Data
· Pancreatitis is an acute inflammation of the pancreas (APG), which can spread to surrounding tissues.
· Successful treatment cannot take place without giving up alcohol and strictly following a diet.
· In most cases, inflammation of the pancreas is mild, but if the patient does not stop drinking and does not undergo drug treatment, the condition worsens and even leads to death.
· Therapy for ARVV includes a course of antibiotics, painkillers, and diet.
· In advanced cases, the disease requires surgical intervention - endoscopy.
Why does the disease occur?
If you look at the disease from a physiological point of view, it appears due to damage to gland cells by toxic metabolites of ethyl alcohol. Interestingly, pathology can appear after a single use of alcohol, and with its regular use. It turns out that the health of any person who decides to get drunk is at risk.
Experiments conducted by foreign scientists have demonstrated that alcoholism does not always play a major role in the progression of pancreatitis. More often, symptoms of the disease appear in people with a hereditary tendency to inflammation of the pancreas, as well as in the simultaneous presence of several provoking factors, for example, smoking, poor nutrition, and protein deficiency in the diet.
What is acute pancreatitis
The pancreas (PG) lies in the upper part of the abdominal cavity and is located behind, closer to the back. It produces enzymes that are released into the intestines through ducts.
Enzymes are important for digestion and complete breakdown of food. The pancreas also produces the hormone insulin, which controls blood glucose levels and the body's metabolism.
Acute inflammation of the pancreas due to alcoholism is a chemical inflammation of the organ. This process occurs both in isolation and spreads to neighboring tissues.
Eating too much is bad
Despite the fact that a person gets drunk much less when eating a large snack, people with a diseased gland need to moderate their appetite. Rich and heavy food (especially fatty or spicy) in combination with alcohol will definitely not do any good. If bile production is impaired, as well as taking into account the altered secretory activity of the affected pancreas, one can expect the development of pancreatic necrosis (in 50% of cases it ends in death). It is better to limit yourself in alcohol, and with it in snacks.
Be careful about advice from unreliable sources of information and various “folk” remedies. For example, you can find a recommendation to drink milk at the same time or after drinking alcohol, supposedly to help digestion. This is bad advice. Milk is quite difficult to digest, so it additionally burdens the gastrointestinal tract. Thus, alcohol poisoning will worsen, and the hangover will be more pronounced. Fermented milk drinks are another matter. If you have a hangover, you can safely use them, but not at the same time as alcohol.
Toxicologists generally do not recommend accompanying the consumption of alcoholic beverages with fatty and protein foods (meat, sausages, legumes). It is better to refuse them not only on the day of alcoholism, but also before it. This will reduce the content of putrefactive microorganisms that multiply in the intestines, and will also reduce the load and protect the pancreas.
If you feel that you have overate or drank too much, then it is better to artificially induce vomiting, no matter how strange it may sound. You will still have to pay for your incontinence - gluttony and drunkenness. So let it be a forced emptying of the stomach, rather than a “bouquet” of pain and suffering that will bring a hangover and inflammation the next day.
As a last resort, if you doubt that overeating can be avoided, then use enzyme preparations, for example, Mezim. It helps to digest heavy foods faster and better, and thus will reduce the additional load that falls on the gland and liver. They are already busy with the extremely complex process of “disposal” of alcohol, and extra help will not hurt them. However, do not think that enzyme preparations will protect against the negative effects of alcohol. Ethanol directly attacks pancreatic tissue, so there is no effective protection.
How common is pancreatitis?
This disease cannot be called rare. Systematic alcohol consumption significantly increases the likelihood of developing the disease and its complications. At least 2-3 thousand new cases of acute pancreatitis are recorded annually. People with cholelithiasis or those who abuse fatty, spicy and sour foods are also prone to this disease.
The incidence rate of pancreatitis is growing every year. This is partly due to advances in diagnosis and partly due to the higher prevalence of risk factors. For example, poor quality nutrition and excessive alcohol consumption .
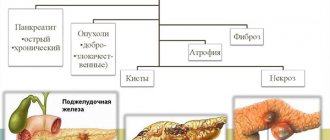
What forms are there?
The development of pancreatitis is possible in two scenarios:
- Chronic alcoholic pancreatitis occurs both independently and against the background of an advanced stage of pancreatitis. A similar form is observed even in people who drink minute doses of alcohol every day. True, it does not appear immediately, but after years, subject to the systematic use of alcoholic beverages. But more often, the chronic version develops with abuse.
- Acute alcoholic pancreatitis - a similar type is observed when drinking a large amount of alcohol at one time. The risk of damage increases if a person smokes and constantly eats fatty and low-protein foods. This is a particularly dangerous form with a severe course. Young men are most susceptible to it.
What Causes Pancreatitis
Alcohol abuse or biliary tract diseases are the most common causes of acute inflammation of the pancreas.
According to statistics, the presence of gallstones is the most common cause. Excessive drinking (alcoholism) ranks second.
Next on the list are hypertriglyceridemia, hyperparathyroidism, accidents, infections, certain medications and hereditary predisposition.
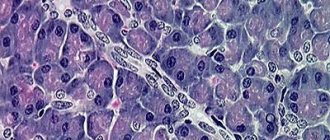
Acute inflammation of the pancreas occurs due to the leakage of digestive enzymes from the cells. These enzymes begin to destroy the gland and the tissue around it. The degree of inflammation ranges from mild swelling to cell death, bleeding from damaged blood vessels, and tissue dissolution.
Pathogenetic mechanisms of development
Destructive changes in the organ are characteristic; in the early stages, signs of fibrosis (replacement of parenchyma with connective tissue) are revealed. Also typical:
- edema;
- foci of necrosis;
- fatty degeneration;
- multiple cysts;
- calcifications and microliths due to changes in the composition and rheological properties of pancreatic juice.
Gradually, the organ becomes denser and enlarges; in the later stages, the reverse process is observed - atrophy. The ducts narrow and become clogged with a kind of “plugs” consisting of compounds with a protein structure.
Damage to the ductal system usually begins with small branches, and gradually larger ones are involved in the process. In severe cases of the disease, obstruction of the biliary tract and the development of obstructive jaundice cannot be excluded. Alcohol-induced changes in lipid peroxidation reactions play a major role. Oxidative stress “triggers” the processes of fibrosis and subsequent disruption of all organ functions.
Symptoms of acute pancreatitis
The disease is characterized by:
1. The presence of moderate or severe pain in the upper abdomen. The course of the disease can range from mild to life-threatening.
2. Pain occurs suddenly. They are strong and have a permanent character. Often aggravated by walking and running.
3. Unpleasant symptoms increase when a person sits down or leans forward. The pain may worsen for several hours before reaching a plateau that lasts for several days.
4. Pain may radiate to the back, chest, sides or lower abdomen.
5. Associated symptoms include nausea, vomiting, diarrhea, flatulence, hiccups and mild fever.
6. Unpleasant taste in the mouth, belching.
7. Dry mouth, feeling thirsty.
8. In advanced stages, weight loss and muscle weakness are observed.
9. With overeating and drinking alcohol, symptoms intensify.
Possible complications of acute pancreatitis
For most people, the initial stages of pancreatic inflammation are relatively mild and asymptomatic. But up to 15% of cases develop into serious diseases with severe peritonitis. A relapse is often observed when the diet is violated and alcohol consumption resumes.
In alcoholics, acute pancreatitis often occurs after 4-8 years of alcohol abuse. An exacerbation of symptoms occurs 6-12 hours after an episode of high consumption.
Complications such as fluid-filled cavities (pseudocysts) and abscesses may occur. In case of advanced acute inflammation of the pancreas, failure of internal organs can lead to the death of the patient.
Literature:
- Svanidze G. Sh. Clinic and surgical treatment of chronic pancreatitis of alcoholic etiology. Dissertation of a candidate of medical sciences: 14.00.27. USSR Academy of Medical Sciences. Institute of Surgery named after. A. V. Vishnevsky. - Moscow, 1989. - 30 p.
- Sadokov V. M. Alcoholic pancreatitis. Dissertation of Doctor of Medical Sciences: 14.00.05. - Moscow, 1992. - 42 p.
- Malykhin S.V. Optimization of treatment of acute pancreatitis complicated by delirium alcoholism. Dissertation of a candidate of medical sciences: 01/14/20. Place of protection: Research Institute of General Reanimatology of the Russian Academy of Medical Sciences. - Moscow, 2016. - 23 p.
Diagnosis of the disease
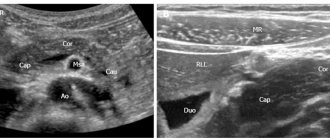
If acute inflammation of the pancreas is suspected, the patient is hospitalized. To confirm the diagnosis, the following examinations are prescribed:
· Blood test for amylase and pancreatic enzymes.
· Laboratory examination of stool.
· Biochemical urine analysis.
· Ultrasound examination of the abdominal cavity.
· Computed tomography of the stomach.
· Magnetic resonance imaging.
· Endoscopic examination (ERCP).
Less commonly, the patient is prescribed fibrogastroduodenoscopy, laparoscopy, and abdominal x-ray.
Revealing
It is not difficult to diagnose pancreatic inflammation - its signs are quite characteristic. The diagnostic process relies on:
- complaints;
- details of the anamnesis (history of the development of pathology);
- results of objective research methods (physical, instrumental, laboratory).
A number of details emerge from the anamnesis:
- is there a connection between the abuse of alcoholic beverages and the described disease;
- what is the “experience” of alcoholism against which the pathology arose;
- how regularly the “hot” is consumed;
- whether there were other factors that could provoke an inflammatory process in the pancreas (for example, a violation of the principles of a healthy diet).
Alcoholic pancreatitis is confirmed or excluded depending on a number of criteria. This:
- absence of complaints before the patient became addicted to alcohol;
- the absence of other causes that could provoke inflammation of the pancreas;
- relief of the condition that occurs when you stop drinking alcohol.
Physical examination includes:
- inspection;
- palpation (palpation of the abdomen);
- percussion (tapping);
- auscultation (listening with a phonendoscope).
Inspection is carried out:
- general
- the condition depends on the severity of the pathology; - local
- if flatulence occurs, bloating is detected.
The results of palpation will be as follows:
- pain is detected in the epigastrium and in the left hypochondrium;
- the stomach is soft;
- There are no symptoms of peritoneal irritation.
- In a thin patient, with deep palpation, an enlarged, compacted head of the pancreas is felt.
With percussion:
- pain in the epigastrium and left hypochondrium is confirmed;
- in the case of flatulence, a characteristic ringing sound appears, as if someone is knocking on a hollow object. Auscultation with abdominal bloating notes a weakening of bowel sounds. But if diarrhea is a concern, peristalsis may be increased.
Additional informative research methods include:
- instrumental - ultrasound, CT, MRI;
- laboratory tests - general and biochemical blood tests, coprogram.
Treatment of acute inflammation of the pancreas
Therapy comes down to the following activities.
· Strict adherence to diet.
· Treatment of alcoholism.
· Taking painkillers.
· Restoration of pancreatic function.
· Prevention of possible complications.
Thus, treatment is aimed at helping the patient in the acute phase and eliminating the cause of inflammation. Sometimes it becomes necessary to use a tube if the patient cannot eat food for 48 hours.
1. In severe cases, the patient receives intensive therapy in the hospital department. If inflammation is severe, painkillers are administered intravenously, feeding is provided through a feeding tube, and antibiotics are prescribed. You may also need to have surgery to remove gallstones.
2. For mild inflammation of the pancreas, following a diet, avoiding alcohol, detoxifying the body , bed rest and drinking plenty of fluids are sufficient measures to eliminate the symptoms of the disease.
Long term prospects
· If the cause of acute pancreatitis is gallstones, they must be removed to eliminate inflammation.
· If alcohol was the causative agent of the disease, the patient must undergo body cleansing and stop drinking alcohol. If it is not possible to do this on your own, the alcoholic needs to be coded .
· Even if the inflammation is caused by other reasons other than alcohol, doctors will recommend not drinking alcohol for at least one year.
· In some cases, acute pancreatitis is an isolated phenomenon. But with alcoholism, the disease returns and worsens.
· In some cases, the condition becomes quite serious. Complications may include peritonitis and chronic pancreatitis and may result in death.
About 15% of the country's general population is at risk. Among alcoholics, this percentage is many times higher.
Preventive measures: recommendations from doctors
Following some simple measures will help not only significantly reduce the likelihood of pancreatitis, but also detect it in a timely manner. Experts advise:
- Maintain moderation in drinking. It is better to avoid binge drinking and not to drink cheap surrogate drinks. Also prohibited are snacks rich in fat, which only enhance the negative effects of ethyl in the body.
- Review your daily diet. The menu must contain a sufficient number of protein dishes. It is protein deficiency that contributes to the development of the disease.
- Stop smoking. The lethal mixture of ethanol and nicotine leaves the pancreas no chance for uninterrupted operation.
It is also necessary to periodically undergo examination by a gastroenterologist. The doctor will promptly determine the malfunction of the gland, which will help stop the violations at the initial stages. Therapy in this case will be most effective.
Ethyl breakdown products can cause serious problems, and no body system is immune from them. That is why it is recommended to carefully monitor your general well-being and immediately go to a specialist , even if mild disturbances appear. Sometimes only this precaution is enough to prevent irreversible processes that threaten serious consequences.
Disease prevention
· If a patient has problems with alcohol, he should initially be taken out of the binge .
· The patient must abstain from alcoholic beverages for at least 1 year. In particularly advanced cases, refusal is recommended for the rest of life and can only be achieved with the help of alcohol coding.
· For triggered gallbladder disease, stones in the bile ducts are removed or the entire organ is excised.
· People at risk are advised to follow a diet, drink plenty of fluids, and take vitamin therapy.
The influence of strong alcohol
With pancreatitis, the patient is strictly prohibited from drinking alcohol in any form and in any quantity. If a person has developed a chronic addiction, he, as a rule, neglects these recommendations received from the doctor. If it is strong alcohol, then such carelessness will not only interfere with recovery, but can also provoke death.
Moreover, even a small dose can lead to pathological consequences. The ethanol contained in it is transformed into acetaldehyde, a toxic substance that destroys pancreatic cells, leading to problems with the normal functioning of the sphincter of Oddi and disturbances in the blood flow.
Thus, any strong alcohol has a destructive effect on the healthy pancreas; with pancreatitis, alcohol triggers irreversible pathological consequences that can provoke tissue necrosis. Even a small dose for a person in this condition can be fatal.
Sign up for a free consultation by phone
Over the phone, the doctor will collect a primary medical history, form a team, and inform you about the exact cost of the procedure and the time of arrival of the narcologist.
Promotion!
When ordering inpatient treatment - up to 20% discount
By clicking on the “Submit Application” button, you agree to the processing of personal data