult a doctor as soon as possible. Late treatment can lead to suppuration of the wounds, which usually requires surgical intervention under local anesthesia (debridement of the festering wound) followed by dressings and possible antibiotic therapy.
Despite the fact that our hospital uses modern high-quality and high-tech instruments and modern suture material, in which wounds are sutured with cosmetic sutures, hypertrophic or keloid scars may form in 5-7% of patients. This complication is associated with the individual characteristics of the patient’s tissue reaction and, if the patient is dissatisfied with the cosmetic result, may require special treatment.
In 0.1-0.3% of patients, hernias may develop at the sites of trocar wounds. This complication is most often associated with the characteristics of the patient’s connective tissue and may require surgical correction in the long term.
Complications from the abdominal cavity.
Very rarely, complications from the abdominal cavity are possible, which may require repeated interventions: either minimally invasive punctures under ultrasonography guidance, or repeated laparoscopies or even laparotomies (open operations on the abdominal cavity). The frequency of such complications does not exceed 1:1000 operations. These may be intra-abdominal bleeding, hematomas, purulent complications in the abdominal cavity (subhepatic, subphrenic abscesses, liver abscesses, peritonitis).
Residual choledocholithiasis.
According to statistics, from 5 to 20% of patients with cholelithiasis also have concomitant stones in the bile ducts (choledocholithiasis). A set of examinations carried out in the preoperative period is aimed at identifying such a complication and using adequate treatment methods (this can be retrograde papillosphincterotomy - dissection of the mouth of the common bile duct endoscopically before surgery, or intraoperative revision of the bile ducts with removal of stones). Unfortunately, none of the methods of preoperative diagnosis and intraoperative assessment is 100% effective in identifying stones. In 0.3-0.5% of patients, stones in the bile ducts may not be detected before and during surgery and cause complications in the postoperative period (the most common of which is obstructive jaundice). The occurrence of such a complication requires endoscopic (using a gastroduodenoscope inserted through the mouth into the stomach and duodenum) intervention - retrograde papilosphinctoromy and transpapillary sanitation of the bile ducts. In exceptional cases, repeated laparoscopic or open surgery is possible.
Bile leakage.
Bile leakage through drainage in the postoperative period occurs in 1:200-1:300 patients; most often it is a consequence of the release of bile from the gall bladder bed on the liver and stops on its own after 2-3 days. This complication may require an extended hospital stay. However, bile leakage through drainage can also be a symptom of damage to the bile ducts.
Damage to the bile ducts.
Damage to the bile ducts is one of the most severe complications in all types of cholecystectomy, including laparoscopic. In traditional open surgery, the incidence of severe bile duct injury was 1 in 1500 operations. In the first years of mastering laparoscopic technology, the frequency of this complication increased 3 times - up to 1:500 operations, however, with the growing experience of surgeons and the development of technology, it stabilized at the level of 1 in 1000 operations. A well-known Russian specialist on this problem, Eduard Izrailevich Galperin, wrote in 2004: “... Neither the duration of the disease, nor the nature of the operation (emergency or planned), nor the diameter of the duct and even the professional experience of the surgeon affect the possibility of damage to the ducts...”. The occurrence of such a complication may require repeated surgery and a long period of rehabilitation.
Allergic reactions to medications.
The trend in the modern world is an ever-increasing allergization of the population, therefore allergic reactions to medications (both relatively mild - urticaria, allergic dermatitis) and more severe (Quincke's edema, anaphylactic shock). Despite the fact that in our clinic allergological tests are carried out before prescribing medications, allergic reactions are possible, and additional drug treatment is required. Please, if you know about your personal intolerance to any medications, be sure to tell your doctor about it.
Thromboembolic complications.
Venous thrombosis and pulmonary embolism are life-threatening complications of any surgical procedure. That is why great attention is paid to the prevention of these complications. Depending on the degree of risk determined by your attending physician, preventive measures will be prescribed: bandaging the lower extremities, administering low molecular weight heparins.
Exacerbation of peptic ulcer of the stomach and duodenum.
Any, even minimally invasive, operation is stressful for the body and can provoke an exacerbation of gastric and duodenal ulcers. Therefore, in patients at risk of such a complication, prophylaxis with antiulcer drugs in the postoperative period is possible.
Despite the fact that any surgical intervention carries a certain risk of complications, refusing or delaying the operation also carries a risk of developing severe illness or complications. Despite the fact that hospital doctors pay great attention to the prevention of possible complications, the patient plays a significant role in this. Performing cholecystectomy in a planned manner, with non-advanced forms of the disease, carries a much lower risk of unwanted deviations from the normal course of the operation and the postoperative period. The patient’s responsibility for strict adherence to the regimen and doctors’ recommendations is also of great importance.
Long-term rehabilitation after cholecystectomy.
Most patients after cholecystectomy are completely cured of the symptoms that bothered them and return to normal life 1-6 months after the operation. If cholecystectomy is performed on time, before the occurrence of concomitant pathology from other organs of the digestive system, the patient can eat without restrictions (which does not negate the need for proper healthy nutrition), not limit himself in physical activity, and not take special medications. If the patient has already developed concomitant pathology of the digestive system (gastritis, chronic pancreatitis, dyskinesia), he should be under the supervision of a gastroenterologist in order to correct this pathology. A gastroenterologist will give you recommendations on lifestyle, diet, dietary habits and, if necessary, drug treatment.
* prepared using materials from the website www.chirurg.com.
Is it possible to remove only the stones and leave the gallbladder itself?
No you can not. There is no such treatment method anywhere in the world. If stones have formed in the gallbladder, then its functioning is no longer adequate, and there is a chronic infection in it. Conservative therapy can be prescribed for a while, but such practice will not lead to a cure.
Don't let things get to the point of acute cholecystitis. If something bothers you, you should not take painkillers, but deal with the cause. In acute inflammation, the bladder is damaged to the point of necrosis of the wall. These are completely different conditions for the surgeon’s work and the patient’s recovery than during a planned operation.
Forms of PCES
The following variants of PCES are distinguished:
- spastic variant
- variant with CO deficiency, chronic biliary insufficiency and fat digestion disorders
- variant with SIBO, duodenal hypertension, sphincter of Oddi dysfunction (SOD), stagnation of bile in the ducts
- variant with SO dysfunction, with chronic biliary insufficiency, fat digestion disorder, intestinal hypertension, SO spasm
- the same with duodenogastric reflux, reflux gastritis.
Factors influencing the formation of PCES can be divided into two main groups:
- Contributing (sphincter of Oddi dysfunction - DSO).
- Allowing:
- bacterial overgrowth syndrome
- duodenal hypertension (increased pressure in the duodenum)
- chronic biliary insufficiency
- intestinal and abdominal hypertension (increased pressure in the intestines and abdominal cavity)
- duodenogastric reflux.
How is gallbladder removal surgery performed?
In most cases, laparoscopic cholecystectomy is performed. This is the removal of the gallbladder through four punctures in the abdomen, 5 to 10 millimeters wide. The second option is a classic open cholecystectomy through an incision in the right hypochondrium.
And another option, which is used in few places except our hospital, is mini-laparoscopic cholecystectomy. In this case, the minimum puncture size is 3 millimeters. The maximum cosmetic effect is achieved and there is virtually no pain. It is important to note: the choice of surgical method remains with the surgeon, depending on the specific situation.
Recommendations after pancreas removal
As already mentioned, the need for surgical intervention and the advisability of organ removal depend entirely on the diagnosis and condition of the patient.
Is it possible to live without the pancreas if it is completely removed? Of course, it is possible, but provided that the person receives adequate replacement therapy. This means that all enzymes and hormones that the pancreas produces must be obtained by the body in the form of medications.
At the same time, future life expectancy is influenced by factors such as partial or complete resection of an organ, age, the condition of other digestive organs, and the presence of chronic concomitant pathologies. It also matters what disease the surgery was performed for (for example, a malignant tumor or a benign cyst).
It is necessary to mention that, in addition to the obvious advantages of radical treatment designed to save a person’s life, there are also some disadvantages of this method. First of all, this is the possibility of developing complications such as peritonitis, abscess, sepsis, diabetes mellitus, bleeding, and persistent intestinal disturbances.
In the vast majority of cases, the early postoperative period ends well, and after discharge from the hospital the patient receives the following recommendations:
- regular observation by an endocrinologist and gastroenterologist;
- constant replacement therapy with enzyme preparations;
- constant insulin therapy;
- daily self-regulation of blood sugar;
- strict nutritional control, a diet with significant restriction of fats and carbohydrates;
- absolute cessation of alcohol and smoking;
- regular physical activity of moderate intensity.
Compliance with these recommendations provides a person with many more years of a full and active life, as evidenced by reviews of patients who have undergone surgery on the pancreas or gall bladder.
Any alcoholic drinks after pancreatic surgery are prohibited
How is it possible to remove a gallbladder with stones through such small holes?
We make a centimeter incision above the navel and inflate the abdomen through it to create sufficient volume. We insert a special tube (trocar) into the same incision and install endovideosurgical optics. With its help we see everything that happens inside.
At the top of the abdomen we make three more incisions of 3 millimeters each and install thin trocars. Through them we insert instruments of the same diameter. Next, the cystic duct, cystic artery and the posterior wall of the gallbladder are separated from the bed by a third. Only then do we cross these structures.
The gallbladder is removed from the liver bed, and then, using certain surgical techniques, is removed from the abdominal cavity.
Nutrition
Since after the removal of the bile, the body is slowly rebuilt, which directly affects the functioning of the digestive tract, you will have to follow a special diet “table No. 5”, the purpose of which is to reduce the load on the liver and normalize the functions of the biliary system. It maintains optimal nutritional levels and satisfies the body's energy needs. The diet includes the required amount of proteins and carbohydrates, while reducing the amount of fat consumed.
The main principle is frequent, split meals every three hours in small portions. Food should be warm and taken at the same time. What is allowed:
- meat – lean beef, chicken, rabbit;
- fish - hake, cod, pike perch;
- cereals – rolled oats, rice, buckwheat, durum wheat pasta;
- low-fat fermented milk products;
- egg omelet or soft-boiled eggs;
- boiled, steamed, baked vegetables;
- fruits – sweet and semi-sweet apples, pears, bananas;
- desserts - puddings, casseroles, jellies, dried fruits, honey;
- drinks - pure water, non-acidic juices, jelly, compotes, fruit drinks, herbal decoctions.
No more than twice a week you can allow yesterday's bread, crispbread, crackers. Prohibited:
- fried, smoked, spicy foods and sauces;
- fast food, canned food, semi-finished products;
- fatty meats and fish, lard, offal;
- sausages;
- animal oil;
- pearl barley, millet, corn grains;
- rich soups with meat and fish broths;
- mushrooms, garlic, ginger, legumes;
- yeast baked goods, black bread;
- carbonated drinks;
- sour berries, citrus fruits.
This is a gentle and healthy diet, but its disadvantage is that some dishes may seem bland at first. However, they will bring maximum benefit, since they are easily digested, do not create a burden on the gastrointestinal tract and stimulate its normal activity.
Over time, the body physiologically fully adapts, and then the diet gradually changes towards the usual one used before cholecystectomy. The process must be controlled, the indicator will be good health and normal laboratory test results.
Diagnostics of PCES
The diagnostic range of studies should include:
- Ultrasound of the abdominal organs
- esogastroduodenoscopy with targeted examination of the nipple of Vater
- ultrasound examination with assessment of the functional state of the sphincter of Oddi (nutritional and pharmacological tests)
- endoscopic ultrasonography
- dynamic echo-choledochography
- dynamic cholescintigraphy with T 99
- hydrogen breath test
- X-ray examination.