Infectious disease specialist
Sinitsyn
Olga Valentinovna
34 years of experience
Highest qualification category of infectious disease doctor
Make an appointment
With the onset of hot weather, the risk of contracting typhoid fever increases. This severe infectious disease is most common in tropical and subtropical countries, especially with poor water supply and low levels of sanitation. In Russia, isolated cases of infection are recorded annually, localized mainly in the southern regions.
General information about the disease
The causative agent of typhoid fever is the bacterium Salmonella typhi. The infection is transmitted from person to person through water, food or contact with contaminated surfaces. With strict adherence to personal hygiene rules, the risk of infection is minimized.
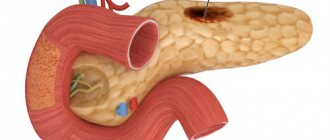
The infection affects the lymphatic system and digestive tract, spreading throughout the body through blood and lymph. Thanks to the presence of flagella, the bacterium actively moves within the intestine and penetrates through its walls into the blood vessels.
Typhoid bacillus can persist outside the human body for a long time. It does not encapsulate and does not leave spores, but when exposed to an unfavorable environment, it transforms into the cell-free L-form, which increases the resistance of the microorganism to drugs. However, it quickly dies when boiled and upon contact with antiseptics - alcohol, chlorine-containing substances and alkalis. At low temperatures, the bacterium can remain viable for several months.
Description
Typhoid fever is an acute cyclic intestinal anthroponotic infection.
It develops after the pathogenic bacterium Salmonella typhi enters the body through nutritional transmission routes. This means that the mode of movement of the infectious agent is from the infected organism to the susceptible immune system. It can get inside through already contaminated water, food or dirty hands. That is why it is important to follow basic personal hygiene rules. After infection, a person feels a feverish state, and the body is subjected to general intoxication. The body gradually develops a typhoid status, roseola rashes appear on the upper layers of the epidermis, as well as specific damage to the lymphatic system in the lower parts of the small intestine.
Features of the bacterium Salmonella typhi
The main causative agent of typhoid fever, Salmonella typhi, is an active gram-negative rod that has slightly rounded ends. It stains well if you use aniline dyes to identify it. After entering the body, the bacterium begins to produce endotoxin, which is considered pathogenic only for humans; the process occurs without the formation of spores.
Salmonella is quite resistant to environmental conditions. It can be found in bodies of water where there is fresh water. The bacterium retains its vital activity for one month if it is in liquid. But if it is placed in a milky environment, the bacteria begin to actively multiply and gradually accumulate.
How can you get typhoid fever?
The mechanism of transmission of typhoid fever occurs through ingestion of contaminated food or water. Patients who experience this disease can transmit the bacteria through water supplies after going to the toilet. The patient's stool contains a huge number of pathogenic microorganisms that are well preserved in water.
Some people have a mild type and degree of typhoid fever, so they are not even aware of its existence. It is also difficult to identify in everyday life. As a result, they remain carriers of very dangerous microorganisms for a long time.
Bacteria tend to multiply in the gallbladder, ducts and liver. A carrier of typhoid fever Salmonella typhi may not have any signs or symptoms, so he is unaware of his illness and poses a danger to healthy people. The pathogens retain their viability well in wastewater.
Types of typhoid fever
Increasingly, people are faced with the following types of typhoid fever:
- Typhus. It belongs to a separate group of infectious diseases, which in most cases develop after rickettsia enters the body. The main carriers of the disease from a sick person to a healthy person are body, head or pubic lice, which can spread lice. There are several varieties of this disease - this is epidemic typhus of the rickettsia species R.mooseri and Rickettsia prowazekii. Mice and lice act as pathogens and carriers of infections.
- Relapsing fever. This term is used to designate pathogenic spirochetes of the disease when lice and ticks act as carriers. In this case, the infectious disease of typhoid fever occurs with alternating symptoms. A person may suddenly feel an attack of fever, after which the body temperature returns to its normal value.
- Typhoid fever (dysentery). This is an infectious disease or intestinal anthroponosis, which begins to develop after salmonella bacteria enter the body. There are several clinical forms of this disease - typical and atypical.
There are also several stages of typhoid fever - mild, moderate and severe. For any manifestations of this disease, you must seek qualified medical help. It is also worth constantly observing the rules of personal hygiene, especially in public places.
In the initial phase of typhoid fever, the patient feels a lack of appetite, severe headaches, weakness, malaise, fever, diarrhea and a state of apathy. If no measures are taken in time, a person may experience a relapse of typhoid fever.
Are there complications with typhoid fever?
If you do not consult a doctor in time, the disease may develop into a more severe form, which will complicate the treatment and recovery of the patient. Several centuries ago, even before the introduction of chloramphenicol into medicine, typhoid fever became the cause of the development of severe asthenia, and led to rapid weight loss and malnutrition. In extremely severe forms of the disease, patients experienced internal intestinal bleeding and perforation of the large intestine.
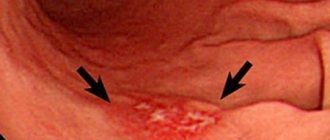
In the first case, erosion of blood vessels occurs in Peyer's patches, as well as places where there is a high accumulation of mononuclear cells in the intestinal walls. Patients note the appearance of blood streaks in the feces. Heavy bleeding occurs three weeks after the onset of the disease. The main clinical sign to pay attention to is a rapid decrease in blood pressure, blood pressure, and body temperature. These are specific complications of typhoid fever that need to be addressed immediately.
Intestinal perforation implies the development of a pathological process in the lymphoid tissue. Gradually, the infection spreads to the muscular and serous layers of the intestinal walls, resulting in its perforation. Antimicrobial drugs help to cope with clinical manifestations in the shortest possible time, as well as prevent complications.
The typhoid fever bacterium in some cases is localized in any internal organs, where it causes the formation of a local purulent process. These processes cause the development of meningitis, chondritis, periostitis, osteomyelitis, arthritis, and pyelonephritis.
The most common complications include pneumonia, which occurs after a bacterial infection enters the body.
Which doctor should I contact if I suspect typhoid fever?
If a person notices the first symptoms of typhoid fever, he should immediately seek advice from an infectious disease specialist. He will listen carefully to all the patient’s complaints and prescribe a full examination to determine the causative agent of the disease. The specialist will definitely pay attention to the medical history and also determine the epidemiological history. This includes identifying contact with infected patients or traveling to infected areas. Often, the doctor may require additional examination, after which he will prescribe the necessary treatment.
To determine typhoid fever, you will need to take cultures and smears for microflora, perform PCR diagnostics, biochemical analysis and blood markers. It is important to remember that the incubation period of typhoid fever is about two weeks, after which the disease begins to develop in an acute form. It is necessary to identify the disease in time for a quick recovery.
Typhoid fever in children
The transmission routes for typhoid fever are varied, and young children often do not wash their hands well after walking, so salmonella infections can easily enter the intestines. Parents will be able to notice the first symptoms very quickly. The child’s behavior and condition change, he becomes lethargic, physical activity decreases, as does his attitude towards his favorite toys.
The acute form of typhoid fever in children is characterized by the appearance of high temperature, fever, pronounced symptoms of intoxication, as well as the detection of roseola rashes on the skin. Children, unlike adults, are more likely to experience negative consequences, so it is important to promptly contact an experienced infectious disease specialist for qualified help.
Children require mandatory hospitalization, where they will receive complex treatment and a special diet. It is important to maintain careful oral hygiene and take care of your skin to protect yourself from developing stomatitis.
How does infection occur?
The main cause of typhoid fever is the penetration of infection into the human body through the oral cavity. Most often this happens when:
- drinking unboiled water containing the bacteria Salmonella typhi;
- swimming in a contaminated body of water;
- consumption of food products containing pathogenic bacteria - milk and dairy products, jelly, poorly fried minced meat, unwashed vegetables and fruits;
- contact with surfaces on which particles of saliva, urine or feces of an infected person remain.
Sometimes the infection is transmitted by flies, which on their legs transfer bacteria from the patient’s feces to food. There are known cases of mother infecting a child through breast milk. The source of infection is always a person - a patient in the acute phase, during an exacerbation, or a carrier of the bacteria. The release of bacteria into the external environment begins already on the seventh day after infection.
Periods of typhoid fever in adults
The disease occurs with a change in certain periods:
- incubation period - from the moment bacteria enter the body until the first symptoms;
- initial stage with nonspecific symptoms;
- peak or peak of the disease;
- stage of fading of symptoms.
Each stage has its own typical manifestations of symptoms, based on which doctors adjust treatment.
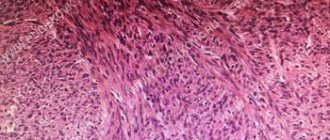
Damage to the large intestine during typhoid fever has distinct stages:
- first week - swelling of intestinal lymphoid formations (Peyer's patches and solitary follicles);
- second week – necrosis of lymphoid formations;
- third week – rejection of necrotic masses;
- fourth week – formation of clean ulcers;
- fifth-sixth weeks – healing of ulcers.
How to recognize an infection
The course of the disease includes four periods, each of which has its own characteristic features. Symptoms of typhoid fever are different for each phase of the disease.
- Incubation phase. It is characterized by a gradual increase in symptoms, which is expressed in general weakness, a gradual increase in temperature from physiological to 40 ° C, chills, headache, loose stools, decreased blood pressure and slowed pulse. At this stage, the signs of typhoid fever can easily be confused with influenza and other respiratory infections. A characteristic feature is a white coated tongue with teeth marks along the edges. The duration of the initial stage is 1-2 weeks.
- Acute phase. The temperature reaches a maximum and fluctuates in waves throughout the day or remains unchanged. Toxins from dying bacteria affect the nervous system, causing severe headaches, insomnia and lethargy. A characteristic red rash appears on the skin of the abdomen, sides and back. Inflammation of the intestinal tissue causes severe pain in the patient. This period lasts about 1.5-2 weeks.
- Resolution of the disease. The patient feels some relief: the temperature drops slightly, headaches decrease, sleep normalizes, and appetite appears. The improvement in well-being is explained by a decrease in intoxication of the body. The resolution period lasts about a week, after which a short-term return of the acute phase is possible.
- Recovery. Within about 2 weeks, the patient feels weak, inflammatory processes decrease, and the functions of the affected internal organs are restored.
Due to the widespread use of antibiotics, the clinical picture is often blurred and insignificant. Early diagnosis of typhoid fever is most complicated, since the incubation period in many patients is asymptomatic. In approximately 2/3 of cases, exacerbation occurs suddenly or with a very short prodromal period.
Are you experiencing symptoms of typhoid fever?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Publications in the media
Typhoid fever (BT) is an acute infectious disease (generalized salmonellosis), characterized by ulcerative lesions of the lymphatic system of the small intestine, bacteremia; manifested by intoxication, typical fever, roseola rashes on the skin, enlarged liver and spleen. Incidence : 0.12 per 100,000 population in 2001
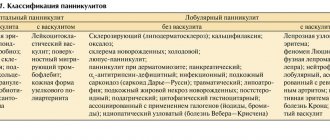
Classification • According to clinical forms •• Typical form (classical clinical variant) •• Atypical forms: ••• Erased ••• Subclinical ••• With a predominance of damage to individual organs and systems (colotif, meningotif, pneumotyphoid, etc.) • By severity: •• Mild form •• Moderate form •• Severe form • By course: •• Uncomplicated •• With complications and relapses.
Etiology . Salmonella typhi is an aerobic gram-negative rod of the Enterobacteriaceae family.
Epidemiology • BT is an anthroponotic disease. Sources of infection are sick people and bacteria carriers. The greatest epidemiological danger is posed by bacteria carriers and patients with erased and mild forms of the disease. Chronic bacteria carriers are the main reservoir of infection in nature • Summer-autumn seasonality is typical • The mechanism of infection is fecal-oral. The water factor is of primary importance in the occurrence of epidemic outbreaks of BT. Contact-household and food transmission routes cause sporadic cases of the disease.
History • Contact with a patient with BT or a bacteria carrier 1 month before the onset of the first symptoms of the disease • Stay of the patient in a region that is epidemiologically unfavorable for BT.
Clinical picture
• Periods of the course •• Incubation (7–25 days, on average 12–14) •• Initial (4–7 days) •• Height of the disease (1–2 weeks) •• Resolution of the disease (up to 1 week) •• Reconvalescence ( 2–4 weeks).
• Clinical symptoms •• Fever is the most consistent objective symptom. BT is characterized by 3 types of temperature curves ••• Trapezoidal Wunderlich temperature curve - classic, with a sequential change of stages of increasing body temperature, constantly high values and decline; their duration corresponds to the initial period of the disease, its height and resolution ••• Botkin’s wavy temperature curve with a sequential alternation of 3-4-day episodes of febrile and subfebrile body temperature ••• Kildyushevsky’s temperature curve with a short (1-2 days) stage of constantly high temperature and a long (2–2.5 weeks) decline stage; typical for children • • Intoxication (anorexia, headache, insomnia) - at altitude the development of delirium, psychotic states and disorders of consciousness (status typhosus) is possible • • Damage to the gastrointestinal tract - thickened tongue coated with a gray-brown coating with tooth marks on the lateral surfaces ( typhoid tongue), shortening of percussion sound over the ileocecal area (Padalka's symptom), pain and infiltration determined by palpation of this area (Obraztsov-Gausman symptom), symptoms of enterocolitis (flatulence, diarrhea with stool in the form of pea puree or constipation), colotyphoid • • Hepatosplenomegaly (determined by palpation from the end of the first or beginning of the second week) • • Skin lesions - pallor of the skin, roseola rash protruding above the surface of the skin (roseola elevata), not abundant, discrete, appears on the 8-12th day of illness, localized on the skin of the chest and abdomen, persists for 3–4 days and disappears without a trace. During the period of resolution, elements of prickly heat (crystallina miliaria) and yellow discoloration of the skin of the palms and feet (Fillipovich's symptom) may appear. • Damage to the cardiovascular system - bradycardia and dicrotia of the pulse, moderate arterial hypotension. With the development of complications - collapse, tachycardia • • Damage to the central nervous system - meningitis and meningoencephalitis of a serous and purulent nature, meningotif • • Damage to the respiratory system - infiltrative forms of pneumonia, pneumotyphoid • • Damage to the kidneys - symptoms of nephritis or hemolytic-uremic syndrome, nephrotyphoid.
Laboratory studies • Isolation of the pathogen or detection of its Ag •• Bacteriological method: sowing and isolation of the pathogen from blood (hemoculture), feces (coproculture), urine (urinoculture), bile (bilinoculture), bone marrow (myeloculture); positive results of pathogen isolation are an absolute diagnostic sign of BT •• Immunofluorescent analysis methods for detecting pathogen Ag in biological fluids • Detection of antibodies to pathogen Ag in the RNGA •• AB to O-Ag (thermostable lipopolysaccharide, endotoxin) is detected in the first week of the disease •• AT to H-Ag (heat-labile, flagellated) is recorded in convalescents and vaccinated people, appears on days 6–8 of the disease and persists during the period of convalescence; a simultaneous positive result of the reaction with O- and H-Ag with a predominance of O-agglutinin titers indicates an actively ongoing process •• Antibodies to Vi-Ag (heat-labile, somatic) do not have diagnostic or prognostic value, the reaction is used to identify carriers (positive reaction - 1:5 and higher) and vaccinated (Vi-Ag is included in vaccines) • CBC - leukopenia, relative lymphocytosis, aneosinophilia; an increase in the number of eosinophils in peripheral blood is a prognostically favorable sign.
Differential diagnosis is carried out with all diseases with a gradual increase in body temperature during the first 5–7 days and with high body temperature that persists for more than a week, especially if no other causes of its occurrence are identified. Wunderlich's rule: the diagnosis of BT is unlikely if on the 1st or 2nd day a body temperature of 40 °C is noted, and on the 4th day the body temperature does not reach 39 °C.
TREATMENT
• Mandatory hospitalization.
• Bed rest until the 10th day of normal body temperature.
• Diet with mechanical, thermal and chemical sparing; diet No. 2, complex of vitamins.
• Causal treatment - antibiotic therapy, does not prevent the development of relapses, complications and chronic bacterial carriage • • Chloramphenicol. Treatment regimen for adults: 0.5 g 4 times a day until the 4th day of normal body temperature, 0.5 g 3 times a day until the 8th day and 0.5 g 2 times a day until the 12th day of normal body temperature. The treatment regimen for children is the same, but the initial dose is 75–80 mg/kg/day, followed by a dosage reduction by 25% and 50%, respectively. The drug is recommended to be taken 1 hour before or 2 hours after meals, washed down with plenty of water • • Ceftriaxone 30 mg/kg/day IV or IM in 2 divided doses (1 g every 12 hours) or cefoperazone 60 mg/ kg/day IV in 2 doses for 14 days • • Ampicillin 1.5 g orally 4 times a day or amoxicillin 2 g 3 times a day until the 10th day of normal body temperature (for 4–6 weeks during carriage) • • Co-trimoxazole, ciprofloxacin, ofloxacin.
• Symptomatic therapy - relief of intoxication (infusion detoxification therapy), improvement of repair processes of the intestinal mucosa and correction of metabolic disorders (infusions of immunoglobulins and other blood products, vitamins).
• Treatment of emergency conditions •• For infectious-toxic shock - infusion of plasma replacement drugs (for example, polyglucin), GC in high doses (prednisolone up to 30 mg/kg IV or dexamethasone for 48 hours, first 3 mg/kg IV, then 1 mg/kg every 6 hours), dopamine, sodium bicarbonate • • For intestinal bleeding - strict bed rest, cold on the stomach, fasting for 8-10 hours, infusions of blood products, fibrinolysis inhibitors; if possible - abstain from surgery • • In case of perforation of the intestinal wall - emergency surgery.
Complications can develop with mild or even erased forms of BT • Intestinal bleeding develops at 2–3 weeks of illness, accompanied by a sudden decrease in body temperature (“incision” of the temperature curve), increased heart rate, disappearance of its dicrotia, decreased blood pressure, clearing of consciousness (apparent well-being) , tarry stools (sometimes mixed with scarlet blood). With massive bleeding, death is possible • Typhoid perforation of the intestine occurs at 3–4 weeks of illness, and can be single or multiple. Symptoms: abdominal pain localized in the right iliac region (the first few hours), symptoms of peritoneal irritation, sudden decrease in body temperature, tachycardia, increased leukocytosis • Infectious-toxic shock is typical for severe forms, observed during the first week of the disease.
Current and prognosis . The course of BT is relapsing. Relapses in typhoid-paratyphoid diseases mean the return of the main symptoms of the disease during periods of resolution and convalescence against the background of normal body temperature. Relapses appear in the first 1.5-3 weeks of the convalescence period, and sometimes later - after 2-3 months of normal body temperature; there can be several of them - from 1 to 9 (usually one). Each relapse is accompanied by bacteremia, and its clinical picture does not differ from that during the main wave of the disease. The fundamental difference is the short duration of manifestations (7–10 days). With timely and adequate treatment of BT and its complications, the prognosis is favorable.
Prevention • Prescription of convalescents no earlier than 21 days from the moment of normalization of body temperature and receipt of negative results of a three-time bacteriological examination of feces, urine and a single study of bile (bile is examined on the 10th day of normal body temperature) • The first collection of material is carried out on the 5th day of normal body temperature , and then at 5-day intervals • Convalescents are subject to 3-month dispensary observation to identify possible relapse and bacterial carriage • Active prevention is carried out in regions with high incidence rates (25 or more cases per 100,000 population) using combined chemical vaccines • Children up to Typhoid bacteriophage is prescribed for 7 years • Disinfection is carried out at the source of TB • Contact persons are placed under medical observation for 25 days with daily thermometry and mandatory bacteriological examination of feces and urine • General measures: strict control of the quality of drinking water and the activities of production, processing and sales enterprises food products.
Features of BT in children • Infants, due to their dietary habits and relative isolation from potential sources of infection, rarely get sick • With age, the risk of the disease increases • Predominance of symptoms of gastrointestinal tract damage - frequent vomiting, diarrhea, up to the development of intestinal toxicosis • Temperature curve or the wrong type, or Kildyushevsky type • Intoxication is manifested by central nervous system excitation (restlessness, psychomotor agitation, convulsive seizures, meningism) • Complications are rarely observed • Absence of characteristic bradycardia • Favorable course.
Reduction . BT - typhoid fever
ICD-10 • A01 . 0 Typhoid fever
Diagnosis methods
The most reliable methods for diagnosing typhoid fever today are laboratory tests.
- Agglutination reaction to detect antibodies to the Salmonella typhi antigen. This test is carried out two weeks after infection. Its disadvantage is the possibility of a false positive result if another Salmonella bacterium is present in the body.
- Indirect hemagglutination. The test can detect typhoid fever during the first week of illness.
- ELISA. This method is highly accurate and allows you to determine the presence of any antibodies to bacterial antigens. Its advantage is the ability to conduct the test at all stages of the disease, including during the recovery period.
For general clinical and bacteriological studies, samples of the patient’s blood, feces and urine are taken. During the last phase of the disease, duodenal intubation is performed, during which a sample of the contents of the duodenum is taken.
Treatment
Photo: cbroadcasting.net
Typhoid fever is diagnosed and treated by infectious disease doctors. All patients undergo therapy in an inpatient setting. Hospitalization is required for the following reasons:
- the disease is infectious;
- there is a risk of infecting others;
- the development of dangerous complications is possible;
- Availability of quality care is the key to a complete successful recovery.
Patients are prescribed a special diet. Etiotropic and symptomatic treatment measures are carried out. Procedures to combat typhoid fever are aimed at neutralizing the infection, increasing the body's immunity and stopping the transmission of the infectious disease. It is also necessary to pay attention to prevention.
Diet
Therapeutic nutrition has a gentle effect on the intestines and does not cause fermentation (putrefactive) processes after consumption. In order for food to be easily digestible, it must be semi-liquid (broths, soups) or rubbed through a sieve. The diet for typhoid fever is high in calories. Frequent consumption of food in small portions is recommended. Drinking plenty of fluids is recommended, preferably warm tea.
Patient care
In addition to the above measures, the patient is recommended to rest in bed for 7-10 days. The prescription must be strictly followed, otherwise straining the abdominal muscles may lead to bleeding or perforation of the intestine. Subsequently, gradual activation is carried out. It is necessary to observe hygienic conditions, both in patient care and in nutrition. Discharge is permitted no earlier than 23 days from the date of admission.
Treatment of typhoid fever in children
Children and adolescents with this disease are also subject to mandatory hospitalization in a hospital. Patients are usually isolated in separate rooms to prevent outbreaks and spread of infection.
During the period of fever, an infectious disease doctor prescribes bed rest and careful care of the skin and oral cavity. A special diet with the necessary nutrients, vitamins, and microelements is prescribed. The specialist uses antibiotics and symptomatic medications in appropriate age-appropriate dosages. In case of severe intoxication, infusion therapy is carried out.
Vaccination
According to epidemiological indications, vaccination of the population is carried out by subcutaneous injection of a liquid anti-typhoid drug into the shoulder. WHO recommends three types of vaccines. Each of them has its own characteristics, a certain adaptation period and dosage.
Vaccination is recommended for those traveling abroad to the countries of Latin America, Africa, and Asia. The optimal time for administering the vaccine is a week before the trip. The average duration of vaccination is 3 years. If you have a history of this procedure, you should consult your doctor about the age of the last vaccination and the relevance of the new one.
Prevention of typhoid fever
As part of prevention, the following activities are carried out:
- It is necessary to strictly follow established sanitary and hygienic rules (from maintaining personal hygiene to organizing water supply).
- You should wash your hands often with warm water and soap.
- According to indications, you should get the appropriate vaccination.
- In areas with poor sanitation, it is recommended to consume only bottled water.
- When the first signs of the disease appear, you should immediately consult a doctor.
Disease prevention also includes supplying the population with high-quality water, timely removal of garbage and sewage from populated areas, insect control, and isolation of infected people.
How to cure
Since the infection is extremely virulent, and the disease is severe and often complicated, treatment of typhoid fever must be carried out in the infectious diseases department of the hospital, in conditions of complete isolation. During illness, the patient remains in bed and does not leave the infectious disease ward. Therapy continues until the patient's body temperature returns to normal for ten consecutive days and includes:
- taking antibiotics (orally or by injection);
- replacement of fluid losses (orally or intravenously);
- a gentle diet with a high content of protein products;
- in case of intestinal perforation - surgical removal of a section of intestine with multiple injuries or closure of a single perforation with drainage of the peritoneum.
Taking antibacterial drugs continues for several months. Constant monitoring of patients' condition allows for timely detection of complications and prevention of their development. After discharge from the hospital, the patient is monitored at the dispensary for a certain time.
References
1. Bogomolov, B.P. Infectious diseases: Textbook for students of medical universities / M.: Moscow State University Publishing House, 2009. 2. Clinical recommendations (treatment protocol) for providing medical care to children with typhoid fever. FSBI NIIDI FMBA of Russia M.: 2015. - P. 85.
3. Andrews, J., Ryan, E. Diagnostics for invasive Salmonella infections: Current challenges and future directions / Vaccine. 2015. - P. 8-15. doi:10.1016/j.vaccine.2015.02.030. 4. Crump, J, Sjölund-Karlsson, M, Gordon, [et al.]. Epidemiology, Clinical Presentation, Laboratory Diagnosis, Antimicrobial Resistance, and Antimicrobial Management of Invasive Salmonella Infections / Clinical Microbiology Reviews. 2015. - Vol. 28(4). — P. 901-937. doi: 10.1128/CMR.00002-15. 5. Heiman, F, Horby, P, Woodall, J. Atlas of Human Infectious Diseases / First Edition // Blackwell Publishing Ltd, 2012.
Epidemiology, risk factors and disease burden
Improved housing conditions and the introduction of antibiotics have led to a sharp decline in the incidence and mortality of typhoid fever in industrialized countries. However, in developing countries in the African, American, South-East Asian and Western Pacific regions, the disease continues to be a public health problem.
WHO estimates the global burden of typhoid fever to be 11–20 million annual cases and 128,000–161,000 deaths per year. Populations without access to safe water and proper sanitation are at increased risk of disease. Poor communities and vulnerable groups, including children, are most at risk.
WHO activities
In December 2022, WHO prequalified the first typhoid conjugate vaccine. It provides longer-lasting immunity than older vaccines, can be used in lower doses and can be used in children over 6 months of age. This vaccine will be used primarily in countries with the heaviest typhoid burden. This will help reduce the use of antibiotics to treat typhus, which will slow the rise of antibiotic resistance in Salmonella Typhi. In October 2022, the Strategic Advisory Group of Experts (SAGE) on Immunization, which advises WHO, recommended typhoid conjugate vaccines for routine use among children over 6 months of age in typhoid-endemic countries. SAGE also called for the priority introduction of typhoid conjugate vaccines in countries with the highest burden of typhoid fever or widespread antibiotic resistance in Salmonella Typhi. Shortly after this recommendation, the GAVI Council approved US$85 million in funding for typhoid conjugate vaccines to begin in 2022.