Briefly: Sludge syndrome is a suspension in the gall bladder, which over time threatens to develop into cholelithiasis. The suspension does not manifest itself in any way at first, but it can be seen with ultrasound. Treatment is usually conservative: pills and diet.
- What is sludge syndrome?
- Reasons for the development of pathology and diagnosis of the disease
- Methods of treating the disease
- The story of how important proper nutrition is for gallbladder health
- How junk food led to poor health
- What the doctor prescribed
- What difficulties did you have with following the diet?
- How a diet violation almost led to the surgical table
- How we began to value healthy eating
This article was checked and edited by Candidate of Medical Sciences, toxicologist Stanislav Radchenko.
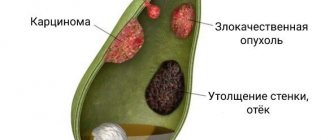
Gallstone disease is a common pathology of the gastrointestinal tract. First, a suspension forms in the gallbladder - few people know about this, even those who have already encountered this phenomenon. But it is the bile components that make up this suspension that subsequently crystallize, forming stones.
What is a suspension in the gallbladder and what does it look like?
The gallbladder is an organ whose main task is to accumulate, store and release bile in portions. It performs the function of breaking down fats during the digestion of food. Bile itself is a liquid, but with certain health conditions it thickens. Then they talk about the presence of suspension in the bubble.
When an ultrasound examination is performed, the contents of the gallbladder, that is, bile and its components, can be displayed on the screen in different ways:
- Anechoic bile is shown in black. It is clean, homogeneous, and does not contain any inclusions. This is an indicator of health.
- The bile on the screen is gray and dark gray in color, that is, echogenic. This is evidence of the heterogeneity of bile and the fact that flakes have begun to form in the gallbladder. Their density is still quite low, they are able to dissolve and easily reach the intestinal tract without blocking the ducts.
- Hyperechoic suspension, or increased echogenicity. It looks like a white precipitate on the device monitor. This formation has a greater density than just flakes. This condition is called bile sludge (biliary sludge). The clots are already dense. According to some researchers, it is from such formations that, with further progression, sand and then stones can form.
Often, in order for the specialist to see additional inclusions in the organ, the patient has to change his body position several times during the examination. This makes the flakes more noticeable.
The flocculent suspension does not pose any particular health hazard and can be removed from the gallbladder using conservative methods. But its presence significantly worsens the patient’s condition.
Suspension particles consist of various components:
- cholesterol is a component of bile;
- calcium salts;
- bile pigments formed during the work of the liver.
The suspension is usually divided according to the size of the particles that form it:
- fine suspension - particles not exceeding 5 mm in size;
- Sludge is jelly-like clots that move freely in the bile;
- sludged bile - with this condition, both sludge and finely dispersed formations are found in the bladder.
Biliary sludge: experience of therapy in real clinical practice
Biliary sludge, originally described as an ultrasound phenomenon and consisting in the visualization of accumulation of cholesterol crystals, pigment crystals and calcium salts in the biliary tract and gallbladder, has not yet been defined as a nosological entity. In accordance with the current International Classification of Diseases, 10th revision, there is no specific code that allows this condition to be encrypted in medical documentation. At the same time, most specialists and practitioners confidently speak out for the continuum of biliary sludge and cholelithiasis and suggest using the code K80.8 - other forms of cholelithiasis. The Rome Consensus VI did not clarify the role and place of biliary sludge as a nosological unit, indicating only the significant role of impaired chemistry in the composition of bile in gallbladder dyskinesia.
The prevalence of biliary sludge in the general population can reach 4%, and in patients with a symptom complex of biliary tract pathology - 55% [1–4]. With various physiological and pathophysiological abnormalities in the human body, the frequency of occurrence of biliary sludge is variable. In particular, during pregnancy, due to an increase in the level of estrogens and progestins, it is detected in 31% of women [5, 6]. With a rapid decrease in body weight, due to an increase in the level of cholesterol in the bile and a decrease in the rate of emptying of the gallbladder, biliary sludge is observed in 25% of cases [5, 7].
Biliary sludge itself, as noted above, is a suspension of liquid crystals of cholesterol monohydrate and/or calcium bilirubinate granules in a mixture of mucin and protein. The sludge suspension includes structures with different ultrasonic and physico-chemical characteristics ranging in size from 0.01 to 5 mm. It should be noted that the chemical composition of sludge varies in different clinical situations [2]. Ultrasound examination identifies the following types of biliary sludge: microlithiasis - a suspension of small hyperechoic particles, “putty-like” bile, echo-heterogeneous bile with the presence of clots of varying densities and a mixed form [11].
Risk factors for the development of biliary sludge include family history, female gender, age, geographic area of residence, foods high in fat and carbohydrates, and foods low in plant fiber. The risk of biliary sludge is significantly increased by pregnancy, obesity, diabetes mellitus, liver diseases with cholestasis syndrome, diseases of the small intestine, parenteral nutrition, and taking a number of medications [10].
The main stages of the pathogenesis of biliary sludge include the formation of vesicles with excess cholesterol content against the background of an increase in the concentration of lithogenic bile acids (BAs) and a decrease in the level of chenodeoxycholic acid. The nucleation of supersaturated bile is stimulated by an increase in the concentration of calcium, copper, manganese, iron, magnesium, potassium, etc. High importance is attached to the increase in the content of sialic acids, hexoses and the accumulation of lipid peroxidation products in the bile. A decrease in clearance due to suppression of the contractility of the gallbladder, induced by the biliary sludge itself, creates conditions for its further persistence [8].
Clinical picture of biliary sludge
The clinical picture of biliary sludge has great variability. The majority of cases of biliary sludge detection are due to incidental ultrasound findings in asymptomatic patients. Of the symptoms listed for this condition - pain, bitterness in the mouth, nausea and a number of others - only pain is a relatively specific symptom. Modern clarifications to the characteristics of pain were introduced by the Rome Consensus VI, giving a definition and criteria for “biliary pain”: episodes of persistent pain in the epigastrium and/or right hypochondrium, lasting more than 30 minutes, repeated at different intervals (not daily), interfering with daily activity or requiring treatment for emergency care, with no significant association (<20%) with bowel motility, posture, or acid suppression. Additional criteria for “biliary pain” include association with nausea and vomiting, radiation to the back or right subscapular region, and awakening from sleep [9].
A study of the natural history of biliary sludge demonstrates that up to 20% of cases end in the formation of stones in the gallbladder, while spontaneous complete regression occurs in up to 70% of cases. In 30–60% of patients with biliary sludge, dynamic ultrasound observation reveals episodes of drug-free disappearance and its re-formation [2, 5]. Possible complications of biliary sludge include acute and chronic pancreatitis, sphincter of Oddi dysfunction, acute and chronic cholecystitis, choledocholithiasis and a “disabled” gallbladder. A retrospective observation of PA Hill and RD Harris (2016) for 21 months of 104 patients with biliary sludge demonstrated the development of complications in 24% of patients [1, 12].
The proven risk of developing complications of biliary sludge in a significant proportion of patients necessitates not only clinical observation, but also drug correction of this condition. The goals of treating patients with biliary sludge should include the possible elimination of modifiable risk factors for this condition, restoration of rheological parameters of bile and impaired functions of the gallbladder/sphincter of Oddi. A drug with a convincing evidence base for its effective and safe effect on biliary sludge by influencing the main link in its pathogenesis - ursodeoxycholic acid (UDCA).
Human bile contains mainly salts of cholic, deoxycholic and chenodeoxycholic acids, while the share of UDCA does not exceed 5% of the total pool of bile acids. UDCA is synthesized in the liver from 7-ketolithocholic acid, which is a product of bacterial oxidation of chenodeoxycholic acid. An important feature of UDCA is its hydrophilicity, due to which the formation of micelles is inhibited. When taken orally, UDCA is absorbed in the jejunum by passive diffusion and in the ileum by active transport. In the liver, UDCA is conjugated, and it enters the bile with subsequent inclusion in the hepatic-intestinal circulation. When taking UDCA orally, the proportion of hydrophobic FAs decreases, and UDCA becomes the main component of bile [13].
The therapeutic properties of UDCA in relation to biliary sludge are due to a decrease in the synthesis of cholesterol in the liver and its intestinal absorption, a change in the structure and composition of micelles in bile, an increase in the dispersion of cholesterol with the formation of a liquid crystalline phase, as well as an increase in postprandial contractility of the gallbladder.
The evidence base for the use of UDCA includes a significant number of studies, including domestic authors, indicating varying effectiveness - from 60% to 87.5% and the safety of the use of UDCA drugs in the treatment of biliary sludge in different groups of patients. At the same time, there is heterogeneity in research data regarding the duration of treatment, the dose of UDCA, the dependence of application on the severity of the clinical picture and the ultrasonic form of biliary sludge [14–18]. Important and unresolved questions for clinical practice are questions about both the pharmacoeconomic aspects of biliary sludge therapy and the clinical equivalence of various UDCA drugs [19, 20].
We conducted a retrospective study to evaluate the effectiveness and safety of UDCA at a fixed dose of 10 mg/kg body weight for 12 months in patients with biliary pain and biliary sludge in real clinical practice.
The objective of the study was to determine the dynamics of biliary pain in patients with biliary sludge taking ursodeoxycholic acid; identify the effect of UDCA on the regression of biliary sludge; to study the safety of the use of ursodeoxycholic acid in patients with biliary sludge.
The study included 76 patients (52 women, 24 men) with a diagnosis of “Cholelithiasis: stage I (biliary sludge) (K80.8).” The average age of the patients was 49.4 ± 7.5 years, the average height was 164.6 ± 10.8 cm, and the average weight was 78.8 ± 8.1 kg. Patient inclusion criteria: outpatients of both sexes aged 18 to 65 years; biliary pain; biliary sludge verified by ultrasound as microlithiasis or echo-heterogeneous bile with the presence of clots of varying densities. Exclusion criteria: pregnant or breastfeeding women; gallstones; polypoid formations of the gallbladder; non-functioning gallbladder; acute cholangitis; acute cholecystitis; acute and chronic pancreatitis; chronic hepatitis; cirrhosis of the liver; renal, cardiac, respiratory failure; obstruction of the bile ducts; empyema of the gallbladder; active tuberculosis; other acute or exacerbation of chronic diseases requiring planned or emergency hospitalization; the patient has a mental illness that does not allow assessing the adequacy of the recommendations being implemented; alcoholism and drug addiction currently or in history; patients suffering from malignant neoplasms of any location; the patient's participation in other clinical trials within the last 3 months; hypersensitivity to the components of the drug at the start of therapy.
All patients underwent a clinical examination, a biochemical study of blood serum, including determination of ALT, AST, GGT, alkaline phosphatase, bilirubin, total protein, amylase; A clinical analysis of blood, urine and stool examination was performed. To assess the severity of biliary sludge, an ultrasound examination of the gallbladder was performed before treatment, after 3, 6, 9 and 12 months during therapy. Patients, in accordance with the instructions for the drug and the current legislation of the Russian Federation, were prescribed the drug by its international nonproprietary name and at a dose of 10 mg per kg of body weight per day for 12 months. Statistical processing was carried out using application programs Statistica 6.0.
Research results
During therapy, biliary pain was relieved after 3 months in 49 patients (64.4%), after 6 months in 61 (80.3%), after 9 months in 63 (82.8%), and after 12 months in 64 ( 84.2%) patients. The effectiveness of UDCA in dissolving biliary sludge was 30.2% after 3 months, 71% after 6 months, reached 80.3% after 9 months and did not change after 12 months. Side effects of UDCA were noted in 6 (7.8%) patients: diarrhea in 2.6%, skin reactions in 1.3%, transient increase in transaminases in 3.9% of observation cases.
Analysis of the obtained data on the effectiveness of therapy demonstrates a certain dependence of the effect of UDCA on the dissolution of biliary sludge on the duration of its use. Moreover, statistical significance of the increase in the effectiveness of therapy was shown when therapy was continued from 3 to 6 months (p < 0.01) and was not detected when comparing treatment results after 6 and 9 months (p = 0.19). Adverse events from the use of UDCA were rare and did not lead to discontinuation of therapy in this observation. Statistical significance of the relationship between adverse events of taking UDCA and age, gender, and choice of drug has not been established, probably due to the small number of observations.
A study of the relationship between a positive therapeutic outcome—dissolution of biliary sludge and a certain factor in the study group of patients—established higher results of treatment effectiveness in women—86%—than in men—69.6%. In patients with normal body weight, the efficiency of dissolving biliary sludge was 85%, compared to 79.3% in patients with excess body weight. The statistical significance of the effect of gender and body weight on the outcome of therapy has not been confirmed (p > 0.05).
The patient's choice of UDCA had a significant effect on the dissolution of biliary sludge (table, figure). Of the 35 patients who took the reference UDCA drug for the Russian Federation, Ursofalk®, after 3 months from the start of therapy, biliary sludge was absent in 42.9%. Of 41 patients taking other UDCA agents, efficacy at 3 months was 19.5% (OR = 3.09; 95% Cl 1.1–8.5). After 6 months of therapy, the effectiveness of taking Ursofalk® was 82.9%, and other UDCA drugs were 60.9% (OR = 3.1; 95% Cl 1.05–9.1). By the 9th and 12th months of treatment, patients taking the reference drug UDCA demonstrated relief of biliary sludge in 91.4% of cases, and when taking other UDCA drugs in 70.7% of cases (OR = 4.4; 95% Cl 1.1–12.2).
A likely explanation for the varying effectiveness of UDCA preparations may be the fact that the solubility of UDCA directly depends on the pH of the medium. At pH less than 7.8, the solubility of UDCA is significantly reduced, the formation of metabolites with taurine and glycine is inhibited, and its absorption slows down [21, 22]. Therefore, with the same dose of the active substance of the drug, differences in its release due to the different composition of the capsule and additional substances may be fundamental for effectiveness, which in turn, with pH fluctuations in different parts of the gastrointestinal tract, determines the concentration of UDCA in the bile. Thus, it has been shown that the effectiveness of therapy with UDCA drugs also depends on the pharmacokinetic properties of each specific drug, which must be taken into account when choosing therapy.
Conclusion
In conclusion, based on the results of the presented study, it is important to note the high efficiency (80.3% in the general group and 91.4% when taking the reference drug UDCA), as well as the safety (adverse events less than 7.8%) of UDCA in the treatment of biliary sludge in real clinical settings. practice. The optimal duration of therapy with determination of the end point—dissolution of biliary sludge—should be 6 months or more. Taking into account the reliability of the factors that increase the effectiveness of biliary sludge therapy in the presented study, the choice of drug, at the same dose, has a certain significance. Randomized, prospective, controlled studies are needed to confirm the data presented.
Literature
- Janowitz R., Kratzer W., Zemmier T. et al. Gallbladder sludge: spontaneous course and incidence of complications in patients without stones // Hepatology. 1994. V. 20. R. 291–294.
- Jüngst C., Kullak-Ublick G., Jüngst D. Gallstone disease: Microlithiasis and sludge // Best Pract. Res. Clin. Gastroenterol. 2006. V. 20. P. 1053–1062.
- Shaff er E. Epidemiology and risk factors for gallstone diseases: has the paradigm changed the 21st century? //Сurr. Gastroenter. Rep. 2005. No. 7 (2). R. 132–140.
- Vikhrova T.V. Biliary sludge and its clinical significance. Author's abstract. dis. ... Ph.D. M., 2003.
- Ko CW, Beresford SA, Schulte SJ Incidence, natural history, and risk factors for biliary sludge and stones during pregnancy // Hepatology. 2005. V. 41. No. 2. P. 359–365.
- Maringhini A., Ciambra M., Baccelliere P. et al. Biliary sludge and gallstones in pregnancy: incidence, risk factors, and natural history // Ann. Intern. Med. 1993. V. 119. No. 2. P. 116–120.
- Pazzi P., Gamberini S., Buldrini P., Gullini S. Biliary sludge: the sluggish gallbladder // Dig. Live Dis. 2003. V. 35 (3). P. 39–45.
- Tukhtaeva N. S., Mansurov Kh. Kh., Mansurova F. Kh. On the molecular mechanism of biliary sludge formation // Problems of GAEL. 2006. No. 1–2. pp. 40–47.
- Peter B. Cotton, Grace H. Elta, C. Ross Carter, Pankaj Jay Pasricha, Enrico S. Corazziari. Gallbladder and Sphincter of Oddi Disorders // Gastroenterology. 2016. No. 150. P. 1420–1429.
- Ilchenko A. A., Vikhrova T. V., Orlova Yu. N. et al. Biliary sludge. Modern view of the problem // Hepatology. 2003. No. 6. P. 20–25.
- Ilchenko A. A. Gallstone disease. M.: Anacharsis, 2004. 200 p.
- Hill PA, Harris RD Clinical Importance and Natural History of Biliary Sludge in Outpatients // J Ultrasound Med. 2016. No. 35 (3). P. 605–610.
- Bueverov A. O. Possibilities of clinical use of ursodeoxycholic acid // Consilium Medicum. 2005. No. 7 (6). pp. 460–463.
- Gallbladder diseases: possibilities of therapy with ursodeoxycholic acid drugs / Comp. O. A. Sablin, T. A. Ilchishina, A. A. Ledovskaya. St. Petersburg, 2013. 34 p.
- Minushkin O. N. Ursodeoxycholic acid in gastroenterology // Effective pharmacotherapy in gastroenterology. 2008. No. 2. P. 18–24.
- Lazaridis KN, Gores GJ, Lindor KD Ursodeoxycholic acid 'mechanisms of action and clinical use in hepatobiliary disorders' // J Hepatol. 2001. V. 35. P. 134–146.
- Biliary sludge: from pathogenesis to treatment / Comp. A. A. Ilchenko et al. M.: TsNIIGE, 2006. 48 p.
- Mehdiev S.N., Grinevich V.B., Kravchuk Yu.A., Bogdanov R.N. Biliary sludge: unresolved issues // Attending Physician. 2007. No. 6. pp. 24–28.
- Raikhelson K. L., Prashnova M. K. Ursodeoxycholic acid: existing recommendations and prospects for use // Doctor.Ru. 2015. No. 12 (113). pp. 50–56.
- Sarvilina I.V. Comparative clinical and economic analysis of the use of ursodeoxycholic acid drugs in patients with stage I cholelithiasis // Treating Doctor. 2015. No. 2. P. 64–68.
- Hempfling W., Dilger K., Beuers U. Systematic review: ursodeoxycholic acid — adverse effects and drug interactions // Aliment Pharmacol Ther. 2003. No. 18 (10). P. 963–972.
- Crosignani A., Setchell KD, Invernizzi P., Larghi A., Rodrigues CM, Podda M. Clinical pharmacokinetics of therapeutic bile acids // Clin Pharmacokinet. 1996. No. 30. P. 333–358.
I. B. Khlynov*, 1, Doctor of Medical Sciences R. I. Akimenko* I. A. Gurikova**, Candidate of Medical Sciences M. E. Loseva*** O. G. Marchenko***
* Federal State Budgetary Educational Institution of Higher Education USMU Ministry of Health of the Russian Federation, Ekaterinburg ** EMC "UMMC-Health", Ekaterinburg *** MO "New Hospital", Ekaterinburg
1 Contact information
Biliary sludge: experience of therapy in real clinical practice / I. B. Khlynov, R. I. Akimenko, I. A. Gurikova, M. E. Loseva, O. G. Marchenko For citation: Attending physician No. 4/2019; Page numbers in the issue: 80-83 Tags: liver, biliary tract, cholesterol, cholelithiasis.
Causes and mechanism of suspension formation
Bile suspension can form for various reasons:
- Liver diseases and problems with the biliary tract: treatment of gallstones by destroying them, dyskinesia and blockage of the biliary tract, fatty liver, problems with the pancreas, taking certain medications.
- Poor nutrition. Abuse of fats, sweets, foods with a lot of spices, and alcoholic beverages. High content of cholesterol and calcium salts in food. Non-compliance with the diet - long breaks in meals, and then overeating. A sharp change in weight in one direction or the other.
- Hereditary factor and structural features of the bladder and biliary tract (kinks). These features provoke changes in the structure of bile, since it cannot drain normally from the bladder.
- Features of the human condition - the period of waiting for a child, older age, low physical activity.
In a normal state, bile does not stagnate in the bladder, and is periodically used to digest food eaten. When free outflow is disrupted, it begins to stagnate. This is how clots and other formations form.
Sediment in a child
Medicine has described cases of gallstone disease in children, starting from the first year of life, but such cases are extremely rare. Nevertheless, biliary sludge in children is a fairly common phenomenon in our time. The literature describes observations of visualization of sediment in a child in the first months of life using ultrasonography. There can be many reasons for this “rejuvenation” of the disease:
- child malnutrition, unbalanced feeding, weight loss;
- failure of liver enzyme systems, and, as a consequence, insufficient utilization of certain groups of medications, especially in young children;
- children after surgical interventions for organ and tissue transplantation - forced systemic intake of drugs that prevent the rejection of donor tissue disrupts the exchange of bile acids;
- congenital conditions that prevent adequate flow of bile;
- maternal diseases, the need for systemic use of medications during pregnancy and breastfeeding;
- stress factors that can cause prolonged spasms of smooth muscles, incl. bile ducts, relevant for teenage children;
- other factors found in the adult population.
Making a diagnosis in childhood is not difficult, provided a carefully collected medical history and timely examination of the child.
What are the dangers of this condition?
If, after clarifying the diagnosis, a person does not follow the doctor’s recommendations, then the violation develops into serious pathologies:
- deterioration of bile outflow and complete blockage of the channels;
- the formation of bile conglomerates, accumulations of salt crystals and stones;
- getting and getting stuck of stones in the ducts;
- inflammation of the bladder and its ducts;
- pancreatitis.
Gallstone disease and cholecystitis are consequences that, in severe conditions, can be solved exclusively by surgery.
Treatment
Treatment is carried out in accordance with three schemes, depending on the complexity of the disease:
- Minor disorders that do not cause severe pain are eliminated by prescribing corrective diet No. 5. Fatty, fried, spicy foods, some types of vegetables, mushrooms, cocoa, and chocolate are excluded from the diet. The use of medications is aimed at eliminating the root cause of the disease.
- Most patients are prescribed conservative treatment. Medicines are used to thin the consistency of bile and eliminate stagnation.
- Surgery is prescribed for more serious complications, such as cholecystectomy, laparoscopy, extracorporeal lithotripsy.
What does a person feel?
The sensations directly depend on what reason leads to the formation of unwanted particles. The size of the sand grains also matters.
Here are the most common complaints that allow a specialist to determine the condition:
- a painful feeling under the lower right rib that can last from 5 minutes to several hours;
- unpleasant sensations are sharp, pulling, grasping;
- feeling of nausea, vomiting;
- violations of stool and its regularity;
- lack of appetite.
Usually, a suspension in the gallbladder in a child or an adult does not show any signs; the condition is asymptomatic and is detected by chance on an ultrasound.
However, when a person already has diseases, for example, cholecystitis, then the general condition will depend on the amount of suspension in the gall cavity. Biliary colic is likely to occur. If there is pathology of the bile ducts, pain and heaviness will occur after eating fatty foods or after prolonged fasting.
Possible complications
The development of complications of the disease is characterized by the following stages:
- oversaturation of bile with cholesterol;
- dysfunction of the mobile balance of pro- and antinucleating factors;
- factors of nucleation and precipitation of cholesterol components;
- the combination of crystals into microlites and their subsequent enlargement.
The presence of echogenic suspension can lead to complications: acute pancreatitis, bile stagnation, biliary colic, inflammatory process in the biliary tract, cholecystitis.
Diagnosis of flakes in the gallbladder
To clarify the diagnosis, a set of research methods is used:
- taking an anamnesis - the doctor finds out when the pain first appeared, where it is localized, and when the condition worsens;
- the presence of chronic and acute diseases, harmful addictions;
- external examination, palpation of the painful area;
- urine and feces analysis, biochemical and clinical blood tests;
- Ultrasound of the digestive organs is the best way to detect gallbladder sludge;
- computed tomography and magnetic resonance imaging make it possible not only to evaluate the echo suspension, but also to determine the condition of other organs, problems with which may be the cause of its occurrence (liver and pancreas);
- study of bile from the lumen of the duodenum - duodenal intubation.
How to treat
Therapy prescribed by a specialist and adherence to certain rules will help get rid of flakes in the gallbladder. It is important after the end of the acute period not to stop following a healthy balanced diet and the recommended regimen.
Diet
Since the bladder belongs to the organs of the digestive system, the main recommendations will concern nutrition. Diet No. 5 according to Pevzner will reduce the load on organs and help them recover:
- Sludge in the gallbladder is formed mainly due to stagnation of bile. Therefore, you need to eat food often - from 5 to 7 times a day, portions should be small, comfortable for digestion.
- Avoid foods that irritate the digestive tract - fatty meats, raw vegetables and fruits, salty, sweet and spicy foods.
- It is important to give up alcohol and reduce tobacco use.
- Drinking the required amount of fluid is beneficial for the gall bladder. It is recommended to drink at least 2 liters of water per day. More accurate data should be obtained from your doctor, since for some diseases this volume may change.
Medicines
The drugs will help relieve pain and relax the spasmodic muscles of the bile ducts. It is important that all medications for such conditions are prescribed strictly by a specialist. Self-medication is unacceptable. Here are the recommended medications:
- Antispasmodics (No-shpa, Drotaverine, Papaverine) to relax smooth muscles. They help especially quickly with spasms of the bile ducts. Antispasmodic drugs help get rid of suspension in the gallbladder if the cause of its appearance is tension in the smooth muscles of the ducts.
- Medicines with a choleretic effect are necessary for stagnation of bile (Ursosan, Ursohol, Allochol, Holosas, Livodexa).
- Painkillers based on non-steroidal anti-inflammatory drugs (Paracetamol, Nurofen, Nalgesin) will relieve pain and discomfort until the main drugs begin to work. This is very important, because pain with biliary colic can be very painful.
Folk remedies
On the recommendation of a doctor, a person can try treatment with folk remedies.
Pathology can be treated with herbal infusions and decoctions with choleretic and anti-inflammatory effects. But before using such drugs, consultation with your doctor is necessary.
The most commonly used are decoctions of medicinal herbs. Choose plants that relieve inflammation and have a choleretic effect:
- sagebrush;
- chamomile;
- sea buckthorn fruits;
- corn silk.
Usually brew 1 tbsp. selected herb or mixture of herbs in a glass of boiling water, leave for an hour. Strain and drink this entire volume throughout the day. The course of treatment is at least 4 weeks.
Physical exercise
Exercising is not only not prohibited, but is even recommended:
- Cardio training will help burn extra calories, speed up your metabolism, and make all your organs work harder.
- Strength loading is permissible if permitted by the attending physician. It will force the muscles to work and take as many nutrients from the blood as possible. As a result, the digestive system will work more actively.
- Daily walking (at least half an hour) will help if a person cannot engage in more active types of exercise.
Prevention of suspension formation
To prevent problems with the bladder include classic recommendations for a healthy lifestyle:
- annual examinations with a therapist and specialists;
- seeking help when feeling unwell;
- presence of adequate daily physical activity;
- maintaining a diet and avoiding unhealthy foods;
- reduction or complete abandonment of bad habits;
- adherence to sleep and wakefulness, work and rest;
- avoiding stress and unnecessary emotional experiences.
The presence of a suspension in the gallbladder is not fatal, but it signals the onset of problems that, without treatment, can turn into serious illnesses. The liver is one of the most important organs of the human body. If you suspect problems, even indirectly related to the health of the gallbladder and liver, you should strictly follow all the doctor’s requirements. Proper therapy and the efforts of the patient himself can cure the problem completely and maintain health.