Pancreatitis is caused by self-destruction of pancreatic tissue by activated enzymes. Activation of enzymes that break down proteins and fats occurs in response to inflammatory changes in tissues.
Pancreatic changes in the activity of the pancreas occur as a response to the vigorous activity of enzymes. Excessive enzyme activity develops due to a number of factors:
Pancreatic tissue
- Mechanical destruction. It consists of blocking the duct and blocking the outflow of gland juice. Develops due to adjacent diseases of the bile ducts and edema. Injuries are distinguished separately.
- Neuroendocrine disorder. General disorders of the body's hormonal function - fat metabolism, carbohydrate metabolism. Reasons: abuse of fatty foods, alcohol.
- Toxic and allergic disorders. Allergic reactions to systemic drugs, droppers.
Regardless of the factor in the development of pain, a pancreatic attack is often caused by a combination of factors and a negligent attitude towards health.
Local changes leading to pain
The ducts of the gland close, but the release of enzymes into the food taken does not stop. The active substances are released into the tissue of the gland itself. Enzymes are highly active proteins. The fat-digesting enzyme molecule is capable of breaking down 154 fat molecules. If a small part of the enzymes gets on the gland tissue, it leads to the death of cells and tissues.
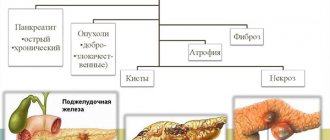
Necrosis occurs - acute pancreatitis. During necrosis, enzymes of the tissue itself are released, enhancing the effect of active substances, worsening the outflow from the affected area, increasing the vulnerability of blood vessels. The cycle of chronic pancreatitis closes.
Chronic pancreatitis
Pain syndrome in chronic pancreatitis
The key process of chronic pancreatitis is the replacement of gland tissue with connective tissue. Sometimes salt compounds, often calcium, settle in the connective tissue, clogging the ducts of the gland (calculous pancreatitis). The closed ducts continue to function, accumulating fluid, forming cysts. When an exacerbation of pancreatitis occurs, dull pain appears in the area under the stomach, increasing after a diet violation. More often, the sensations occur after heavy feasts or an excessive amount of food eaten. This happens due to the expansion of the stomach, pressing on the head of the pancreas, causing spasm, leading to pain. It occurs under the stomach, it feels deep in the abdomen. Depending on the eating disorders, the pain is short-term or becomes permanent.
The pain spreads to the area of the left sternum, affecting the shoulder, spreading to the back. If the disease progresses in the head of the gland, it spreads to the liver area. If the pathology affects the entire organ, the pain encircles.
There is an increase in pain in certain positions of the patient - lying on his back. Becomes weaker when sitting. Instinctively, the patient presses his legs to his chest in a sitting position - with this position the pain weakens.
According to statistics, with chronic pancreatitis, pain is observed in 9 out of 10 patients, and only 1 in 10 pancreatitis is not accompanied by painful sensations.
The attacks may recur. Doctors have created a scale of attacks:
- Type A. Pain lasts up to 10 days, interspersed with long periods without it.
- Type B. Long periods of pain up to 30-60 days. This type is more common in alcoholic pancreatitis.
- Persistent, ongoing pain. It is an indication for surgical intervention and the use of narcotic painkillers.
Pancreatitis, after a month of therapy there is another exacerbation, pain
Valery
6871 views
October 1, 2020
Hello! I have been undergoing treatment since August, before that I had periodic pain, but in August it got worse. The doctor diagnosed: reactive pancreatitis, chronic pancreatitis, chronic cholecystitis, chronic. gastritis of mixed type, unstable remission, not associated with nr. I was prescribed Razo 2 times a day before meals for 2 weeks, then 1 time in the morning, Duspatalin 1 time in the morning, Creon 25,000 2 times with food for 1 month, Ursosan 500 at night and Odeston 2 tablets at night. I took it for a month, there were noticeable improvements, but the treatment was continued. Razo was replaced with Controloc 1 time in the morning, Creon 25,000 with the main meal 1 time, Duspatalin 1 at night, Rebagit 1 three times a day and Phosphogliv 2 to twice a day. I took this course almost until mid-September, but on the 20th I had another attack - my tongue was coated, the pain radiated to my back. No matter what you eat, after a certain time, aching pain begins. This has already raised my nerves. In the morning you wake up and intuitively begin to look for pain in your stomach, touch it, feel it - it hurts/doesn’t hurt. As a result, sometimes you get frustrated and start to get sick. Let me add that I didn’t follow a diet as such, but switched to milk, porridge with milk, and gave up sausage, fried foods and spices. Reduced my diet. I used meat to make myself a chicken roll for breakfast. But before the new attack, I ate baked meat for breakfast for several days, ate lettuce and greens. I think that this is what created a new complication. I visited the doctor again with complaints of pain and received the following recommendations: Control 20 mg in the morning, Creon 25,000 2 times with meals, Ursosan 500 at night for 2 weeks, Odeston 2 tablets at night for 2 weeks and 5 injections of 2 ml of 0.2% platifillin . I haven’t started taking injections yet, I’m afraid. In general, it seems that the course is not very complete, maybe something should be added? I saw the doctor 2 days ago, after that I decided to fast for 24 hours - only water, liquid tea, and used phosphalugel to save myself from the aching pain - I had to drink 2 servings per day to calm the pain. The pain begins to come more in the evening towards night. After a day of fasting, I feel better. I want to start eating oatmeal with water and boiled carrots. Is it possible to consume milk and fermented milk products during this period? There is so much information that you don’t know where the truth is. I'm 50 years old, I don't drink or smoke. Working more on the computer, perhaps this provokes the disease. If possible, I would like to adjust the course of treatment. Thank you!
The question is closed
pancreatitis
relapse
pain
How long does an attack of pancreatitis last?
The answer to the question of how long an attack of pancreatitis lasts lies in the stage of pancreatitis and aspects of development. Violation of the outflow of pancreatic juice and an increase in pressure in the lumen of the duodenum lead to the reflux of contents into the gland duct. The duct is not designed for this; small breaks occur, into which active bile enzymes from the intestines enter. They activate their own pancreatic enzymes. The process of inflammation and destruction of pancreatic tissue begins.
Pain in chronic pancreatitis varies. Dull infrequent accompanies patients who violate their diet due to illness.
A different type of pain is acute, with intensification, without spasm. Women are more often haunted by pressing pain after eating. According to statistics, in women, pancreatitis is often combined with biliary tract disease. Pain after eating the wrong food goes away after 2-3 hours and occurs in periods with a chronic course.
Despite the progress achieved in the treatment of acute pancreatitis, mortality in this pathology continues to remain high. Treatment of patients with acute pancreatitis is carried out both in surgical departments (mild forms of edematous pancreatitis) and in intensive care and resuscitation departments (moderate and severe forms of destructive pancreatitis). Timely hospitalization of a patient with severe pancreatitis in the intensive care unit is extremely important, as this allows for the full range of diagnostic and therapeutic measures to be immediately provided. Treatment of such forms of pancreatitis requires large material costs, labor and time.
The pathogenesis of pancreatitis, even at present, is not fully understood, and many reasons leading to its development are known. The bulk of the causes are gallstone disease and chronic alcohol abuse (up to 75% of all causes). There are also some geographic differences in the incidence and progression of the disease. The response to various etiological factors may have a genetic predisposition, leading to different prognosis of the disease in different ethnic groups. Death at the onset of the disease is usually due to the development of systemic inflammatory response syndrome, as well as multiple organ failure. In the longer term, the leading causes of mortality are sepsis and purulent-inflammatory complications.
The clinical picture of acute pancreatitis is quite typical in many cases. There is acute pain in the upper abdomen, which often begins two to three days after drinking strong alcohol or significant dietary errors towards fatty foods, which cause significant stress on the pancreas. The onset of the disease can develop quickly, or it can drag on for several days.
Patients often complain of girdling back pain, they experience nausea, vomiting, as well as agitation and restlessness. In some cases, acute pancreatitis may begin with the development of shock or even coma.
On physical examination, the clinical manifestations of pancreatitis often depend on the severity of the disease. There is pain, tenderness on palpation of the epigastric region, signs of obstruction of the common bile duct in some cases, and effusion into the pleural cavity may be noted. If the patient seeks medical help late, as the disease progresses, a mass formation may be noted in the epigastric region due to the development of a pancreatic pseudocyst.
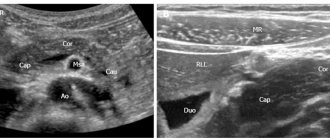
The diagnosis of acute pancreatitis is confirmed by a biochemical blood test, as well as by ultrasound and radiological examination. In a biochemical study, the level of serum amylase increases 6–12 hours after the onset of the disease; this enzyme is quickly removed from the bloodstream and is elevated for 3–5 days in pancreatitis. This test cannot be used alone to make a diagnosis, since amylase levels can increase in various pathologies. In addition, measurement of enzyme levels has low prognostic value for assessing the course of the disease and outcome. In certain severe cases, due to pancreatic necrosis, amylase levels may be within normal limits.
Radiation diagnostics, namely computed tomography, is of great importance in the diagnosis of pancreatitis. A study with oral or intravenous contrast should be performed after 48 hours; conducting a study earlier may not provide a complete picture of the nature and extent of the disease.
Treatment of a patient with pancreatitis in the intensive care unit includes a comprehensive program aimed at various parts of the etiology and pathogenesis of the disease. Treatment is carried out together with a surgeon, who must determine the need for surgical intervention and its volume, as well as resolve the issue of eliminating the cause of pancreatitis (if it is removable in a given clinical situation). Invasive monitoring is used if necessary. Adequate fluid therapy for pancreatitis is of great importance, since large volumes of fluid can accumulate in damaged pancreatic tissue and parapancreatic tissue. Inadequate infusion therapy can lead to further spread of necrosis. Pain syndrome is also eliminated, for which regional anesthesia methods can be used. To prevent infection, broad-spectrum antibacterial drugs are prescribed. The patient must be provided with adequate nutritional support.
Treatment of pain due to pancreatitis
The issue of treating pain syndrome in chronic inflammation of the gland is complex; pain and gland disorder have to be treated simultaneously.
The golden mean is observed when the functions of the gland are restored. Favorable conditions are created for the organ through a strict diet and pain relief. After the pain disappears, the inflammatory process in the gland is relieved and treatment is carried out to restore function.
It is necessary to occupy the gland by restoring the outflow of pancreatic juice, then the pain will subside. For these purposes, non-narcotic analgesics and antispasmodics are used in a hospital setting. Good results are observed when using drugs that block choline receptors, using ganglion blockers.
For persistent pain of an increasing nature, analgesics are administered intravenously - novocaine, diphenhydramine, papaverine, combined with saline, magnesium sulfate and ascorbic acid.
In some cases, doctors resort to the use of serious analgesics - tramadol and others. Sometimes the described therapy is replaced by paracetamol with non-steroidal anti-inflammatory drugs. In extreme cases, narcotic analgesics allow the patient to survive until surgery.
Depending on the stage, the pain can last a long time without subsiding. For such pancreatitis, surgical treatment is recommended. An operation is performed to remove part of the gland or duct.
Home remedies to relieve pain
Selected measures can temporarily lull the pain and relieve the symptoms of acute pancreatitis. Conventionally, the measures are called “Cold, hunger and peace”:
- Refusal of food. The minimum time is one day. The measure is due to the need for enzymatic unloading of the gland.
- Apply a cold compress or a bottle of cold water to the navel area to eliminate swelling.
- Water mode. Increasing the liquid to 2 or more liters of warm water.
- Elimination of spasm. Taking antispasmodics.
- Peace from stress. Avoid physical and psychological stress.
The following simple actions ease and relieve pain. It is important to remember that moderation in consuming foods not recommended for pancreatitis will only provoke pain. You should take medications to relieve pain after a specific doctor’s prescription.