Often patients come to the appointment who have had an endoscopic examination of the stomach and in the conclusion the specialist writes: “chronic gastritis, intestinal metaplasia.” While our patients have heard a lot about chronic gastritis, intestinal metaplasia causes anxiety and thoughts about malignant lesions of the stomach. Is it so?
The term “chronic gastritis” means chronic inflammation of the stomach, but we are not talking about the entire wall of the stomach, but only the mucous membrane, in which, along with inflammatory and atrophic processes, a disorder in the renewal of cells of the gastric mucosa develops, which is an important sign of gastritis and can determine the prognosis of chronic gastritis .
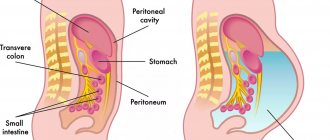
Learn more about the gastric mucosa
The gastric mucosa is characterized by constant cellular renewal. With any damage to the gastric mucosa, regeneration is activated, which leads to the restoration of the structure of the mucosa. Evidence of impaired cellular renewal in chronic gastritis is the characteristic changes in the mucosa, disruption of the phases of cellular renewal, which are well known to morphologists and are defined as disturbances in the morphological restructuring of the gastric mucosa in the form of intestinal metaplasia and mucosal dysplasia.
Therefore, when conducting an endoscopic examination, it is necessary to carry out multiple biopsies of the gastric mucosa in order to confirm the diagnosis of chronic gastritis, in which a qualitative disturbance in the regeneration (restoration) of cells and their replacement with cells unusual for the stomach or its parts can be observed, i.e. We are talking about replacing the gastric epithelium with intestinal epithelium. Metaplasia (from the Greek “formation, formation”) is the persistent replacement of cells of one type with cells of another type while maintaining the species identity of the tissue.
Causes
The main reasons for the development of the disease include:
- inflammation of the gastric mucosa caused by various factors;
- gastrointestinal irritation;
- chronic esophagitis - inflammation of the tissues of the esophagus;
- long-term gastritis - especially with increased stomach acidity. In most cases, the development of metaplasia is associated with the bacterium Helicobacter pylori. The microorganism affects the immune system and adapts to its changes, causing damage to the gastric epithelium of varying severity;
- frequent stressful situations;
- chronic reflux - esophagitis - exposure to irritating factors on the mucous membrane of the esophageal walls for more than six months. Inflammation occurs when gastric juice leaks or leaks into the esophagus;
- hormonal disorders.
What is intestinal metaplasia
Intestinal metaplasia was described more than a hundred years ago and is still being studied mainly because of its possible association with gastric cancer. Intestinal metaplasia is quite common. In old age, it is also found in practically healthy people, but especially often with atrophic gastritis, almost 100%. For stomach ulcers - 81%. For duodenal ulcers – 47%. Stomach cancer ranks 4th in the structure of cancer diseases.
The level of pepsinogens in the blood is a marker of chronic atrophic gastritis and the risk of developing stomach cancer. Therefore, determining the level of pepsinogens and Helicobacter pylori infection using a blood test improves the detection of chronic atrophic gastritis and stomach cancer.
If a patient is suspected of having chronic atrophic gastritis (according to the gastropanel results), gastroduodenoscopy with multiple biopsies of the gastric mucosa is indicated. Histological confirmation of intestinal metaplasia is the most reliable marker of atrophy of the gastric mucosa. Patients diagnosed with chronic atrophic gastritis with intestinal metaplasia are at risk for developing stomach cancer (gastric adenocarcinoma).
Risk factors for intestinal metaplasia may include:
- Helicobacter pylori infection,
- poor nutrition,
- genetic factors
- ecological environment,
- smoking,
- duodenogastric reflux - bile reflux into the stomach,
- disturbance of intestinal microflora.
The use of folk remedies
Traditional medicine offers no less effective methods of combating the disease. Decoctions and infusions of medicinal herbs and herbs reduce signs of inflammation and relieve pain.
- Herbal mixture of chamomile, calendula, yarrow and marshmallow root. Take 1 tsp. each herb, mix and steam 0.5 liters of boiling water. Leave in a thermal container for about an hour. Filter and take 3-4 times a day for 30 minutes. before meals, 20 ml.
- Pour boiling water over flax seeds (1 tbsp) and boil for 5 minutes. Leave for 1-2 hours, take 30 ml before each meal.
- St. John's wort. Grind 15 gr. dried herbs, steam 200–250 ml of boiling water. Leave to infuse in a thermos for 12 hours, preferably overnight. Filter the mixture and bring the volume to 250 ml. Take 30 minutes before. before meals, 50 ml of infusion. The course of treatment is 14 days, then take a week break.
Photo gallery: popular folk remedies in the treatment of gastric metaplasia
St. John's wort has astringent properties, prevents the appearance of malignant neoplasms
Chamomile, yarrow, calendula, calamus root have an anti-inflammatory and wound-healing effect
A decoction of flax seeds protects the mucous membrane from the harmful effects of gastric juice
Intestinal metaplasia - types
Currently, two types of metaplasia are distinguished - complete , resembling the mucosa of the small intestine, type 1 metaplasia and incomplete, resembling the mucosa of the colon, type 2 metaplasia.
Complete intestinal metaplasia
It occurs most often in chronic gastritis. The small intestinal epithelium, which forms areas of metaplasia, is generally less prone to malignancy (cancerous degeneration). A well-known factor is the rarity of small bowel cancer. Therefore, complete intestinal metaplasia is not considered a precancerous change in the mucosa. If manifestations of chronic gastritis are observed, then dynamic observation and gastroduodkeroscopy are carried out after 3-5 years.
In the diet, it is recommended to consume foods that have enveloping properties - rice water, jelly, baked fruits, jams with pectin, herbs - flax seed.
Incomplete intestinal metaplasia
It resembles the mucous membrane of the colon and is detected in 11% of patients with all benign diseases of the stomach, but in stomach cancer it is observed in 94% of cases. Incomplete intestinal metaplasia showed a higher specificity of this sign of changes in the gastric mucosa to cancer, but low sensitivity (38%) indicates its limited value as an indicator of prognosis for the development of intestinal cancer. An important factor in this case is the large area of replacement of normal gastric epithelium with intestinal epithelium.
There is a known connection between chronic atrophic gastritis, intestinal metaplasia and Helicobacter pylori, in which the elimination of Helicobacter can prevent the development and progression of atrophy, and the reverse development of atrophy of the gastric mucosa is also possible. The presence of intestinal metaplasia is a sign of Helicobacter gastritis. Patients with incomplete intestinal metaplasia are monitored dynamically annually.
Incomplete intestinal metaplasia of the gastric mucosa often progresses to the next stage of mucosal restructuring - dysplasia of metaplastic epithelium.
Symptoms of the disease
Intestinal metaplasia itself does not manifest itself. All symptoms relate to ailments that preceded its development. Doctors identify the main signs of the disease:
- nausea;
- aching pain in the epigastric region;
- loss of appetite.
The epigastric region is the part of the abdomen in the upper, middle area just below the ribs
With increased acidity of the stomach, heartburn and “hunger” pains are observed, which intensify at night. If the disease is accompanied by reflux of gastric contents into the esophagus, vomiting and a feeling of bitterness in the mouth may occur.
Morphological diagnosis of stomach diseases
Dysplasia of metaplastic epithelium is a morphological diagnosis. We can talk about it in the presence of cellular atypia and disruption of the structure of the cells of the gastric mucosa. Depending on the severity of these changes, 3 degrees of dysplasia are distinguished:
- 1 - weak,
- 2- moderate,
- 3 - pronounced or severe degree.
The concept of dysplasia was proposed to designate precancerous changes, the formation of high-risk groups for observation and preventive treatment. Studies of the development of dysplasia have shown that in patients with grade 2 dysplasia, progression to grade 3 dysplasia was found in 4-8%.
Literature
- Balasubramanian G. et al. Cigarette smoking is a modifiable risk factor for Barrett's oesophagus //United European gastroenterology journal. – 2013. – T. 1. – No. 6. – pp. 430-437.
- Coleman HG et al. Tobacco smoking increases the risk of high-grade dysplasia and cancer among patients with Barrett's esophagus //Gastroenterology. – 2012. – T. 142. – No. 2. – pp. 233-240.
- Hooi JKY et al. Global prevalence of Helicobacter pylori infection: systematic review and meta-analysis //Gastroenterology. – 2022. – T. 153. – No. 2. – pp. 420-429.
- Jarosz M., Taraszewska A. Risk factors for gastroesophageal reflux disease: the role of diet //Przeglad gastroenterologiczny. – 2014. – T. 9. – No. 5. – P. 297.
- Liu KSH, Wong IOL, Leung WK Helicobacter pylori associated gastric intestinal metaplasia: Treatment and surveillance //World journal of gastroenterology. – 2016. – T. 22. – No. 3. – P. 1311.
- Olmez S. et al. The prevalence of gastric intestinal metaplasia and distribution of Helicobacter pylori infection, atrophy, dysplasia, and cancer in its subtypes //Gastroenterology research and practice. – 2015. – T. 2015.
- Tang SJ, Wu R., Bhaijee F. Intestinal Metaplasia of the Stomach // Video Journal and Encyclopedia of GI Endoscopy. – 2013. – T. 1. – No. 1. – pp. 187-189.
Observation of patients with dysplasia 1 and 2 degrees
For mild dysplasia , detected in people over 60 years of age against the background of severe gastritis, it is recommended that repeat endoscopies with biopsies be performed after 12 months and then every 3 years.
severe dysplasia are detected in biopsy samples of the gastric mucosa, multiple repeat biopsies should be performed after 6-12 months, since severe dysplasia often indicates not that the patient may develop cancer, but that it already exists. And even if cancer has not yet been detected, then surgical treatment is recommended for such patients - surgical or endoscopic resection due to the high likelihood of developing adenocarcinoma (stomach cancer). In 25%, high-grade dysplasia can progress to adenocarcinoma within a year.
Otherwise, simply dynamic observation, even with many biopsies during endoscopy when confirming severe dysplasia of the gastric mucosa, may end up wasting time for diagnosing early gastric cancer and timely treatment and recovery.
Diet
Treatment will not be complete without proper nutrition. Patients are recommended:
- exclude dairy products from the menu, as well as those that irritate the gastric mucosa (fried, spicy, salty);
- do not drink alcohol, coffee, carbonated drinks;
- meals should be fractional, at least 5–6 rubles/day;
- last meal – 2–3 hours before bedtime;
- The diet must include fresh vegetables and fruits.
Nutritionists advise introducing a variety of cereals into your diet. It is recommended to eat food only warm.
Too hot food irritates the gastric mucosa, while cold food takes a long time to digest and provokes the release of hydrochloric acid.
Photo gallery: foods you can eat
You can eat steamed meat. It retains many beneficial substances for the body, which are so necessary during illness.
Fresh and steamed vegetables will not harm the stomach and will be an excellent addition to the diet
The absorbent properties of rice porridge are successfully used to effectively remove toxins and waste.
Treatment of patients with grade 3 dysplasia
Patients diagnosed with chronic atrophic gastritis with dysplasia , which is associated with highly virulent Helicobacter pylori strains, have an increased risk of developing stomach cancer. Eradication of Helicobacter pylori can lead to regression of atrophic processes in the stomach and reduce the risk of stomach cancer. For dysplasia, eradication of Helicobacter pylori, rhythmic nutrition, and protection of the gastric mucosa from damage by drugs are required.
If the examination reveals a low level of pepsinogen I and a low pepsinogen I/pepsinogen II ratio, this is already a serious stage of atrophic gastritis. Gastroduodenoscopy with multiple biopsies is recommended, even in cases where a serological test (determining antibodies in blood serum) for Helicobacter pylori did not reveal infection in the stomach.
Morphologists in biopsy samples of the gastric mucosa, using the new staging system for atrophic gastritis (OLGA), summarize the indicators of atrophy in the body and antrum of the stomach and determine the scores in each biopsy. Stages III and IV of the severity of atrophic gastritis according to this system indicate a high reality of the development of stomach cancer