Any abscess is a cavity filled with pus. A liver abscess also fits this classic definition. The peculiarity of the disease lies in the source of inflammation. The doctor faces questions: where did the infection come from in the sterile liver? How did it come into being? Having found the answers, you can choose the right treatment and achieve a favorable outcome of the disease.
The disease is more common among young and middle-aged men. The disease is registered in men 7 times more often than in women. According to statistics, non-parasitic abscesses account for 4.9–5.1 per 10 thousand hospitalized patients. In the general surgical department of a multidisciplinary hospital, the proportion of patients with this disease reaches 0.5%.
Causes
The causes of liver abscess in every tenth case remain unknown. The greatest interest is shown in primary abscess formation. This includes the occurrence of a lesion directly in the liver tissue against the background of previously unchanged structures of the organ.
Secondary liver abscesses imply a route of infection. Most often, infection occurs through:
- bile ducts (30–40% of all abscesses) - with inflammation (cholangitis), cholelithiasis, malignant neoplasm, they are called cholangiogenic abscesses;
- blood (up to 20%) - from the vessels of the abdominal cavity through the portal vein and hepatic artery (appendicitis, peritonitis, diverticulitis, peptic ulcer of the large intestine, enterocolitis, sepsis);
- tissues by contact - when empyema breaks through into the liver from the gallbladder, subdiaphragmatic abscess, penetration of a stomach ulcer;
- destruction due to trauma, surgical intervention on the liver, a purulent focus in the liver can develop not only with direct injury to the parenchyma of the organ, but also as a result of closed injuries received in road accidents, falls, beatings due to suppuration of hematomas, usually occurs after 3–4 weeks after injury.
When an infection enters the blood vessels, an abscess develops within 10 days
Liver abscess after surgery accounts for up to 30% of all cases. Abscesses with an unknown cause are called cryptogenic. Various authors indicate their share in the population from 10 to 20%.
An abscess also occurs:
- with the disintegration of a tumor and specific granulomas (tuberculosis) in the liver;
- infection of various cysts (parasitic and others).
The main causative agents of inflammation are:
- hemolytic streptococcus;
- enterobacteria;
- Staphylococcus aureus;
- coli;
- Klebsiella;
- protozoa (amoebas).
Less commonly - Proteus and Pseudomonas aeruginosa. Mixed infection is very common. Abscess formation in the liver can cause infection:
- worms (usually roundworms);
- alveococcus;
- Echinococcus.
For amoebic and parasitic origin, it is typical to enter the body through the mouth, penetrate into the wall of the small intestine, transport into the liver parenchyma and form within three months a cyst-focus filled with infectious agents and necrotic masses. Gradual growth leads to rupture.
The main risk factor for liver abscess is a sharp drop in immunity. This condition leads to the development of a purulent focus in the liver, as a complication of other diseases. This course of the disease is observed in 3–5% of cases.
Symptoms
The person does not feel anything, despite the fact that a large formation is forming in his liver. Only when the cyst becomes very large can dull pain appear in the right hypochondrium.
Complications may develop that are associated either with an allergic reaction to the waste products of the helminth, or with compression of nearby organs by a large cyst. Main complications:
- allergy symptoms - mainly hives or diarrhea;
- intestinal obstruction if it is compressed by a cyst;
- portal hypertension syndrome in case of pressure on the portal vein or its main branches;
- obstructive jaundice - caused by a violation of the outflow of bile into the small intestine.
Suppuration of the cyst and the formation of an abscess in the liver is one of the likely complications of echinococcosis.
Frequency of distribution of different forms
Statistical records and studies of the etiology of liver abscesses revealed the following prevalence among patients:
- amoebic - 64.7% of patients;
- Echinococcal - 12.5%;
- bacterial - 6.5% (including the consequences of dysentery, phlegmonous appendicitis, putrefactive colitis, cholecystitis);
- cholangiogenic - 5.2%;
- traumatic - 1.8%;
- Giardiasis - 0.4%.
According to other data, the proportion of liver abscesses of appendicular etiology is up to 32%, and cholangiogenic - 39%. Rare cases of primary tuberculous liver abscess have been identified; only about 100 such cases have been described.
General information
A liver abscess is a limited purulent accumulation in the liver parenchyma as a result of the penetration of a parasitic or bacterial infection, which causes purulent-destructive processes. The pathology was assigned the ICD-10 code: K75.0. A type is suppuration of hydatid cyst ; hepatic amoebic abscess (ICD-10 Code: K77.0).
The main predisposing factors are the presence of foci (for example, appendicitis , cholecystitis ) and hematogenous, cholangiogenic or lymphogenous penetration of infection from them. There is also a high probability of infection in cases of liver damage and surgical operations on internal organs.
Classification
In addition to the primary and secondary types already given, as well as classification according to routes of infection, abscesses are distinguished according to etiology:
- parasitic;
- bacterial - more common in women 30–60 years old.
Parasitic infection is recorded 4 times less frequently than bacterial infection.
By number:
- single - 87.5% of patients;
- multiple - 12.5%.
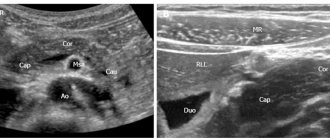
On ultrasound, multiple abscesses are visible as round formations
By size:
- large;
- small.
By localization:
- right lobe (80.2%),
- left (14.7%);
- in both (5.1%).
Depending on the accompanying complicating factor:
- complicated;
- uncomplicated.
Secondary processes are considered complicated against the background of:
- pleurisy;
- liver failure.
In these cases, the course of the disease is threatened by abscess rupture and general sepsis. According to the international classification, all types of liver abscesses are coded K 75.0, except amoebic, which is included in the class of infectious diseases with code A 06.4.
Pathogenesis
Suppuration in the liver is usually limited and has a sheath of connective tissue that separates it from healthy parenchyma. Lytic melting of tissue occurs inside the lesion.
Schematic representation of a liver abscess
Liver abscess - varies depending on the route of infection:
- Biliary tract - the infection penetrates the bile ducts and is usually caused by obstructive jaundice and cholangitis (in 30-40% of cases).
- Venous route - passes through the portal vein and is characteristic of destructive appendicitis, cholecystitis, nonspecific ulcerative colitis (approximately 20% of cases).
- Arterial - the passage of infection through the liver artery causes various diseases, which are accompanied by bacteremia and sepsis .
- Contact - provoked by a breakthrough of liver tissue and empyema of the gallbladder , observed in cases of penetrating gastric ulcers and subdiaphragmatic abscess .
- Traumatic - caused by closed and open liver injuries.
- Cryptogenic - liver abscess is diagnosed in approximately 20% of NOS - without additional instructions, that is, when the cause of development could not be determined.
Pathological and anatomical signs
The source of infection is surrounded by dilated veins and a bank of inflamed edematous parenchyma cells. A cavity forms in the center. First, the abscess is delimited from the surrounding tissues by a grayish-red membrane. Then it becomes thicker and forms a dense capsule. Cholangiogenic abscesses are located along the branches of the bile ducts. At the same time, inflammation forms in the walls, and bile stagnation occurs in the lumen of the ducts.
If the abscess comes directly from the gallbladder, then more often it has a single character and is located close to the bladder bed. The longer the disease, the greater the chance of infection penetrating into the liver tissue and the formation of thick-walled multi-chamber structures.
Conservative treatment
It is necessary to treat patients with suspected liver abscess only in a surgical hospital. The treatment plan is developed individually for each patient. If small single or multiple lesions are detected, then conservative measures are used. Among antibiotics, preference is given to drugs with a wide spectrum of effects:
- third generation cephalosporins;
- aminoglycosides;
- macrolides.
The drug is administered intravenously
A parasitic abscess requires the mandatory prescription of specific antiparasitic agents:
- for amoebic etiology - Yatren, Emetin, Diiodoquine, Hingamin, Chloroquine, Metronidazole, Tinidazole, Ornidazole are used according to indications;
- if alveococcosis is detected - Albendazole, Mebendazole;
- for echinococcosis - a group of benzolimidazoles.
If it is possible to drain the liver abscess after the procedure, a tube is installed through which antibiotics are injected directly into the cavity for several days and rinsed with an antiseptic solution.
Conservative treatment must be accompanied by:
- prescribing vitamins to improve immunity and support liver function;
- means that relieve intoxication (Hemodez, Ringer's solution, glucose);
- cardiac drugs and diuretics for ascites;
- hemostatic therapy for bleeding tendencies;
- prescription of antipyretics;
- sufficient pain relief;
- a course of enterosorbents to remove waste and toxins through the intestines (Smecta, Enterosgel);
- if necessary, use antiemetics.
It is imperative to treat the underlying disease that contributes to the formation of an abscess (sepsis, osteomyelitis, cholecystitis, peptic ulcer, tumors).
Symptoms of liver abscess
The initial clinical manifestations of liver abscess are not very specific. A person feels for several days:
- general malaise;
- chilling;
- slight increase in temperature;
- dizziness;
- drowsiness, weakness;
- aching joints;
- nausea.
Attacks of nausea are one of the signs of a pathological condition
Patients usually associate symptoms with a cold. The duration of this period is determined by the state of the body’s defenses: the higher the immunity, the more actively and longer the person resists infection.
The further course of the disease is expressed:
- in a significant increase in temperature (up to 39–40 degrees);
- constant chills with profuse sticky cold sweat on the body;
- lethargy;
- headache;
- tachycardia;
- nausea and vomiting;
- hallucinations;
- memory loss.
Signs of liver damage include:
- intense pain in the hypochondrium on the right with precise localization - it is dull, aching, constant, radiating to the right shoulder and scapula, patients note an increase in the position of lying on the left side, with movements, deep breathing and a decrease if curled up on the right side;
- feeling of heaviness;
- severe pain when pressing on the lower ribs and hypochondrium on the right;
- the appearance of ascites (a large abdomen due to the accumulation of fluid in the abdominal cavity) - associated with compression of the liver vessels, thrombosis;
- palpable enlargement of the liver and spleen, the edge is painful to the touch;
- weight loss - complicates diagnosis in terms of suspicion of a malignant tumor;
- dark urine and discolored stool;
- the presence of bloody discharge in the stool;
- signs of esophageal or intestinal bleeding (vomiting brown contents, called “coffee grounds”, liquid black stool);
- bloating;
- diarrhea;
- exacerbation of chronic hemorrhoids;
- lack of appetite.
Yellowness of the skin, sclera, and mucous membranes occurs in the later stages of the disease
A feature of the course of secondary liver abscesses is the long-term predominance of clinical symptoms of the underlying disease. This complicates and increases the diagnostic time.
Some authors distinguish three types during the course of the disease:
- I - all classic symptoms appear;
- II - signs of an abscess are “masked” by the clinic of diseases of the digestive system;
- III - manifestations develop gradually in the absence of clear symptoms, most likely in immunodeficiency states.
Possibilities of ultrasound diagnosis of liver abscess (clinical observation)
Ultrasound scanner HS50
Affordable efficiency.
A versatile ultrasound scanner with compact design and innovative capabilities.
Introduction
Liver abscess is a limited purulent-destructive suppuration of its parenchyma with a focus of lytic melting in the center, resulting from the introduction of infection by hematogenous, lymphogenous, cholangiogenic or contact routes, as well as infection of intraparenchymal and subcapsular hematomas. Liver abscess was first described by Hippocrates 400 BC. He suggested that the severity of the disease may depend on the nature of the abscess contents. At the beginning of the 19th century, R. Bright first suggested the possibility of the formation of liver abscesses in amebiasis, and in 1890, W. Osler was the first to discover amoebae in the liver abscess and feces of the same patient. P. Dieulafoy and H. Fitz considered suppurative diseases of the abdominal organs among the various causes of the formation of liver abscesses [1]. In 1926, pylephlebitic liver abscess was first described in a patient with diverticulitis. In 1903, L. Rogers noted the connection between purulent cholangitis, bile duct obstruction and liver abscesses. Before the advent of antibacterial drugs in the 30s of the last century, late diagnosed destructive appendicitis was the main cause of the development of pylephlebitic liver abscesses. In 1938, A. Ochsner and M. DeBakey, having analyzed surgical protocols and autopsy material, found that in 35% of cases the cause of the formation of liver abscesses was appendicitis [1].
Typically, a liver abscess is a secondary disease that develops against the background of existing inflammatory changes in the liver. But there are abscesses that are a manifestation of a primary disease (parasitic etiology). There are several classifications of liver abscesses; there is no single classification. The most comprehensive, in our opinion, is the classification of liver abscesses by B.I. Alperovich [2].
- Primary liver abscesses: bacterial (coccal, bacillary, mixed);
- parasitic (amoeba, roundworm, echinococcal, opisthorchiasis, giardiasis, etc.).
- suppuration of pathological neoplasms of the liver (non-parasitic liver cyst, decaying cancer, syphilitic or tuberculous granuloma);
- single;
The epidemiology of liver abscesses is not well understood. In different countries, incidence rates can vary greatly, ranging from 2.3 per 100 thousand population in North America to 275.4 per 100 thousand in Taiwan [3]. Before the era of antibacterial therapy, the main cause of liver abscesses was acute appendicitis. Mortality was extremely high and amounted to about 80%. With the introduction of antibiotics and surgical treatment methods into clinical practice, this figure decreased significantly, remaining, however, at the level of 10-40%. At the same time, the structure of etiological factors of liver abscesses has also changed. Diseases of the biliary tract and liver, malignant neoplasms and complications of invasive medical procedures began to come to the fore [4, 5].
The etiology of liver abscesses is heterogeneous. The main causes include infectious and inflammatory diseases, malignant neoplasms, iatrogenic conditions and blunt liver injuries (see table). In developed countries, abscesses of bacterial etiology predominate, while in Southeast Asia and Africa amoebiasis remains their most common cause [3].
Table
. The main causes of the development of liver abscesses [1].
| Hematogenous abscesses (portal and arterial) | Cholangiogenic abscesses | Abscesses in liver diseases | Iatrogenic causes and injuries |
| Sepsis | Cholangitis as a consequence of choledocholithiasis, strictures, neoplasms of the biliary tract, chronic opisthorchiasis | Primary malignant tumors of the liver (adenocarcinoma, etc.) and metastatic liver disease | Percutaneous ethanol injections Chemoembolization of the hepatic artery Radiofrequency ablation of liver tumors |
| Inflammatory diseases of the abdominal organs leading to pylephlebitis: - appendicitis; - acute cholecystitis; - pancreatitis; - diverticulitis; - Crohn's disease; - ulcerative colitis; - peritonitis | Biliodegestive anastomoses, fistulas | Liver granulomas | Surgical interventions and endoscopic procedures on the biliary tract and liver: - stenting; — papillosphinc-terotomy; — choledochoduodenostomy; - liver resection; – orthotopic liver transplantation |
| Violation of the integrity of the intestinal wall with the subsequent development of bacteremia: - endoscopic polypectomy; - non-metastatic colon cancer | Acute cholecystitis (hematogenous or direct spread of infection) | Liver hematomas | Blunt liver injuries |
| Amoebiasis |
The main risk factors for the development of liver abscesses are diabetes mellitus, liver cirrhosis, immunodeficiency states, old age, and male gender [4].
Despite significant advances in medicine, early and accurate diagnosis of liver abscesses remains critical. Difficulties in interpreting the clinical picture, the results of laboratory and instrumental research methods can cause late diagnosis, untimely initiation of treatment, the development of severe complications and, as a consequence, an unfavorable outcome of the disease. Thus, according to T. Pang et al., the diagnosis of liver abscess could be established on average a week after the appearance of its first symptoms [6].
The clinical manifestations of liver abscesses are nonspecific and may depend on their size, number and location. Most patients complain of pain in the right hypochondrium, fever and other symptoms of intoxication (chills, myalgia, weakness, sweating, tachycardia, nausea, anorexia). The pain often intensifies with a deep breath, changing body position, and can radiate to the right shoulder, scapula, and upper arm. An objective examination may reveal hepatomegaly. Sometimes jaundice and ascites occur. The clinical picture of the disease that led to the development of an abscess often comes to the fore [2, 5-8].
Laboratory indicators are not very specific and reflect the presence of an active inflammatory process. A general blood test reveals leukocytosis and accelerated ESR. Biochemical examination showed increased levels of C-reactive protein, bilirubin, ALT, and AST [1, 4].
The main methods for diagnosing liver abscesses are ultrasound and CT of the abdominal cavity. The sensitivity of these methods is 96-100%. At the same time, according to A. Lin et al., when contacting 25% of patients, ultrasound results give indeterminate results, and in 14% they are false negative [9].
To determine the etiology of liver abscesses, bacteriological examination of the contents of the abscess and blood is of great importance.
The ultrasound picture of a liver abscess has a number of features associated with the time of its existence. In the formation phase, in the presence of appropriate clinical and laboratory data in the liver parenchyma, it is possible to identify a zone of reduced echogenicity with a heterogeneous structure and unclear contours that transform into normal tissue. In the central part of this zone of reduced echogenicity (zone of intense parenchymal edema), an anechoic structureless area is usually detected, which is an area of tissue necrosis, so far without a liquid component. This picture can be observed for a short period of time (several hours). Subsequently, with a parallel increase in clinical manifestations, a fluid-containing anechoic cavity with internal echogenic contents is formed, due to the presence of pus and tissue detritus. In addition to the echographic signs characteristic of the liquid structure (the effect of enhancing the posterior wall, the effect of lateral shadows, the effect of distal pseudo-amplification of the echo signal), some special signs are observed: separation of the contents of the abscess cavity with the formation of a “liquid-liquid” boundary with a horizontal level, where the thicker part is located below ; possible appearance of air bubbles in the cavity (in the presence of gas-producing flora, for example the genus Klebsiella) in the form of hyperechoic structures near the upper wall, giving the “comet tail” reverberation effect; movement of all internal contents when the patient’s body position changes; the formation of a clear demarcation of the abscess cavity from the surrounding liver parenchyma in the form of a somewhat heterogeneous rim (pyogenic membrane) of increased echogenicity with a thickness of 0.5-1.5 cm [10].
In the literature, we came across a description of the ultrasound picture of a liver abscess depending on the predominance of infiltrative or destructive changes [11]. The authors identified two types of abscess images. Type I abscesses are located, as a rule, in the posterior segments of the right lobe (VI, VII) and represent areas of parenchyma of increased echogenicity of various sizes with unclear contours of a heterogeneous structure with the presence of foci of reduced echogenicity or fluid formations of irregular shape, corresponding to areas of necrosis. Such abscesses are a consequence of inflammatory infiltration of the parenchyma during exacerbations of opisthorchiasis cholangitis. As experience has shown, given the predominantly infiltrative nature of the lesion and a minor destructive component, these abscesses, with timely detection and adequate antibacterial therapy (preferably with intraportal administration), can be cured without surgery.
Type II abscesses are a consequence of purulent cholangitis and are unevenly dilated intrahepatic bile ducts with thickened and compacted walls, with the presence of heterogeneous echogenic content (pus, detritus) in the lumen. These abscesses are characterized by multiple localization, small size, connection with the bile ducts, the walls of which are the walls of the abscesses. Type II abscesses develop from cholangioectasis with prolonged biliary hypertension caused by obstruction of the ducts as a result of sclerotic changes, stenosis of the major duodenal papilla, and obstruction by opisthorchiasis detritus.
The echographic picture of a parasitic abscess in amoebiasis may have some differences [10]. When amoebas enter, inflammatory infiltration develops, followed by the formation of foci of necrosis and lysis of the liver tissue. Ultrasound initially shows moderate and then pronounced diffuse-focal heterogeneity of the liver parenchyma with mixed and predominantly reduced echogenicity. Then, against this background, hypoechoic areas of irregular shape of various sizes with uneven, unclear contours are formed. Subsequently, they form one or several cavities, almost similar in ultrasound signs to bacterial abscesses, but with a number of differences: the contours are usually uneven with the presence of “pockets”, the echogenic membrane around the abscesses is not clearly expressed, heterogeneous contents are visualized in the abscess cavity, up to the presence of sequestration of the liver tissue and a large amount of gases.
When abscesses break into the abdominal and sometimes pleural cavity, into the retroperitoneal space, accumulations of fluid similar to the contents of the abscess are detected extrahepatically, and a defect in the liver capsule may be visible.
The main treatment method for liver abscesses is their surgical or percutaneous drainage in combination with parenteral administration of antibiotics [12-14]. First-line therapy is usually a combination of a third-generation cephalosporin with metronidazole. For small abscesses (less than 3 cm), only systemic antibiotic therapy can be used. For amoebic abscesses, the drugs of choice are metronidazole and tinidazole [1, 2, 4].
The key to successful management of patients with liver abscesses is often timely diagnosis and treatment of the underlying disease.
To illustrate the above brief overview, we present a clinical observation.
Clinical observation
Patient A., born in 1971, instructor in therapeutic exercises. He complained of chills, fever, weakness, lack of appetite, and slight vague discomfort in the right hypochondrium.
I fell ill a week before going to the clinic, when, for no apparent reason, an acute “shooting” pain arose in the shoulder girdle and under the shoulder blade on the right, which intensified with breathing. The patient assessed the pain as “muscular.” Conducted a session of therapeutic exercises. The pain subsided. The next day, an aching and stabbing pain appeared in the right hypochondrium, radiating under the right shoulder blade, intensifying with breathing and movement. Body temperature increased to 37.8 °C.
On the 3rd day after the appearance of the first symptoms, the patient went to the clinic at his place of residence. Ultrasound of the abdominal organs revealed signs of moderate hepatomegaly, predominantly in the right lobe of the liver, and a general blood test revealed leukocytosis up to 14.6 x 109 /l and acceleration of ESR up to 59 mm/h.
Over the next 4 days, there was no abdominal pain, but weakness, anorexia increased, and fever and chills were often bothersome. Low-grade fever persisted. I took paracetamol. I contacted our clinic.
From the life history it is known that the patient leads a healthy lifestyle and has no bad habits. Three months ago I went to Japan, and about three years ago I visited India. During the trips and after them I did not get sick.
At the time of treatment, the condition is of moderate severity. Body temperature 38.4 °C. The skin is pale pink. Subcutaneous fat is moderately developed. There is no swelling. Peripheral lymph nodes are not palpable. In the lungs, breathing is vesicular, weakened on the right in the lower parts, there is no wheezing. Heart sounds are rhythmic and clear. Blood pressure 120/75 mm Hg. Pulse 102 beats/min.
The abdomen is not enlarged, participates in the act of breathing, and is soft and painless on superficial palpation. The lower edge of the liver is percussion at the edge of the costal arch. On palpation, the liver has a soft-elastic consistency and is painless. Ortner's and Murphy's signs are negative. However, with deep palpation in the right hypochondrium, a stabbing pain occurred in the right shoulder girdle. Frenicus symptom is negative on both sides.
Stool once a day, formed, brown, without pathological impurities. Urination is free and painless.
To clarify the diagnosis, the patient underwent an ultrasound of the hepatobiliary zone with ultrasound angiography:
The liver is enlarged in size: the anteroposterior size of the right lobe is 14.3 cm (N up to 12.5 cm), the vertical size of the right lobe is 19.0 cm (N up to 15.0 cm), the anteroposterior size of the left lobe is 9.3 cm (N up to 7.0 cm). The diaphragmatic edge is smooth. The structure of the liver parenchyma is heterogeneous with the presence in the right lobe in the projection of the V segment of a formation of reduced echogenicity, with somewhat indistinct contours, dimensions up to 6.5 x 4.6 x 4.8 cm, a clearly heterogeneous structure with the presence in the central sections of an area of moderately increased heterogeneous echogenicity structure measuring 5.8 x 4.8 x 4.2 cm, avascular (Fig. 1). Along the periphery of the formation there is deformation of the vascular pattern (Fig. 2). The echogenicity of the liver is normal. Intra- and extrahepatic bile ducts are not dilated, their walls are compacted. The diameter of the portal vein is 1.2 cm.
Rice. 1.
B-mode. In the right lobe of the liver, in the projection of the V segment, a formation of reduced echogenicity with unclear contours of a clearly heterogeneous structure is visualized with the presence in the central parts of an area of moderately increased echogenicity of a heterogeneous structure.
CDK): the described formation is avascular, along its periphery there is a deformation of the vascular pattern"/>
Rice. 2.
Color flow mode. The described formation is avascular. Along its periphery there is a deformation of the vascular pattern.
The gallbladder is typically located, measuring 7.0 x 1.7 cm, with an inflection closer to the neck. The contours are clear and even. The wall is 0.3-0.4 cm thick, the echogenicity is moderately increased. The contents of the bubble are homogeneous. The common bile duct is not clearly visible, the diameter of the proximal part is 0.5 cm.
Pancreas: veiling of the pancreas is satisfactory, not enlarged in size: head 2.5 cm, body 0.9 cm, tail is not clearly visualized - 2.7 cm. The contours of the head and body are smooth and clear; the contours of the tail are somewhat indistinct. The structure of the parenchyma is somewhat heterogeneous. Echogenicity is moderately increased. The Wirsung duct is not visualized.
The spleen is not enlarged in size - 11.6 x 4.4 cm, area 47.66 cm² (N up to 50.0 cm²). The contours are smooth and clear. The structure of the parenchyma is diffusely heterogeneous. The echogenicity is average. The splenic vein is up to 0.6 cm in diameter. The retroperitoneal and para-aortic lymph nodes are not clearly visualized. No free fluid was detected in the abdominal cavity. Conclusion: suspicion of an abscess of the right lobe of the liver. Hepatomegaly. Moderate diffuse changes in the spleen.
Taking into account the data obtained, a preliminary diagnosis was established: “liver abscess.” The patient was urgently hospitalized at the Research Institute of Emergency Medicine named after. N.V. Sklifosovsky. In the hospital, a CT scan of the abdominal organs confirmed the diagnosis.
Percutaneous drainage of the abscess was performed. When inoculating the abscess contents, no growth of pathogenic flora was obtained.
Antibacterial therapy and washing of the abscess cavity with antiseptics were carried out. The symptoms of intoxication were completely stopped, the size of the abscess cavity was significantly reduced. The patient was discharged in satisfactory condition under the supervision of a polyclinic surgeon.
Conclusion
The presented clinical observation illustrates a case of acute cryptogenic liver abscess with a developing capsule in a young man who does not have significant risk factors for the development of this pathology. In the clinical picture, attention is drawn to the atypical onset of the disease, manifested by pain in the chest, and the spontaneous disappearance of pain with increasing symptoms of intoxication.
Difficulties in interpreting the clinical picture in this patient were also associated with the absence of significant pathology of the liver and gallbladder according to a previously performed ultrasound. However, the characteristics of the pain syndrome, the presence of intoxication, and objective examination data suggested an acute inflammatory disease of the liver or gall bladder. Repeated ultrasound allowed us to quickly and accurately establish the diagnosis on an outpatient basis, which ensured timely initiation of treatment and a favorable clinical prognosis.
Literature
- Akhaladze G.G., Tsereteli I.Yu. Liver abscesses // Annals of surgical hepatology. 2006; 11 (1): 97-105.
- Alperovich B.I. Liver surgery. M., 2010: 245-260.
- McKaigney S. Hepatic abscess: case report and review // West J Emerg Med. 2013; XIV (2): 154-158.
- Lebedev M.S. Experimental substantiation of minimally invasive combined surgical treatment of liver abscesses (experimental study): Diss. ...cand. honey. Sci. Saratov, 2015. 173 p.
- Roesch Dietlen F., Perez Morales A., Diaz Blanco F. Laparascopic surgical treatment of non-parasitic hepatic cyst // Rev Gastroenterol Mech. 1999; 64 (2): 56-60.
- Pang T.C., Fung T., Samra J. et al. Pyogenic liver abscess: An audit of 10 years' experience // Wld J Gastroenterol. 2011; 17: 1622-1630.
- Mavilia MG, Molina M., Wu GY The Evolving nature of hepatic abscess: a review // J Clin Transl Hepatol. 2016; 4 (2): 158-168.
- Lardiere-Degueltea S., Ragot E., Amrouna K. et al. Hepatic abscess: diagnosis and management // J Visc Surg. 2015; 152 (4): 231-243.
- Lin AC, Yeh DY, Hsu YH et al. Diagnosis of pyogenic liver abscess by abdominal ultrasonography in the emergency department // Emerg Med J. 2009; 26: 273-275.
- Practical guide to ultrasound diagnostics. General ultrasound diagnostics; Ed. Mitkova V.V. M.: Publishing house "Vidar-M", 2003: 106-108.
- Tskhai V.F., Brazhnikova N.A., Merzlikin N.V., Maksimov M.A., Saipov M.B., Eskov I.M., Khlebnikova Yu.A. Opisthorchiasis liver abscesses // Bulletin of Siberian Medicine. 2011; 3: 129-135.
- Chen C.-H., Wu S.-S., Chang H.-C. Initial presentations and final outcomes of primary pyogenic liver abscess: a cross-sectional study // BMC Gastroenterol. 2014; 14:133.
- Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 9th ed. Elsevier, 2010.
- Boyko V.V., Tishchenko A.M., Maloshtan A.A., Skory D.I., Smachilo PM Treatment of solitary liver abscesses taking into account the stage of abscess formation // Xipyrgy of Ukraine. 2013; 1: 16-21.
Ultrasound scanner HS50
Affordable efficiency.
A versatile ultrasound scanner with compact design and innovative capabilities.
Diagnostics
To make a correct diagnosis, the doctor needs to find the main source of infection and find out how the liver is infected. When questioning the patient, attention is paid to:
- duration of symptoms;
- previously suffered septic diseases (endocarditis, osteomyelitis, furunculosis), inflammatory diseases of the digestive system (enterocolitis, amoebic dysentery);
- living in areas with endemic prevalence of echinococcus, alveococcus, and amoebiasis;
- professional and domestic contact with animals, cutting of carcasses, processing of hides and skins;
- clarification of alcohol history to exclude chronic alcoholic hepatitis and liver cirrhosis.
Percussion reveals enlarged liver boundaries and flatulence due to intestinal bloating. Palpation reveals a painful soft edge of the enlarged liver; the spleen can be identified in the left hypochondrium.
Prevention
Prevention of liver abscess is simple - treatment of abdominal diseases should be timely and correct, under the supervision of a doctor. It is necessary to pay attention to the problem of cholecystitis, cholelithiasis (cholelithiasis), and appendicitis. Complications of liver abscess can be different. It can eventually break through, after which acute peritonitis develops - inflammation of the peritoneum, the membrane covering it and all the organs located in it. A breakthrough can occur, for example, in the intestines or stomach. Multiple abscesses are much more difficult to cure, especially if the diagnosis is delayed and treatment is not carried out on time. Such an incident could be fatal. A separate item is amoebic liver abscess, the most common form of extraintestinal amebiasis. As mentioned above, it is caused by dysentery amoeba entering the organ from the intestines.
Prevention measures should always be focused on breaking the chain of transmission of infection, and in simple words - hygiene, disinfection, as well as identifying infections in people at risk and their timely treatment. Those at risk:
- patients with diseases of the gastrointestinal tract, especially infectious ones;
- residents of settlements where central sewerage is not installed;
- personnel of food enterprises, similar organizations and grocery stores; workers of greenhouses;
- servicing treatment and sewerage systems;
- persons who were in areas with a high incidence of amoebiasis among local residents.
Workers and those who work for food enterprises and organizations that are equivalent to them (kindergartens, schools, sanatoriums) must be examined for eggworms and intestinal protozoa.
If the test for the presence of parasites is positive, treatment is prescribed. Scheduled preventive examinations are carried out 1-2 times a year. Medical examination of those who have recovered from the disease lasts 12 months. Hygiene consists of protecting the environment from pollution through sewers and providing the population with a supply of suitable drinking water. Also, in hospitals and clinics, the secretions of a patient with an infectious liver abscess must be immediately disinfected. It is important to maintain hand hygiene.
Laboratory research
The results of laboratory tests indicate a pronounced inflammatory reaction and intoxication of the body:
- leukocytosis with a shift of the formula to the left;
- the appearance of reticulocytes in the blood;
- increase in ESR;
- drop in red blood cells and hemoglobin.
Damage to the liver tissue is indicated by elevated tests for bilirubin, alanine and aspartic transaminases, and alkaline phosphatase.
An increase in the pigment bilirubin is detected in the urine. Stool analysis reveals a lot of undigested food debris and blood.
Radiological signs of liver abscess are:
- areas of tissue clearing or one large formation with a fluid level;
- limited mobility of the right dome of the diaphragm;
- reactive pleurisy (fluid in the pleural cavity on the right).
Ultrasound examination (US) is the most convenient for diagnostic purposes. It is performed on patients for emergency indications and allows to identify:
- increased size of the liver and its individual sections;
- the presence of small and large cavities filled with fluid and pus;
- diameter and localization of ulcers.
The abscess has the appearance of a hypoechoic formation with rounded, even contours. Under ultrasound control, in the surgical department, material is taken from the suspected abscess with a thin needle for biopsy and bacteriological examination.
If possible, therapeutic drainage with evacuation of contents is carried out
Subsequent tank. the analysis allows you to accurately determine the pathological flora and its sensitivity to antibiotics. Experts consider it mandatory to study the histology of the abscess capsule. The diagnosis of tuberculous abscess and detection of tumor disintegration depend on the result.
If clarification is necessary and during preparation for surgery, magnetic resonance and computed tomography are performed. They detect even small lesions. Angiography and radioisotope scanning methods are required to clarify the characteristics of the blood supply and confirm the functional state of liver cells in the abscess area.
Diagnostic laparoscopy - insertion of an endoscope through an incision in the abdominal wall. It is carried out under anesthesia. Necessary for differential diagnosis with liver cancer, subphrenic abscess, purulent pleurisy and cholecystitis. It also allows you to drain the abscess and take material for analysis.
In the differential diagnosis of parasitic abscesses, a blood test for serological tests is used. It is positive if the patient’s body has antibodies to the supposed parasites (amoebiasis, echinococcosis, alveococcosis). Are used:
- indirect hemagglutination reaction;
- precipitation test;
- latex test.
Hydatid abscesses
Echinococcus is a helminth. The main host for it is a dog, and one of the intermediate hosts can be a person. The larva of this worm lives in the liver.
A person becomes infected through food or water. The helminth egg is absorbed into the blood in the small intestine. It reaches the liver and settles there. A colorless bubble is formed, which initially has a diameter of about 1 mm. It begins to grow and increases by an average of 2-3 centimeters per year. Over time, a large cyst forms. When it festeres, an abscess can develop.
Are there any special dietary requirements?
Patients are recommended to adhere to dietary table No. 5. It prohibits reception:
- fatty foods (meat, rich broths, confectionery, sour cream, cream);
- any canned and smoked meats;
- pickles and marinades;
- hot sauces, seasonings;
- whole milk;
- fried foods;
- eggs;
- fresh baked goods;
- carbonated drinks;
- strong coffee and tea.
It is necessary to build a diet:
- from low-fat fermented milk products (cottage cheese, kefir);
- boiled and stewed poultry meat;
- boiled fish;
- dried bread;
- vegetables prepared by stewing;
- fresh juices;
- fruit;
- porridge with moderate addition of oil.
To facilitate the digestion process, you should eat in small portions and more often than usual (6-7 times a day). The diet must be followed during treatment and after suffering a liver abscess for at least a year. And for patients with diseases of the digestive system - for life.
Treatment methods
Treatment of liver abscess must be comprehensive, and adherence to a special diet is an important factor on the path to recovery and elimination of a number of symptoms. For liver disorders, diet No. 5 is usually prescribed. It is based on excluding fatty, fried, smoked foods, coarse fiber (cereals, vegetables, fruits), yeast, baked goods, and fresh bread from the patient’s diet. Alcohol is excluded (for minor chronic diseases of the gastrointestinal tract, dry white wine is allowed, but an abscess is a completely different case), chocolate, custard cakes and pastries.
You need to eat meals in small portions, 5-6 times a day. Salt intake is limited to 3 grams per day.
On the contrary, they increase protein consumption: meat, fish, dairy products. As well as products with a high content of magnesium, zinc, vitamins B, C, A and K: bananas, buckwheat, almonds, peanuts, spinach, chicken eggs, sesame seeds.
With this diet, you are allowed to eat low-fat fish (tuna, pike perch, pike, pollock, hake), low-fat cottage cheese and cheese (in most cases, its fat content is 50%, so you need to choose feta cheese - its fat content is about 35%). The energy value of the daily diet varies between 2500-3000 calories depending on the patient’s weight. The amount of protein consumed is approximately 1.5 grams per 1 kilogram of weight, that is, in this regard there is virtually no strict quantitative limitation.
During treatment of a liver abscess, it is important to limit your activity and be at rest. The patient is prescribed bed rest; even the slightest stress must be avoided, as it weakens the body’s defenses. Drugs used for amoebic liver abscesses - metrogyl or metronidazole, emetine, chloroquine. The duration of treatment is 10 days, which is then reinforced with another 10-day course of metronidazole in doses reduced by half. If therapy does not produce results, they resort to draining the cavity of the lesion and washing it. At the same time, amoebas are eliminated from the intestines. If surgery is indicated, it is not performed until the intestinal abscess is eliminated.
After determining the type of causative agent of the purulent process, in an uncomplicated case, appropriate medications are prescribed. For bacterial infections, intensive therapy must be used. For amoebic infection, anti-amoebic drugs are used.
It is recommended to administer antibiotics not only intramuscularly, but also into the abscess cavity itself, taking into account the sensitivity of the microflora to the drug.
First, drainage (a syringe needle) is carried out through the skin, drainage is inserted into it and aspiration (removal) of the liquid contents is performed under ultrasound control. It is also possible to introduce a double-lumen drainage and wash it for some time with solutions of antiseptics and antibiotics. In mild cases, after such treatment, patients recover fairly quickly. When such therapy is unsuccessful, surgical methods are resorted to.
Surgical methods
Surgical treatment is preceded by puncture of the abscess under ultrasound control. Liver puncture is performed depending on the location through the intercostal spaces.
In case of viscous pus, a sodium chloride solution is first injected into the cavity, then sucked out with an aspirator
The procedure ends with inserting a conductor string into the needle, removing the needle and installing a drainage tube with side holes along the conductor. The drainage is attached to the skin with separate sutures. Through the tube, you can not only rinse the cavity, but also introduce a contrast agent. And from the photographs you can evaluate the size and quality of drainage.
The development of endoscopic surgery has made it possible to remove small abscesses. But large formations and lesions located in an area that is inconvenient for viewing are excised after an incision in the abdominal wall (laparotomy). Each abscess is carefully opened, and pus or other contents are removed using an aspirator. The empty membrane is washed with an antiseptic solution and then removed within healthy liver tissue.
With such an operation, the risk of pus releasing from the abscess when it is opened into the abdominal cavity and leaking between the intestinal loops increases. Therefore, special skills and experience of the surgeon are required. The patient's life depends on them. In case of cholangiogenic abscesses, after opening the abscess, the common bile duct must be drained for washing and subsequent rehabilitation of its inflammation (cholangitis).
Surgical treatment is necessarily accompanied by massive antibiotic therapy and other conservative methods of liver support.
Treatment
Treatment tactics are selected individually in each specific case. If there is one or more small abscesses, you can limit yourself to conservative treatment, which consists of long-term use of antibiotics and drainage of the pathological focus.
At the initial stages, drugs are prescribed by selection. To know exactly which microorganism is responsible for the development of inflammation, you need to wait for sowing, and this takes at least a week. Therefore, doctors prescribe an antibiotic that affects those pathogens that, according to statistics, most often cause this disease. When culture results come back, treatment is adjusted if necessary.
Medicines
Do not forget about symptomatic therapy. It includes detoxification of the body (Ringer's solution, saline solution), pain relief (ibuprofen), spasm relief (drotaverine), and intake of enterosorbents (smecta).
For multiple lesions, a combination of aminoglycosides and penicillins is usually used. Third generation cephalosporins can also be used. They have a wide spectrum of action and have proven themselves in this pathology. The drug of choice for amoeba infection is metronidazole.
If it is impossible to drain the abscess cavity, as well as in the presence of one or more foci of significant size, surgical treatment is performed. During surgery, the surgeon provides direct access (laparotomy), and then drains and sutures the cavity formed after the outflow of pus.
Surgical intervention
Complications
Untimely treatment of a liver abscess can lead to serious complications associated with breakthrough of pus:
- into the abdominal cavity (peritonitis);
- into the pleural layers (purulent pleurisy or pleural empyema);
- into the pericardium (pericarditis);
- under the diaphragm (subphrenic localization of the abscess);
- into the intestines or stomach.
A weakened body is not able to localize the infection in one place, so when pus comes into contact with blood, sepsis and the formation of ulcers in different organs (kidneys, lungs, brain) are possible. Corrosion of the walls of blood vessels by the inflammatory infiltrate is accompanied by massive internal bleeding with a drop in pressure, depression of cardiac activity, and the development of anemia.
Consequences
With proper and timely treatment, the liver abscess resolves, and a scar forms in its place. The connective tissue that has replaced the cells of this organ does not perform their function. Consequently, with a large lesion volume, chronic liver failure may develop. In some cases, with a significant size of the abscess, the cavity may persist. Later it becomes overgrown with connective tissue from the periphery to the center, and over time it disappears completely.
An unfavorable outcome of the disease occurs only in 7-9% of patients. In many ways, mortality also depends on the underlying disease, which caused the development of focal inflammation in the liver. The healing process takes a long time, mainly due to the need for prolonged drainage of the abscess.
Drug therapy
In cases of pyogenic bacterial abscesses, complex treatment includes antibacterial therapy. As a rule, it complements surgical methods of draining the abscess.
Isolated use of conservative treatment is rare, only in cases where the patient will not undergo surgery or when he has multiple abscesses that cannot be drained. In these cases, patients require many months of antibiotic therapy with constant and careful monitoring for the development of complications. Most often, antibiotics are prescribed in addition to surgical treatment.
Until the results of culture of blood or the contents of the abscess cavity are obtained and the type of pathogen is determined, doctors prescribe broad-spectrum antibiotics - carbapenems, third-generation cephalosporins and metronidazole. After receiving the results of the microbiological examination, treatment is changed, prescribing drugs based on determining sensitivity to them. The duration of antibacterial therapy can range from 6 weeks (for a single and well-drained abscess) to 3 months (for multiple liver abscesses).
- In the case of amoebic liver abscess, 90-95% of patients recover without surgery. They are prescribed metronidazole. Most patients experience improvement within 72-96 hours. If metronidazole is ineffective, chloroquine is used, to which emetine or dihydroemetine is sometimes added. After successful treatment of an amebic abscess, doctors prescribe diloxanide furoate, which destroys amoebas in the intestines.
- In case of fungal abscesses, systemic antifungal therapy is carried out. This treatment is in addition to surgical drainage of the abscess cavity. Doctors most often prescribe Amphotericin B or Fluconazole.
In addition to antibacterial or antifungal therapy, patients with a liver abscess may need fluid therapy (to correct fluid and electrolyte balance), pain medications, and correcting nutritional deficiencies.
Diagnostic methods
What to look for during diagnosis:
- symptoms indicating liver damage;
- signs of intoxication;
- the presence of an underlying disease that led to the formation of an abscess;
- physical examination data: increased liver size, local pain;
- data from additional research methods - laboratory and instrumental.
It is difficult to make a diagnosis based on the clinical picture alone; additional tests must be prescribed.
| Method | Results, features of the study |
| Complete blood count (CBC) | The CBC reveals signs of inflammation: an increase in the level of leukocytes due to neutrophils, the appearance of young forms of leukocytes, acceleration of ESR. |
| Blood chemistry | A biochemical blood test reveals signs indicating liver damage: increased levels of liver enzymes (ALT, AST), increased levels of bilirubin (mostly direct). |
| Bacteriological examination of the contents | To determine the pathogen and its sensitivity to antibiotics, bacteriological culture of the abscess contents is carried out. |
| Ultrasound examination (ultrasound) | One of the main diagnostic methods. With its help, you can detect a cavity in the liver that is filled with liquid contents. The size of the abscess and its location are determined. Abscesses larger than 1 cm are available for imaging. |
| Plain radiography of the abdominal organs | On the x-ray you can see a focus of clearing in the liver with a horizontal level of fluid. |
| Computed tomography (CT) | A more informative and specific research method is carried out in cases where ultrasound data is insufficient. The exact size of the formation, its localization and location relative to the parenchyma (superficial, deep), the nature of the contents, and the thickness of the capsule are determined. |