Magnetic resonance imaging is carried out as an expert method of examination in identifying diseases of the pancreas.
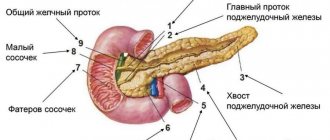
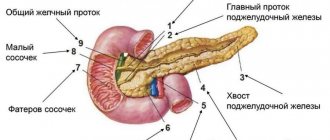
Modern units are able to level out artifacts associated with natural movements (blood flow through vessels, peristalsis, respiratory excursions). The use of phased arrays to enhance the magnetic field in the area of interest allows one to obtain layer-by-layer images of the organs of the biliary system with high contrast resolution. Evaluation of the pancreas is optimized with MR pancreatography demonstrating the ductal system and MR angiography demonstrating the vessels.
The doctor can examine enlarged images of the pathological lesion. Using computer modeling, three-dimensional image reconstruction is available.
Magnetic resonance scanning does not involve invasive penetration into the body, as with endoscopic retrograde cholangiopancreatography (ERCP), and can be performed on an outpatient basis. In the absence of contraindications, the diagnostic procedure is absolutely safe for humans.
Administration of a drug based on gadolinium chelates increases the differences in signal intensity between normal pancreatic parenchyma and altered tissue in malignant tumors. Enhanced MRI is useful in assessing acute pancreatitis and shows the area of necrosis in complicated forms. The study allows you to differentiate hypervascular formations of the pancreas, which can mimic cystic lesions on non-contrast scanning.
Pancreatic diseases
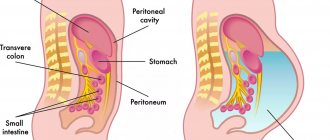
The pancreas is an organ of the digestive and endocrine system. The main functions are the production of pancreatic juice, which contains enzymes, and the production of several important hormones, including insulin. Located posterior to the stomach, closely connected with the duodenum. The pancreas consists of a head, body and tail; blood supply occurs through the pancreaticoduodenal arteries and veins. Most often diagnosed:
- Pancreatitis.
Magnetic resonance imaging for acute organ pathology
Acute inflammation of the pancreas is accompanied by severe pain in the upper abdomen. Other symptoms include nausea, vomiting, diarrhea, flatulence and fever. The cause of acute pancreatitis is gallstones, chronic alcohol consumption, hereditary diseases, injuries, medications, infections, electrolyte and hormonal disorders, high lipid levels, etc. If it is impossible to detect an internal factor, they speak of idiopathic (i.e., self-occurring) form. In the absence of adequate diagnosis and treatment, tissue necrosis occurs.
In acute pancreatitis, MRI shows the presence and degree of necrotization of the pancreas and the area of edema. Magnetic resonance imaging has advantages over CT in diagnosing subtle (initial) changes.
A standard MR scanning protocol of the pancreas, including T2WI, T1WI fat-suppressed and a series of T1WI, GRE sequences before and after gadolinium administration, is a reliable way to determine the stage of acute pancreatitis and the prognosis of the disease.
In severe acute pancreatitis, MRI of the pancreas with contrast is performed to assess parenchymal perfusion and the presence of necrosis. Organ enlargement is clearly visualized on any sequence, and parenchymal edema is better demonstrated on native T1 imaging.
MRI of the pancreas in chronic pancreatitis shows uneven expansion of the main duct with the formation of lateral branches, filling defects
Chronic pancreatitis is a progressive disease associated with the gradual destruction of the pancreas against the background of fibrosis and cellular infiltration, with the development of duct pathology and loss of exocrine and endocrine functions. Clinical manifestations are similar to the acute form. The advanced stage is characterized by underweight, anemia, and the development of type 2 diabetes. With a long-term ongoing process, MRI shows atrophy of the pancreas and pseudocysts. Changes are differentiated from tumor pathology.
- Pancreatic tumors.
Double duct sign on MRI indicates pancreatic cancer of the head of the organ
The majority of cases (85%) of malignant lesions are adenocarcinoma of ductal origin with typical localization in the head of the organ. Pancreatic cancer is difficult to detect at an early stage because there are no clinical manifestations. As the pathology progresses, abdominal pain, back pain, weakness, yellowing of the skin and sclera appear. Ultrasonography for tumors smaller than 3 cm shows ambiguous data. Multiparametric MRI with diffusion-weighted imaging and magnetic resonance cholangiopancreatography allow the analysis of morphological changes in the pancreatic parenchyma and duct.
- Cystic and pseudocystic neoplasms.
Multicystic lesion of the pancreas on MRI
Cysts and pseudocysts are detected during ultrasound scanning of the abdominal organs; often, when they are small in size, symptoms are nonspecific or absent. It is important to undergo an in-depth study to determine the malignant potential of the tumor. To make a diagnosis, gender, age, and medical history (trauma, alcohol intoxication, chronic diseases of the biliary system, etc.) are important. Final verification is possible after morphological examination.
Signs of cystic neoplasms of the pancreas:
- irregular contour, thickening of the walls;
- presence of partitions;
- visualization of solid components;
- dilated pancreatic duct more than 3 mm;
- calcifications, etc.
Symptoms of DIPZH
At the initial stage of chronic pancreatitis, swelling and slight hemorrhages appear in the tissues of the gland.
Signs of DI in tissues directly depend on the leading disease. The main symptoms include a feeling of heaviness in the stomach, frequent diarrhea and constipation. Acute pancreatitis is accompanied by an increase in pressure in the pancreatic duct, which causes its deformation.
Digestive enzymes penetrate the cells of the pancreatic tissues and lead to poisoning of the body. The patient experiences pain in the left area under the sternum, nausea, turning into vomiting. Blood pressure drops and pulse quickens. The condition requires urgent therapeutic treatment.
At the initial stage of chronic pancreatitis, swelling and small hemorrhages appear in the pancreatic tissues. Over time, the pancreas decreases in size, the connective tissue grows, replacing the deformed tissue of the enzyme-producing gland. As a result, the production of digestive enzymes is disrupted.
With fibrosis, healthy pancreatic tissue is also displaced and connective tissue is formed. The production of hormones and enzymes decreases. At the beginning of the disease, symptoms are not observed, or are similar to signs of pancreatic inflammation.
With lipomatosis, normal organ tissue is replaced by adipose tissue. The body begins to experience a deficiency of necessary hormones and digestive enzymes. The severity of lipomatosis depends on the volume of DPJ. With minor DI, pathology does not manifest itself. But in the process of growth of lipoid tissue, the parenchyma becomes compressed, as a result the functioning of the pancreas is disrupted and pain appears.
Is MRI performed for diseases of the pancreas?
The reason to sign up for a magnetic resonance examination of the abdominal cavity and retroperitoneal space is the detection in laboratory parameters of changes characteristic of damage to the organs of the biliary system
MRI for diseases of the pancreas is done to identify pathology, determine the stage of the disease and detect complications. The images provide the doctor with valuable information for making a diagnosis. The doctor analyzes:
- location, size and internal structure of the gland;
- zonation of the organ - features of visualization of the body, head and tail;
- involvement of parapancreatic tissue in the pathological process, spread of the tumor to nearby tissues, connection of the neoplasm with the pancreas, damage to the lymph nodes;
- configuration, tumor density, blood supply characteristics, presence of areas of necrosis, calcification (allows to differentiate benign and malignant processes);
- consistency of anastomoses after liver transplantation;
- changes in the parenchyma, the severity of inflammation;
- parasitic lesions;
- developmental anomalies;
- modification of the ducts of the pancreatic and biliary tract as a whole, the presence of strictures, localization, stone formation;
- changes in the retroperitoneal space etc.
Taking into account the absence of long-term consequences after the diagnostic procedure, the study is suitable for dynamic monitoring of cystic neoplasms and monitoring the effectiveness of therapy.
What types of disorders cause diffuse changes?
Diffuse changes in the pancreas reflect the formation of hyperechoic tissue structures, but do not indicate the variant of the pathological process that caused them. The most common types of violations are related to:
- with dystrophy;
- inflammation and swelling (with pancreatitis);
- replacement of healthy acini with fatty inclusions such as steatosis;
- fibrosis of the parenchyma (proliferation of scar connective tissue).
With the help of echo signs of diffuse changes in the pancreas, it becomes possible to establish the degree of development of the pathology and identify the proportion of remaining undamaged tissue. This is important for choosing the optimal treatment tactics in a particular case.
A lighter duct passes through the parenchyma, the grain pattern is similar to lipomatosis
MRI of the pancreas: indications
What is better, to do a magnetic resonance or computed tomography, the doctor decides, taking into account the clinical situation and restrictions on the use of the method
There are many indications for MRI of the pancreas. It is recommended to sign up for the procedure if:
- pain in the epigastric region, abdomen, indigestion, inexplicable by tests and ultrasound, appeared, indigestion - foul-smelling stool, unusual color of stool, nausea, vomiting, flatulence, jaundice, etc.;
- family history is burdened - several first-degree relatives have been diagnosed with pancreatic cancer;
- preoperative diagnostics are necessary to study the anatomical features and plan the intervention;
- ultrasound results are ambiguous/suspicious for pancreatic pathology, which implies advanced diagnostics;
- differentiation between cancer and chronic pancreatitis is required;
- deviations from the norm in laboratory parameters indicate disease of the pancreas, gallbladder, ducts, liver;
- there is a suspicion of a tumor in the biliary system, it is necessary to determine the stage of the oncological process, relapse after treatment;
- there are contraindications to computed tomography, including enhanced CT (pregnancy, childhood, allergy to iodine-containing contrast, renal failure, hyperfunction of the thyroid gland);
- There is no effect of therapy for pancreatitis / frequent exacerbations are observed when following a diet (MRI of the pancreas shows choledocholithiasis, intraluminal stones, stage of inflammation);
- it is necessary to exclude postoperative complications, etc.
Causes of diffuse reactive changes
The reaction from the pancreas occurs in response to various diseases of the digestive system. Moreover, on ultrasound they appear diffusely in the parenchyma. Most of all, the secreting function of the gland changes depending on the activity of the liver and the biliary system. In patients with cholecystitis, cholelithiasis, hepatitis, secondary pancreatitis may develop.
A violent reaction develops with symptoms of poisoning with drugs, industrial and household poisons. In the same way, changes in the pancreas occur in a child, with increased sensitivity or negative effects of medications.
In childhood, unexplained enzyme deficiency and abnormalities in the development of the biliary tract play a role. Ultrasound reveals signs similar to acute pancreatitis. A special feature is the more frequent localization of changes in the tail zone of the gland, expansion of the duct.
Ultrasound examination of the pancreas is included in a comprehensive examination of the abdominal organs
How is an MRI of the pancreas done?
The greatest diagnostic value is for images obtained on high-field units with a closed contour
Before scanning, you must leave items containing metal in the storage compartment. A cell phone or payment card forgotten in a pocket when exposed to a magnetic field causes distortion in the photo.
After completing the documentation, the x-ray technician escorts the patient to the diagnostic room and places him on the scanner table. The limbs are fixed with soft belts and bolsters, and an intensifying coil is placed above the abdomen.
If an MRI of the pancreas with contrast is planned, a catheter is inserted into the vein. During certain phases of the study, a chelated gadolinium enhancer will be automatically delivered through the drain (using an injector) to improve visualization.
Medical staff monitors the progress of the diagnosis through glass from an adjacent room. Communication takes place via speakerphone; in case of an unforeseen event (an attack of claustrophobia, deterioration in health), the patient has a special signal button at hand. Technical noise produced by equipment can be leveled out using headphones.
After the native series of images, there is a wait for the dye to spread through the bloodstream to the organs of the biliary tract. The duration of MRI with contrast is 30-45 minutes. The results will be ready within an hour. There are no obstacles to daily activities.
MRI of the pancreas, how to prepare?
Ask your doctor if you have any questions about MRI scans.
Magnetic resonance imaging is often performed routinely; in urgent situations with an acute abdomen, it is preferable to do a CT scan. Preparation for an MRI of the pancreas implies:
- Obtaining a referral for research. The document must indicate the intended diagnosis, area/s of interest, type - with or without contrast;
- Dieting. A few days before the procedure, products containing starch, yeast, sugar - baked goods, confectionery - are excluded from the diet. Excessive flatulence and fermentation processes in the intestines are caused by fresh vegetables (cabbage, peas, beans), fruits, herbs, mushrooms, milk, brown bread, etc. Alcohol, kvass and drinks with gas can cause the movement of small stones and accompanying inflammation, which will provoke swelling of the gland and gallstone colic. You should avoid fatty meats, fish, smoked meats, marinades, and spices. A 6-hour fast is required before the test. The paramagnetic gadolinium and prolonged lying on the back can cause autonomic reactions in the form of dizziness, nausea, and drooling. You can prevent such phenomena by having a light snack 30 minutes before leaving the house.
- Taking medications. Medicines for routine therapy are taken as usual. Antispasmodics, enzymes, adsorbents, laxatives are used exclusively on the recommendation of a doctor. An enema is needed for chronic constipation (if it is planned to examine all organs of the gastrointestinal tract).
Don’t forget to take with you the results of ultrasound, FGDS, images and descriptions of previously performed MRI/CT, epicrisis from the hospital, conclusion of the oncoconsilium. If the study is paid for by an insurance company, a compulsory medical insurance or voluntary health insurance policy will be required.
What can you eat before an MRI of the pancreas?
It is preferable to prepare dishes using gentle heat treatment - boiling, baking, stewing
To ensure that food is fully digested, the following are allowed on the eve of the procedure:
- lean meat, dietary fish, skinned chicken breast;
- baked vegetables and fruits;
- porridge with water;
- omelettes;
- unrich broths;
- crackers, dry cookies;
- vegetable oil in small quantities;
- unsweetened compotes, still water, herbal teas, diluted juices without pulp.
Normal size of the pancreas on MRI
Organ parameters are variable:
| Department | Dimensions (mm) |
| Head | 11- 35 |
| Body | 4- 30 |
| Tail | 7- 30 |
The concept of normal on magnetic resonance images is relative. Sizes depend on gender, height, age, food load. A slight deviation from generally accepted indicators, provided the structure of the organ parenchyma is normal and functions are intact, is not considered a pathology. The length of the pancreas is 15-23 cm, width 4.5-6 cm, weight about 70-80 grams.
Normally, the organ is not enlarged, the contours are clear, even, and the dimensions correspond to the person’s build. The pancreatic duct is not dilated, the surrounding tissue is without any features. No changes in the MR signal were detected.
The concept of echogenicity
During ultrasound, ultrasonic pulses are sent into human tissues, which, passing through them, encounter reflective surfaces along the way and are partially reflected. The reflected impulses are perceived by the sensor and converted into an image on the screen that is seen and analyzed by a specialist.
Echogenicity refers to the degree of reflectivity of tissue. The reflected signals are represented on the ultrasound scanner screen as many small dots corresponding to different shades of the gray scale. Echogenicity is determined not only by the nature of the structures being studied themselves, which give reflections, but also by the frequency of the sensor, the settings of the device, as well as possible interference during the study.
The echogenicity of an object of interest is always assessed relative to the echogenicity of other objects - surrounding tissues, adjacent or symmetrical organs. Thus, in the abdominal cavity, the echogenicity of organs is compared with the echogenicity of normal liver tissue or kidney parenchyma.
Let's take a closer look at such an important sign as the echogenicity of the pancreas.