Periodic or constant pain in the chest when swallowing can be a sign of many problems and diseases - from a cold to a foreign body in the human body. The main reason is a pathological process in the digestive system. Any problems with the gastrointestinal tract most often arise and develop unnoticed and practically asymptomatic. But if, when swallowing, it hurts in the middle of the chest or radiates to other areas, you cannot ignore it. Trying to relieve pain and self-medicating is not recommended. It is better to consult a general practitioner
who will determine the exact cause and prescribe the correct treatment. Everything should happen under the supervision of a specialist.
Chest pain when swallowing: causes
Painful discomfort can be associated with various disorders in the body. Pain when swallowing is caused by viruses and colds, allergies, foreign bodies in the throat or esophagus, as well as diseases of various systems and internal organs. If you experience pain while eating or swallowing, then most likely there are problems with the esophagus, and the pain radiates to the sternum. The problem may be associated with disturbances in the contractions of the esophagus, with the emergence and development of pathologies, with the passage of food into the stomach, with inflammation or erosion of the mucous membrane, etc. What do you need to remember? If, when swallowing food, pain appears in the chest area (on the left, right or in the middle), then this rarely indicates problems and diseases of the chest - more often there is a symptom of gastrointestinal tract pathologies, including oncological ones.
How is diagnosis carried out?
To determine the exact cause of pain when swallowing, you need to undergo a diagnosis from a gastroenterologist. To begin with, the doctor collects anamnesis, interviews the patient and performs palpation (physiological examination).
To check the wall of the esophagus and stomach, laboratory research methods are used:
- radiography;
- fibrogastroduodenoscopy;
- determination of gastric juice concentration;
- manometry;
- Ultrasound of the chest and stomach.
Patient examination methods are aimed at assessing motor function. If erosions, tumors or ulcers are found during diagnosis, a biopsy is prescribed. The resulting biopsy specimen (biomaterial) is sent for histological examination. This will help determine the nature of the tumors - malignant or benign.
Possible diseases
What led to the pain and how serious the problem is, only a specialist can say. Therefore, if it is difficult and painful for you to swallow, do not delay visiting a doctor, because you risk missing the onset of a serious illness and worsening your health condition.
Esophageal diverticula
Diverticulum is a dangerous disease that can lead to a large number of suppurations and ulcers in the neck and the development of pneumonia. It all starts with the fact that the walls of the esophagus are stretched due to the occurrence of hernial formations. They interfere with normal swallowing of food and cause severe pain. The first signs of the disease are bad breath, sore throat and further painful swallowing.
Esophagitis
This is an inflammatory process in the esophageal mucosa that causes pain when eating. Pain syndrome occurs in separate parts of the esophagus, or it hurts entirely. The intensity and nature of the pain resembles an attack of angina pectoris and responds with pain behind the sternum.
Esophagospasm
A disease of esophageal motility, in which painful sensations appear both when eating and drinking water, and at rest (for example, during sleep) or under severe stress when a person is worried. Pathology develops when the nerve plexuses are disrupted or when the mucous membrane is damaged.
Cardiospasm
Pathology develops when a narrowing and subsequent expansion occurs in the lower part of the esophagus. When the situation worsens, the patient develops anemia and vitamin deficiency, as well as constant belching and nausea.
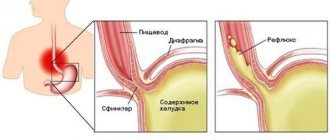
Gastroesophageal reflux disease
This is a chronic disease that manifests itself in the form of hydrochloric acid from the stomach entering higher parts of the digestive tract. In this case, the mucous membrane of the esophagus is constantly injured, and the person experiences more and more pain when swallowing. The pathology is accompanied by a severe cough and constant sore throat. The disease can be recognized if heartburn torments every day for several hours a day and for several months in a row. If left untreated, the disease will lead to the development of ulcers and possibly esophageal cancer.
Lapina T.L. Esophageal pain // Medical Bulletin. – 2006. – No. 32 (375). - October 11. - With. 16.
Esophageal pain
T.L.
Lapina A detailed and complete description of such an important symptom as pain allows the doctor to “find” the correct diagnosis, assess the stage of the disease and possible complications.
Pain in diseases of the esophagus
is often very “eloquent”, clearly indicating the nosological form, but there are also frequent situations when chest pain requires a broad differential diagnosis, and it is not easy to identify its connection with esophageal pathology.
T.L. Lapina, associate professor of the course “Functional diagnostics and pharmacotherapy in gastroenterology” at the Department of Family Medicine of the MMA named after. THEM. Sechenov
It is necessary to determine whether the pain is caused by swallowing or not. Pain when swallowing
is called
odynophagy
.
If there is no connection between pain and swallowing, it is called spontaneous. As a feature of odynophagia, its possible combination with dysphagia should be noted. Dysphagia
, which is defined as difficulty, obstruction or discomfort during swallowing (that is, when food passes through the oral cavity, pharynx and esophagus) when pathological changes in the esophagus become more severe, can indeed develop into odynophagia or become an additional symptom when painful swallowing occurs.
Odynophagia
, unlike spontaneous pain, as a rule, very clearly indicates that
the pain belongs to the esophagus
. Diseases of the esophagus with odynophagia are often accompanied by destructive changes in the mucous membrane: chemical burn of the esophagus, infectious esophagitis (especially viral - herpetic, cytomegalovirus, but also bacterial and fungal), drug esophagitis, erosive and erosive-ulcerative esophagitis with gastroesophageal reflux disease, esophageal tumors. The severity of odynophagia can vary, be minor and occur only when swallowing solid food or hot drinks, or it can accompany every meal and be extremely painful. Odynophagia can make the patient refuse to eat. We observed a young woman who came to the clinic with complaints of intense pain behind the sternum when passing solid and liquid food (the most severe pain was localized in the middle third of the sternum); a feeling of difficulty in passing food in the middle third of the sternum and constant pain along the esophagus, especially in the middle third of the sternum, which was so pronounced that in order to alleviate it, the patient took a forced position (lying on her stomach or tilting her body forward in a vertical position) . Thus, in one case there was a combination of odynophagia, dysphagia and esophageal pain; not related to swallowing. The complaints were due to a large ulcer localized on the posterior wall in the middle third of the esophagus, the formation of which was caused by taking a nutritional supplement. If the pain is not caused by swallowing (or is not associated with other typical esophageal symptoms, such as heartburn), then it can be difficult to determine its cause, since pain localized to the chest is very common. Even in the most general terms, it is necessary to differentiate a number of possible sources/causes of pain (see table).
Table. Causes of chest pain
Cardiac
| Non-cardiac | |
| - ischemic - non-ischemic |
|
Determine the true cause of chest pain
It's not always easy.
Thus, according to SR Achem (2005), in the USA in the late 80s. last century, when conducting coronary angiography, up to 30% of those examined did not have damage to the coronary arteries of the heart: with a general count throughout the country, up to 300 thousand cases of non-cardiac pain in the chest could be detected annually. When analyzing domestic data from coronary angiography of 425 patients, changes in the coronary vessels were not detected in 9.4% of cases, and the diagnosis of gastroesophageal reflux disease was established in 6.4%. The following should be listed as causes of esophageal pain: acid-peptic factor during reflux; smooth muscle spasm; stretching of the esophagus; damage to the sensory nerve endings of the esophagus during tumor growth. Accordingly, gastroesophageal reflux disease is most often accompanied by esophageal pain. It is recognized that in 50% of patients with noncardiac chest pain, the cause of pain is precisely gastroesophageal reflux. More rare causes of pain are diseases caused by movement disorders (esophagospasm, achalasia cardia) and tumors. With esophagospasm, the pain is intense, localized in the sternum or high in the epigastric region, radiating along the front surface of the chest up to the neck, into the lower jaw, shoulders, occurring either spontaneously or when swallowing food or saliva, or during neuropsychic stress. With achalasia cardia, the pain is localized at the level of the lower third of the sternum and usually occurs after eating due to overstretching of the esophagus with stagnant contents. With gastroesophageal reflux disease, pain is also localized behind the sternum, can be pressing, burning, radiates to the back, often occurs in the supine position and after eating, decreases or disappears after taking antacid or antisecretory drugs. To establish the esophageal cause of chest pain, it is necessary to carefully question the patient. The combination of pain with other esophageal symptoms (heartburn, dysphagia) significantly helps in the interpretation of the pain syndrome. With a typical clinical picture of gastroesophageal reflux disease, proton pump inhibitors can be immediately prescribed, treatment of which is likely to lead to the disappearance of pain. In the absence of a clue in the form of typical esophageal symptoms, a detailed instrumental examination may be required. An X-ray examination of the chest (to exclude lung diseases) and an ultrasound examination of the abdominal organs (to exclude pancreatobiliary pathology) are advisable. X-ray examination of the esophagus and stomach will make it possible to establish a diagnosis of esophagospasm, achalasia cardia, tumor, but for most cases of reflux disease it will be uninformative. The importance of endoscopy also cannot be overestimated, since pain can be a manifestation of non-erosive (endoscopically negative) reflux disease. 24-hour pH monitoring
has been repeatedly studied as a method for objectively identifying the cause of non-cardiac chest pain.
Its diagnostic value is debated. About 40% of patients with noncardiac pain demonstrate pathological acid reflux, a positive symptom index. However, recorded acid reflux may in some cases not indicate the presence of reflux disease, including as a cause of non-cardiac pain. Esophageal manometry
, unfortunately, cannot be considered as an optimal diagnostic test. According to WG Paterson (1998), pathological manometry data are found in 60% of patients with non-cardiac chest pain, but the identified changes are insignificant, atypical (that is, not characteristic of esophagospasm), regarded as nonspecific motor disorders and are unlikely to have significant clinical significance . In addition, episodes of non-cardiac pain may be irregular, which also makes their diagnosis difficult. Carrying out manometry with provocative tests (acid perfusion, betanicol stimulation or balloon distension of the esophagus) in most cases allows to initiate pain syndrome and increases the accuracy of diagnosis, however, it becomes difficult and uncomfortable for the patient. It becomes obvious that a simple and informative test with a proton pump inhibitor (for example, omeprazole) serves as a very attractive diagnostic method for gastroesophageal reflux disease with extraesophageal manifestation - non-cardiac chest pain. If after a trial course of a proton pump inhibitor the pain goes away, then it was caused by reflux. Thus, F. Cremonini et al. (2005), in a meta-analysis of studies undertaken to compare the proton pump inhibitor test with endoscopy and pH monitoring, found that the sensitivity of the test was 80% and the specificity 74% for diagnosing this condition. The same authors conducted a meta-analysis of eight randomized controlled trials to evaluate the effectiveness of a proton pump inhibitor treatment for noncardiac chest pain compared with placebo. The risk of continued episodes of non-cardiac chest pain after treatment with a proton pump inhibitor was 0.54 (95% CI (confidence intervals) 0.41-0.71), NNT (number needed to treat) - 3 (95% CI 2-4 ). It was concluded that proton pump inhibitors may be used to treat non-cardiac chest pain. A recent review of the literature on this topic (JR Malagelada, 2004) recommends the possibility of prescribing a proton pump blocker for non-coronary chest pain at a standard dose for a short course of treatment, for example one week, which may be sufficient to relieve pain. Other drug approaches to the treatment of esophageal pain include nitrates and calcium channel blockers (for hypermotor dyskinesias of the esophagus), as well as antidepressants.
Esophageal injuries
If a patient comes to the doctor asking why there is pain in the middle of the chest when swallowing, then the doctor must determine the cause. This is often associated with trauma to the esophagus, which may be:
- received due to various types of damage: gunshots, stab wounds, incised wounds, etc.;
- associated with internal pathological processes: neoplasms, narrowing, expansion in different areas (neck, thoracic region, etc.);
- associated with various pathologies of body systems, for example, damage to large vessels;
- received due to damage during surgical treatment, for example, during intubation, neck injuries, etc.
The type and duration of treatment depends on the type of injury and the severity of the damage.
Treatment
Help before diagnosis
Most non-drug measures are aimed at preventing pain between the shoulder blades: developing and maintaining correct posture, eating a balanced diet without harmful foods, leading an active lifestyle and playing sports. In case of severe pain during the diagnostic search, the doctor prescribes non-narcotic analgesics, recommends limiting mobility, and, if necessary, prescribes strict bed rest.
Conservative therapy
In the treatment of back pain between the shoulder blades, a differentiated approach is used - the therapeutic regimen is selected individually, taking into account the leading disease that caused the symptoms and concomitant pathologies. In case of orthopedic problems, posture correction with the help of corsets and other orthoses comes to the fore. The following groups of medications are used to treat the causes of pain:
- Nonsteroidal anti-inflammatory drugs
. Prescribed to relieve discomfort in diseases of the osteoarticular system, as well as to eliminate inflammation and speed up recovery. NSAIDs are also effective for diseases of the respiratory organs and mediastinitis. - Antisecretory drugs
. Proton pump inhibitors and H2-histamine blockers are the basis for the treatment of GERD and achalasia cardia. The drugs reduce damage to the esophagus from acidic stomach contents and relieve pain. To quickly relieve the burning sensation, non-absorbable antacids are taken. - Antibiotics
. Massive antimicrobial therapy is indicated for acute forms of mediastinitis to destroy pathogens and prevent bacterial complications. Medicines are selected empirically. A combination of 2-3 agents is introduced to act on all possible types of microbes. - Cytostatics
. Polychemotherapy is selected for some forms of mediastinal cancer as preparation for surgery or as palliative care. Immunosuppressants are sometimes recommended for patients with severe forms of ankylosing spondylitis.
Patients with acute conditions (aortic dissection, fulminant mediastinitis) are hospitalized in the intensive care unit. The goal of treatment is to get rid of the state of shock: for this purpose, cardiotropic medications, infusion solutions are used, and oxygen support is provided. To relieve pain, narcotic analgesics and tranquilizers are administered.
Non-drug methods play an important role in the treatment of musculoskeletal diseases. Special exercise therapy complexes are prescribed to strengthen the muscle corset and form an even posture. Manual manipulation, kinesiotherapy, orthopedic massage of the chest, back, and lower back show good results. A number of physiotherapeutic methods are used: electrical stimulation of the back muscles, peloid therapy, general ultraviolet radiation.
Surgery
For persistent deformities of the spinal column, surgical correction of scoliosis is recommended. Surgical treatment for osteochondrosis is resorted to in the case of spinal compression: the intervertebral hernia is removed and the spinal canal is decompressed. As a rule, minimally invasive techniques are used: puncture vaporization of the disc, microdiscectomy.
Surgical interventions are indicated for complicated forms of diaphragmatic hernia and severe stenosis of the esophagus. The hernial orifice is sutured with crurorrhaphy, gastropexy or fundoplication, resection and plasty of the esophagus. Emergency surgery is the only treatment for a dissecting aneurysm. Vascular surgeons perform resection of the damaged area with reconstruction of the aorta.
Symptoms
The pathology has quite varied symptoms, which largely depend on the type of damage, causes, concomitant diseases and duration of the disease. The main symptoms include:
- bad breath, burning, heartburn, cough, shortness of breath, difficulty breathing;
- sharp pain (most often behind the sternum);
- low pressure;
- decreased appetite, weakened immune system, gastrointestinal problems;
- pale skin color, blue mucous membranes, etc.
The first and most obvious symptom is problems with swallowing.
Inflammation of the esophagus. Esophagitis
11.10.2019
The esophagus is a hollow organ of the digestive system that connects all organs to the stomach . Its length is approximately 24 cm. The connection between the esophagus and the stomach is called the gastroesophageal junction, and immediately below is the lower sphincter, which comes from the esophagus.
The purpose of this sphincter is to prevent stomach acid and food from returning esophagus . In a number of painful conditions, the esophageal sphincter ceases to function. One such condition is inflammation of the esophagus.
Esophagitis is a disease that is an inflammation of the lining of the esophagus. The esophagus allows food to pass from the throat to the stomach , so inflammation can cause severe swallowing problems and even ulceration of the esophagus. Inflammation of the esophagus can be severe or chronic.
Causes of inflammation of the esophagus
There are two main causes of inflammation of the esophagus - infectious and other. Infections include fungal and viral infections, as well as bacterial infections. Other causes of inflammation may include Crohn's disease , alcohol abuse, physical injury, and chemical damage from acidic and alkaline solutions (vinegar). The most common cause, however, is gastroesophageal disease.
Types of inflammation of the esophagus
In principle, esophagitis is divided into specific and reflux (peptic). Reflux is inflammation caused by the reflex of throwing food back into the esophagus. Prerequisites for this condition are frequent vomiting (due to gastritis , ulcers or other diseases). Returned gastric juice contains pepsin and hydrochloric acid, and these are the main causes of inflammation.
Specific esophagitis most often occurs in bronchopulmonary tuberculosis and is therefore also known as tuberculous esophagitis . The disease is very serious because ulcers or even swelling can occur.
esophagitis is also known . It forms after long-term treatment with antibiotics, in people with a compromised immune system , as well as in diabetics. There is also so-called eosinophilic gastritis , which is an allergic inflammation of the esophagus and is less common.
Symptoms of inflammation of the esophagus
Inflammation of the esophagus often occurs without symptoms. If it is not very strong, a person may feel discomfort while eating. Severe forms are characterized by severe pain and fever. It is possible that the pain even reaches the neck or back .
Increased salivation, stomach , and in more severe cases the patient may vomit blood . Symptoms should not be ignored and consultation with a doctor is mandatory.
Among the most common signs of esophagitis are cough, difficult and painful swallowing, nausea , possible vomiting, heartburn and belching with a smell, decreased or complete absence of appetite.
Published in Gastroentorology Premium Clinic
Diagnostics
The doctor will determine which examinations will be needed during the initial consultation. To do this you need to see a therapist
who will give recommendations and directions, or you can immediately go to
a gastroenterologist
who will prescribe an endoscopy of the stomach and esophagus.
X-rays (with and without contrast agent), ultrasound
of certain internal organs, checking the functioning of the cardiovascular system and additional studies and tests (for each specific case) may also be prescribed.