Benign neoplasms of the pancreas are a group of tumor diseases based on the pathological process of uncontrolled cell division of the tissues of the pancreas and its ducts, characterized by a benign course.
The main diseases of this group are insulinomas (tumors originating from glandular tissue that produces the hormone insulin), fibromas (from connective tissue), hemangiomas (benign neoplasms growing from blood vessels), and cystic formations.
Benign pancreatic tumors are quite rare. In general, in the general statistics of all types of pancreatic tumors, benign tumors account for approximately 0.01 to 0.1%. Men and women suffer from this disease with equal frequency.
Etiology
Pancreatic cancer is more common among urban residents who consume large amounts of meat and fat. Smoking contributes to carcinogenesis in general and prostate cancer in particular (pancreatic cancer is registered 2-2.5 times more often in smokers than in non-smokers). It is assumed that carcinogens contained in tobacco can, under certain conditions, enter the pancreatic duct with bile, first provoking inflammation and then the formation of a tumor. Drinking large amounts of coffee (more than 3 cups per day) increases the risk of the disease, but the true cause-and-effect relationship remains unclear.
Pathological anatomy
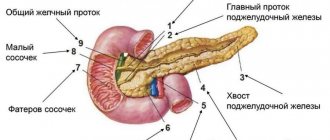
A pancreatic tumor is most often an adenocarcinoma growing from the ductal epithelium. Cancer of the head of the pancreas accounts for approximately 70% (in almost a quarter of these patients the tumor is localized in the uncinate process), the body and tail - 15-20%, the terminal part of the common bile duct and BDS - in 6-7% of cases in relation to all cancers of the organ.
At the time of diagnosis, the tumor in almost half of the patients has already spread beyond the pancreas, and in a third, distant metastases are detected.
Depending on the primary localization of the tumor, invasion of the latter can occur in various neighboring organs and tissues:
when the tumor is localized in the head - in the common bile duct, duodenum, portal vein, celiac trunk and its branches, mesentery of the transverse colon;
when localized in the body and tail - into the portal and splenic veins, common hepatic and splenic arteries, celiac trunk, aorta, stomach, mesentery and/or wall of the transverse colon.
Pancreatic cancer metastasizes early through the lymphatic tract and hematogenously. Regional lymph nodes are affected: pancreaticoduodenal, retropyloric, periportal (hepatoduodenal), pericelial, mesenteric, para-aortic. Hematogenous metastases are most often localized in the liver, much less often in the lungs, pleura, and kidneys.
Clinical picture of pancreatic cancer
Classic, although usually late, symptoms include weight loss, abdominal pain, loss of appetite to the point of anorexia, and jaundice. Weakness and fatigue, nausea, vomiting, diarrhea, dyspepsia and back pain appear quite often.
The clinical picture depends on the location of the tumor. The leading clinical symptoms of pancreatic head cancer are jaundice (92-98%), weight loss (65-80%) and pain (45-65%). With cancer of the body and tail, weight loss (more than 90%) and pain (more than 70%) are most often noted. At the same time, it was noted that with cancer of the uncinate process, the most common complaints of patients are pain (70%) and weight loss (50%), and jaundice, unlike cancer of the head of the pancreas, is extremely rare (about 15%) and is more late symptom.
It should also be remembered about the possibility of an erased clinical picture of pancreatic cancer and even the almost complete absence of clinical symptoms of the disease.
Pancreatic cancer should be suspected in a patient over 50 years of age who exhibits any of the following signs: 1) jaundice that occurs without a painful attack; 2) unexplained decrease in body weight by more than 10%; 3) unexplained pain or discomfort in the upper abdomen, especially with negative results of x-ray and endoscopic examination of the upper gastrointestinal tract; 4) unexplained lower back pain; 5) an attack of pancreatitis for no apparent reason; 6) exocrine pancreatic insufficiency without an obvious cause, manifested by unstable stools and frequent diarrhea; 7) sudden onset of diabetes mellitus without predisposing factors such as obesity or heredity
Laboratory and instrumental diagnostics.
With obstructive jaundice, an increase in bilirubin levels, an increase in alkaline phosphatase activity, and only a slight increase in transaminase activity are observed (in contrast to hepatitis). Increased amylase activity is unusual. In 50-60% of patients, changes are noted on radiographs: compression of the antrum of the stomach and duodenum, dilated duodenal loop. Scanning computed tomography is a more accurate method, especially when combined with needle aspiration and cytological testing (a negative result does not determine the diagnosis). Transhepatic cholangiography is a more optimal method for diagnosing obstructive jaundice than ERCP. RCCP may be useful in identifying neoplasms localized in the body/tail of the pancreas or pathology of the duodenal-ampullary region. Cytological analysis of a sample obtained during surgery by aspiration is of great help in difficult cases. Tumor markers are variable, the best being CA 19-9. Laparoscopy can be used to identify the stage of the disease and determine indications for resection.
Benign hormonally inactive tumors
Clinical picture The most common are adenomas, myxomas, lipomas, chondromas, lymphangymas, etc. If the tumors are small and do not compress the gland ducts, they may be asymptomatic. Compression and germination of nerve trunks leads to pain. When the tumor compresses the gland ducts, secondary obstructive pancreatitis develops. Obstructive jaundice may appear due to compression of the common bile duct by the tumor.
diagnostics helps determine the appearance of the tumor, its shape, and the presence of cyst-like inclusions. A computed tomography scan is performed and used as a method to clarify the diagnosis. The advantage of the method is non-invasiveness and the ability to visualize organs. Magnetic resonance imaging is a high-resolution technique. When analyzing the results of this study, a specialist can draw a conclusion not only about the prevalence of the tumor process and its connection with the vessels, but also suggest the histological structure of the tumor.
Treatment Only surgical treatment is performed.
Hormonally active tumors This is a rare type of tumor (insulinoma, apudoma).
Clinical picture Clinical symptoms are associated with hormonally active substances produced by tumors. As the size of the tumor increases, pain may appear. Some tumors can be malignant and metastasize to the liver. Tumors can be single or multiple.
Diagnostics Ultrasound, computed tomography, and magnetic resonance imaging are used to search for tumors. If necessary, angiography is used. Endoscopic ultrasonography makes it possible to diagnose 80% of small tumors. Scintigraphy provides the best results.
Treatment Treatment is surgical. For malignant growth, cytostatics are used.
GASTRINOMA
Clinical manifestations. The disease is characterized by the original Zollinger-Ellison triad: peptic ulcers with atypical localization and a fulminant, aggressive course, extreme hypersecretion of gastric contents and the presence of a non-P islet cell tumor of the pancreas. It can begin as a simple disease and end with the appearance of severe complications (perforation, obstruction, bleeding, refractoriness to therapy). Standard medical and surgical treatment is ineffective. There are cases accompanied by significant diarrhea and steatorrhea.
Diagnostics. Manifestations typical of gastrinoma include high basal secretion rates of VAO/MAO (= or >0.6), hypertrophied gastric mucosal folds, fasting hypergastrinemia (>200 pg/ml) or paroxysmal increase in gastrin levels in response to secretin administration, imaging pancreatic tumor using CT.
Pathology and pathophysiology. Gastrinomas are non-β islet cell tumors of the pancreas that range in size from 2 to 10 mm. There is varying evidence in the literature regarding the malignant potential of gastrinomas, although rates equal to or greater than 90% have been reported. The presence of gastrinomas in the wall of the duodenum is observed. Neoplasms grow slowly and metastasize late; The cause of death is often peptic ulcer disease. Cases of gastrinomas have been described as manifestations of MEA-1 syndrome (Wermer's triad: pituitary gland, parathyroid glands, pancreas), in which the tumors are distinguished by the fact that they are multiple and benign.
Treatment. The original treatment method is gastrectomy. However, the use of histamine H2 receptor blockers and omeprazole with or without proximal selective vagotomy can control the condition of patients with disease that cannot be resected.
List of signs of a high risk of cyst degeneration into cancer
There is a list of “alarming” signs of a pancreatic cyst that will serve as a signal for immediate surgical treatment:
- cyst size more than 3 cm;
- an increase in the diameter of the pancreatic duct (dilatation) of more than 6-10 mm;
- the presence of parietal nodes in the cyst;
- lymphadenopathy (enlarged lymph nodes);
- presence of complaints from the patient;
- thickening of the cyst walls;
The patient’s unfavorable family history (presence of pancreatic cancer in relatives), high level of the CA-19-9 marker is important; low levels of lipase and amylase, the occurrence of diabetes mellitus in the near future; age, overweight, mutations in certain genes, rapid tumor growth (more than 5 mm in 2 years), dysplasia of more than 30% of cells in a cytological study of the contents of the cyst.
All examinations are designed to identify the degree of danger of the cyst and answer one question: to operate or not to operate?
If there are no alarming signs, the pancreatic cyst is subject to regular observation, control and nothing more.
If there is evidence that the cyst is malignant, surgery is definitely necessary.
Pseudocysts are also treated promptly and very effectively.
OTHER ISLE CELL TUMORS
Lipomas can cause diarrhea, “pancreatic cholera”, WDHA syndrome (water diarrhea, hypokalemia, achlorhydria), 50% of them are malignant. Glkzagonoma is characterized by skin lesions (necrolytic erythema migrans), diabetes, glossitis, anemia, weight loss, depression and venous thrombosis; 75% of glucagon are classified as malignant tumors. The best treatment is resection. Clinical manifestations of somatostatin include diabetes, diarrhea, steatorrhea, achlorhydria, gallstones, malabsorption and abdominal pain. All of these symptoms are attributed to excess somatostatin levels. Streptozocin, dacarbazine, and doxorubicin are most often used in treatment.
Consultation on paid services
Show phone numbers
Hemangioma
Hemangioma
- a benign tumor that most often appears on the head and neck in girls. As a rule, vascular formation is detected in newborns.
The reasons for the formation are not clear. Presumably, this is a viral infection carried by a pregnant woman.
Symptoms of pathology
- Superficial formations are red or purple in color and have clear edges. When pressed, the formation turns pale.
- Cavernous hemangiomas are located under the skin in the form of blood-filled nodules.
- Combined hemangiomas are a combination of superficial and subcutaneous.
- Mixed formations consist of different tissues.
- Hemangiomas of the perineum and genital organs are prone to ulceration.
How is the diagnosis done?
- The problem is diagnosed by a surgeon using an external examination and laboratory data.
- Using ultrasound, the depth and location are determined, the speed of blood flow and the volume of the tumor are measured.
- For large tumors, angiography is used.
Hemangioma in adults is a rare phenomenon. Most often, localization occurs on the neck and face, less often - on the arm, on the finger, on the hand, in the anus, on the external genitalia. It does not degenerate into a malignant tumor.
Treatment
The disease is often treated by surgeons. Hemangioma should be treated immediately after detection:
- For deep-lying formations, surgical excision is used;
- For large areas, radiation therapy is used, acting in small fractions;
- Cauterization (diathermoelectrocoagulation) is used for point formations.
- For small complex formations, sclerosing treatment is used - alcohol injections.
- Treatment of combined hemangiomas requires the sequential use of cryogenic and injection therapy.
- Hormonal treatment is indicated for children.
- All simple small hemangiomas must be cauterized with liquid nitrogen.
- Over a large area, the use of hormonal and radiation exposure is indicated.
- For cavernous and combined lesions, surgical, cryogenic and sclerosing methods are effective.
- For formations in the parotid region, complex treatment using angiography and embolization is used.
The disease is often treated by surgeons.
If left untreated in young children, the formation may resolve over time. If the formation increases or complications arise, then it is not recommended to delay. Vascular tumors on the face should be removed early, as the risk of complications is too great.