Viral hepatitis poses a serious problem for society and the state. According to statistics, about 50 million people become infected every year, and almost two million die.
Hepatitis C in 90% of cases becomes chronic and leads to cirrhosis or liver cancer. The insidiousness of the disease is that it does not have characteristic signs at an early stage and proceeds like an acute respiratory viral infection.
Therefore, pathology is diagnosed either by chance or at a stage when irreversible processes have already passed in the body. Every year the state suffers large losses due to the increase in the incidence of hepatitis C.
This is due to the high cost of treatment. Only 3% of patients have the opportunity to be treated under the compulsory medical insurance policy. The rest have to buy medicine at their own expense.
About the disease
The hepatitis C virus tends to change
Hepatitis C refers to chronic viral pathologies of an anthroponotic nature. In other words, the causative agent of the virus is viable only in the human body. The causative agent is a microorganism of the flavivirus family.
Medicine knows 8 types of virus, which are divided into 100 subtypes. The pathogen has the ability to mutate and create quasitypes. Therefore, it has not yet been possible to invent a vaccine against hepatitis C.
Chronic hepatitis
The reason for the chronicity of the pathology is ignoring symptoms and lack of therapy in the acute period. After the infection progresses to the chronic stage, the manifestations become less pronounced.
The patient feels decreased ability to work and deterioration of cognitive functions, as viral cells affect the nervous system. Periodically, the patient experiences exacerbations. Without appropriate therapy, relapses become more frequent and various complications develop.
A man can also suspect the presence of an infection by various skin rashes. They appear due to decreased blood clotting and the accumulation of large amounts of toxins. Skin manifestations of the disease:
- Acne that cannot be treated.
- Small red dots concentrated on the bends of the elbows and knees (hemorrhagic diathesis).
- Blueness of the skin (marbling).
- Swelling of the veins on the abdomen (jellyfish head).
Chronic hepatitis has a negative impact on the endocrine system. Men develop erectile dysfunction, female-type obesity, gynecomastia, testicular shrinkage, and hair loss.
In the later stages, the above symptoms are accompanied by pain in the joints, dry skin and mucous membranes, and itchy blisters all over the body.
Alcoholic hepatitis
Alcoholic hepatitis is a consequence of regular consumption of alcohol in large quantities. Acetaldehyde, concentrating in the liver, causes cell hypoxia and their subsequent death.
Toxic damage leads to an inflammatory process. When alcoholic hepatitis is combined with the hepatitis C virus, the clinical picture is more pronounced and severe.
Pathology has the following types of course:
| Latent | There are no specific symptoms, the man feels a constant heaviness in his side, weakness, and slight nausea. |
| Jaundice form | Most common. Characteristic manifestations: loss of strength, weight loss, pain in the right hypochondrium, vomiting, abnormal bowel movements, yellowing of the skin and sclera. If ascites develops and the palms become red (palmar erythema), this indicates the onset of cirrhosis. |
| Cholestatic form | It is expressed in darkening of urine, whitening of feces, skin itching, and severe jaundice. |
The final stages of alcoholic hepatitis are liver cirrhosis and hepatocarcinoma.
Hepatitis C
Viral hepatitis is an infectious disease caused by a group of hepatotropic viruses (reproducing mainly in liver cells - hepatocytes). Currently, the most widely studied viral hepatitis are A, B, C, D (delta) and E.
The special position of viral hepatitis C (HC) among other hepatitis is due to the catastrophic increase in infection with the HC virus in the population and especially young people, which is associated with the growth of syringe drug addiction. Thus, according to the World Health Organization, approximately 1 billion people on the planet are infected with the HS virus. It is quite clear that at such a rate the absolute number of unfavorable outcomes is increasing.
Another feature of the HS problem is that viral hepatitis C has not been sufficiently studied both from the standpoint of virus and immunogenesis, and from a purely clinical point of view. It is with HS that paradoxical situations are observed when a diagnosis of chronic hepatitis is made, but there are no clinical, anamnestic, and sometimes laboratory data (except for the detection of antibodies to HCV (Hepatitis C Virus) alone).
It is necessary to immediately determine that HS should be considered as one of the components of the global problem of HCV infection, which includes not only acute and chronic hepatitis itself, but also liver cirrhosis and extrahepatic lesions. It is this approach that will help to correctly determine the condition of a particular patient and evaluate laboratory data, foresee the prospects for the development of infection, individually and timely select the necessary adequate therapy and avoid categorical, hasty predictions regarding the fatality of acute and chronic HS.
Clinical forms of hepatitis C
When the HS virus enters the human body, two variants of the infectious process may develop:
- the manifest form of HCV infection is acute hepatitis in an icteric or anicteric form, but always with symptoms of hepatitis (intoxication, asthenodyspeptic syndrome, enlarged liver and spleen, etc.);
- asymptomatic (subclinical) form of HCV infection, when there are no complaints or symptoms of hepatitis.
Acute manifest forms of HCV infection (icteric and anicteric) occur as acute HS with varying degrees of disease severity (mild, moderate, severe and malignant). In some cases, a protracted course is observed: with prolonged hyperfermentemia and/or with prolonged jaundice (cholestatic variant).
Subsequently, the disease ends:
- recovery (15–25%);
- the formation of a chronic infection that occurs like chronic hepatitis with varying degrees of activity.
The asymptomatic (subclinical) form of HCV infection is the most common (up to 70% of all cases of infection), but is practically not diagnosed during the acute phase. Subsequently, subclinical forms (as well as acute manifest ones) end with recovery or the formation of chronic hepatitis with varying degrees of activity. It should be emphasized that the course of the asymptomatic form of HS (as well as manifest forms) is accompanied by qualitative and quantitative changes in specific (IgM and IgG) antibodies, as well as certain dynamics of viremia, studied by the level of HCV RNA in the blood. At the same time, changes in the biochemical parameters of hepatocyte cytolysis (hyperenzyme of alanine (ALT) and aspartic (AST) aminotransferases, etc.) are observed, varying in severity.
Acute icteric form . The incubation period varies from several weeks (with blood transfusion and its preparations) to 3–6 and rarely up to 12 months (with infection through parenteral manipulations). The average incubation period is 6 months.
Pre-icteric period. The disease often begins gradually, manifesting itself mainly as astheno-dyspeptic syndrome. Patients complain of general weakness, decreased performance, malaise, increased fatigue, loss of appetite, possible nausea, vomiting 1–2 times, a feeling of heaviness in the epigastrium, and sometimes aching pain in the right hypochondrium. An increase in body temperature is not a permanent symptom - only 1/3 of patients with HS in the pre-icteric period show an increase in body temperature, mainly within the subfebrile range. In the same period, you can palpate an enlarged, often painful liver. The duration of the initial (pre-icteric) period ranges from 4 to 7 days, but in some patients it can reach 3 weeks. At the end of the pre-icteric period, the color of urine and the color of stool changes.
Jaundice period. With the appearance of jaundice, symptoms of liver intoxication may persist, but more often they decrease or completely disappear. During this period, lethargy, weakness, decreased appetite up to anorexia, nausea, rarely vomiting, pain in the epigastrium and right hypochondrium are characteristic. In all patients, hepatomegaly is detected, sometimes the edge of the liver is sensitive to palpation, and in some patients (up to 30%), an enlarged spleen is detected. The severity of jaundice varies: from weak icterus of the sclera to high intensity coloring of the skin.
One of the features of HS is a rather short, compared to other types of hepatitis, period of maximum severity of symptoms of intoxication and jaundice. In the blood serum there is an increase in bilirubin content and a significant increase in the activity of ALT and AST. The thymol test indicators moderately increase, and the sublimate titer decreases. The icteric period lasts from 1 to 3 weeks. Some patients may develop a cholestatic variant of the disease with a duration of jaundice of up to two to three months, itching of the skin (sometimes debilitating) and with biochemical changes in the blood typical for long-term hyperbilirubinemia (high levels of total and conjugated bilirubin, increased alkaline phosphatase levels).
The period of decline of jaundice is characterized by normalization of the patient’s well-being, a decrease in the size of the liver and spleen, a gradual restoration of the color of urine and stool, and a significant decrease in enzyme activity and bilirubin levels.
Outcomes of acute hepatitis C. Recovery is observed in 15–25% of all cases of acute hepatitis, and in the rest there is a transition to chronic hepatitis, with the gradual (over many years) formation of liver cirrhosis and, extremely rarely, with the development of primary liver cancer - hepatocellular carcinoma.
In most cases, the disease progresses slowly. About 15% of people infected with the HS virus recover spontaneously (i.e., after hepatitis, no hepatitis C virus RNA is detected in the blood for two years); in 25%, the disease is asymptomatic with normal levels of serum aminotransferases or with mild liver damage, i.e., on average, 40% of patients recover clinically. Naturally, with adequate therapy, the percentage of favorable outcomes increases.
Of course, factors such as alcohol abuse, drug addiction, substance abuse and poor nutrition largely accelerate and intensify the process of damage to the liver parenchyma, which in turn determines the unfavorable outcome of both acute and chronic HCV infection.
The risk group for developing viral cirrhosis of the liver also includes patients suffering from chronic diseases: diabetes mellitus, tuberculosis, collagenosis, chronic diseases of the stomach, intestines, kidneys, etc.
In terms of prognosis, the development of HS along with hepatitis B is alarming: simultaneous infection (co-infection) or combination (superinfection): chronic hepatitis B with the addition of acute HS; chronic hepatitis B and hepatitis B virus (HBV) infection.
In this regard, the tactics and strategy for treating such patients require a differentiated, individual approach in each specific case.
Chronic hepatitis C. With HCV infection, more often than with HBV (Hepatitis B Virus), the disease becomes chronic.
Clinical manifestations of chronic hepatitis C (CHC), which develops after an icteric form or after an asymptomatic course of the disease, are very insignificant and are manifested by some astheno-vegetative symptoms: increased fatigue, unmotivated weakness, bad mood, and sometimes loss of appetite. Often the severity of symptoms and complaints is so low that only after a thorough and even biased examination of the anamnesis is it possible to build a chronology of the disease. Dyspeptic syndrome is also mild or absent - there is a slight decrease in appetite, nausea is possible after fatty, spicy foods, and sometimes there is a disturbing feeling of heaviness in the right hypochondrium. Patients usually associate these symptoms with a violation of nutrition and diet. On examination, an enlarged liver is determined (the liver is 1–1.5 cm below the costal edge with a moderately elastic, smooth, sharp, sensitive or painless edge); in 30–40% of patients the spleen is palpated. Ultrasound reveals hepatosplenomegaly and diffuse changes in the parenchyma of the liver and spleen. Transaminase activity is usually within normal values or 1.5–3 times higher than them. No disruption of protein metabolism is observed. During a serological study, antibodies to HCV of the general pool are recorded, while the RNA of the virus is determined in the blood.
In chronic HS with high process activity, the course of the disease is wavy and consists of periods of exacerbation and remission. The period of exacerbation is characterized by polymorphism of the clinical picture, but the leading one is astheno-dyspeptic syndrome; jaundice is observed in 10–25% of patients. Sharp changes in laboratory parameters are noted: transaminase activity exceeds normal values by 10 or more times, and indicators of protein and lipid metabolism change. HCV RNA is detected in the blood. Ultrasound reveals hepatosplenomegaly, depleted vascular pattern, echogenic heterogeneity of the parenchyma (granularity) and thickening of the liver capsule.
During the period of remission of chronic HS, the well-being of patients improves, enzyme activity decreases, but hepatomegaly persists, while splenomegaly is recorded in 10–15% of patients. In some cases, viremia may disappear (with the subsequent appearance of viral RNA during the next exacerbation).
The frequency of periods of exacerbations and remissions and the degree of their severity are quite variable, but a certain pattern exists: the more frequent the exacerbations, the longer they are and the higher the activity of ALT and AST, which contributes to the more rapid formation of liver cirrhosis. It is with high activity of CHC that extrahepatic manifestations such as arthralgia, low-grade fever, telangiectasias, skin rashes, etc. are observed, as well as symptoms of decompensated intestinal dysbiosis (milder forms of dysbiosis - compensated or latent and subcompensated are observed in almost any clinical form of HS ).
Repeated exacerbations of CHC, occurring with a high degree of activity, ultimately end in the transition to the next clinical form of HCV infection - viral cirrhosis of the liver, the symptoms of which are well known. However, this usually takes many years.
It should be separately emphasized that in chronic active HS, extrahepatic manifestations are associated with the development of autoimmune (immunopathological) processes, in the initiation of which the HCV infection virus plays a certain role. Progressive autoimmune pathology (polyarthritis, Sjögren's syndrome, polyneuritis, nephropathy, anemia, etc.) in turn aggravates the course of chronic liver damage, which determines the need to select adequate therapy.
Morphological characteristics . Most patients with chronic infection have moderate or moderate severity of necrotic-inflammatory damage in the liver with a minimal level of fibrosis. The progression of HCV infection is accompanied by a portal and periportal inflammatory reaction with small focal necrosis and massive lymphocytic infiltration. The process of liver damage may intensify: as a result of necrotic changes, connective tissue septa are formed and multilobular (confluent, so-called “bridge-like”) necrosis develops, which characterizes chronic active hepatitis with initial signs of liver cirrhosis. The high activity of chronic HS is morphologically characterized by the progression of multilobular necrosis and the formation of multiple connective tissue septa, which in turn disrupts the blood supply and causes chaotic nodular regeneration in the remaining surviving islands of parenchymal cells, which contributes to the formation of “false” regenerative hepatic lobules resulting in macronodular cirrhosis.
Outcomes of chronic hepatitis C. The rate of transition of CHC to cirrhosis of the liver is different: only 10–20% of patients have pronounced activity of the inflammatory process and clinically manifest cirrhosis develops within 10–20 years, while the majority of patients with CHC simply do not live to develop manifest cirrhosis and, especially, liver cancer, dying from other (general somatic) diseases. However, in a number of cases, there is a rapid progression of CHC to cirrhosis of the liver, which depends on many factors, among which are alcohol abuse, toxic effects of drugs, concomitant somatic diseases, simultaneous infection with viruses C and B (co-infection) or HBV superinfection, initially inadequate specific therapy HCV infections. Therefore, knowledge of the chronology and features of the development of viral liver damage should be taken into account when choosing tactics and strategies for treating HCV infection, especially its chronic forms.
Diagnostics
Specific laboratory diagnosis of HCV infection is based on the detection of specific antibodies to the main antigens of the virus and determination of the RNA of the virus, its quantity and genotype.
Third-generation enzyme-linked immunosorbent test systems for determining antibodies to HCV, where immunoreactive synthetic peptides are used as a binding antigen on the solid phase, are quite sensitive and informative, and their widespread use has increased the percentage of detection of individuals infected with the HS virus.
The so-called definition is widely used. general antibodies to HCV, however, the interpretation of the positive results of such a study is very limited - the presence of general antibodies to HCV only allows us to state the fact of the patient’s contact with the HS virus and does not allow us to judge either the duration of the process, or its completion or progression. There is also no correlation with the severity of the clinical course of HCV infection.
Thus, the detection of only general antibodies to HCV has a screening (indicative) meaning and provides the basis for further comprehensive, including specific laboratory examination. Note that general antibodies to the hepatitis C virus remain in the body indefinitely.
Antibodies of the IgM class to HCV, determined by the enzyme immunoassay method, allow us to speak not only about infection with the HS virus, but with a certain degree of certainty about the acute phase of infection or exacerbation of chronic hepatitis, despite the absence of symptoms of the disease and hyperenzymemia of ALT, AST.
Viral RNA is detected in the cytoplasm of most liver hepatocytes already in the first or second week of infection. Subsequently, the number of viral particles may periodically increase, but this does not always correlate with the presence of RNA in the blood serum or with the degree of inflammatory changes in the liver. Maximum viremia is observed at the beginning of the acute period of the disease. Antibodies appear 6–12 weeks after the onset of hepatitis. First of all, antibodies are detected to structural (nuclear protein-associated) proteins, and then to non-structural proteins - NS3, NS4 and NS5 regions of the genome.
Determination of HS virus ribonucleic acid (HCV-RNA) is carried out using PCR, which with a high degree of accuracy shows the presence or absence of viral RNA in the blood.
The PCR method allows you to determine the viral genotype and its subtype, as well as the amount of RNA (titer or number of genocopies per ml). Determination of the genotype of the virus and its titer (semi-quantitative study) in the patient’s blood is used both for diagnosing HCV infection and for additional assessment of the activity of the viral process and for monitoring the effectiveness of complex, including antiviral treatment. The interpretation of the results obtained is assessed as follows: 1 + (1:1) and 2 + (1:10) - viral RNA is detected in a low titer, the level of viremia is low, 3 + (1:100) - an average level of viremia and finally 4 + ( 1:1000) and 5+ (1:10000) - high level of viremia. The disadvantage of the method is its technological complexity and currently quite high economic costs, which does not allow its widespread implementation in mass laboratory testing.
If the test result is positive for antibodies to HCV and there is no clinical picture of hepatitis, the simplest (and correct) decision would be to refer the patient to an infectious disease specialist. To obtain a more complete description, additional examination should be carried out:
- biochemical blood test (so-called liver tests - ALT, AST, GGTP (g-glutamyl transpeptidase), cholesterol, bilirubin, etc.);
- separate determination of antibodies to HCV;
- blood test for virus RNA (PCR) and if it is detected: determination of genotype and titer;
- An ultrasound examination of the abdominal organs is also desirable.
The results of such an examination, together with data from the epidemiological history and physical examination at the first stage, will help to develop the correct treatment tactics and management of a particular patient. There are often situations when the results of a comprehensive examination do not reveal any abnormalities other than the detection of antibodies to HCV. In these cases, it is reasonable to talk about a previously suffered subclinical form of HCV infection. However, given the existing likelihood of reactivation (replication) of the virus, the patient should be registered at a dispensary and random laboratory examinations should be carried out 2–4 times a year. Similar recommendations are given to a patient who has suffered a manifest form of HS.
Hepatitis C therapy
Treatment of hepatitis has a number of features and depends primarily on whether acute or chronic hepatitis is diagnosed in the patient.
Acute hepatitis C is a typical infectious disease and in its treatment traditional principles of treatment of viral hepatitis are applied: the nature of the treatment of manifest forms of viral hepatitis (occurring with symptoms of intoxication and jaundice) depends on the severity, however, in all forms, patients must follow a regimen with limited physical activity and diet - table No. 5, and in case of exacerbation of the process - No. 5a. Basic therapy also includes oral detoxification, the use of antispasmodics, enzyme preparations, vitamins, and desensitizing agents. Along with generally accepted basic therapy, in modern conditions it is possible to prescribe etiotropic treatment: the prescription of interferon inducers and immunomodulators (Amiksin, Neovir, Cycloferon, Immunofan, Polyoxidonium, etc.).
In moderate and even more severe forms of HS, accompanied by severe symptoms of intoxication (prolonged nausea, repeated vomiting, severe weakness, increased jaundice and other signs of liver failure), intravenous administration of glucose-electrolyte solutions, polyvinylpyrrolidone preparations (Hemodez and analogues) in a daily volume is indicated up to 1.5–2 liters under diuresis control. In cases of the development of a severe and malignant course, glucocorticoids are added to therapy (prednisolone 60–90 mg per os per day or 240–300 mg intravenously), protein preparations (albumin, plasma), amino acid mixtures (Hepasteril A and B, Aminosteril N-hepa etc.), antihemorrhagic agents (Vikasol, Dicynone, aminocaproic acid), protease inhibitors (Kontrikal, Gordox and analogues), enterosorbents, among which Duphalac is the most preferred. Plasmapheresis remains an effective method of treating severe forms.
When a cholestatic variant of the course develops, Usofalk (ursodeoxycholic acid) is prescribed at 8–10 mg/kg body per day once in the evening for 15–30 days, enterosorbents (Polifepam, Enterosgel, etc.). In some cases, a positive effect is observed during hyperbaric oxygenation (HBO), plasmapheresis sessions, and inhaled heparin in combination with laser therapy.
Other drugs can also be included in the pathogenetic therapy of GS: Heptral, Riboxin, Tykveol, Chofitol, Phosphogliv, Karsil, Legalon and analogues. Recently, the drug “Glutoxim” has been used, which selectively acts on virus-infected and unaffected cells and regulates the processes of thiol metabolism.
Considering the fact that in liver pathology there are always disturbances of the intestinal microflora of varying severity, it is recommended to prescribe bacterial preparations that normalize the intestinal microflora - Bifidumbacterin and its combinations, Lactobacterin, Hillak-forte, etc. It is rational to use the complex synbiotic Bifistim, which contains, in addition to bacteria, a multivitamin complex and dietary fiber, the need for inclusion of which was mentioned earlier.
Currently, there is no consensus on the advisability of using antiviral drugs of the interferon group (or other groups) in the treatment of acute HS. There are a number of studies demonstrating the effectiveness of prescribing a 3-month course of interferons (or a combination of interferons with nucleosides) in patients with acute hepatitis. According to the authors, early administration of antiviral drugs significantly reduces the frequency of transition of acute hepatitis to protracted and chronic.
It also seems justified to prescribe drugs with antiviral activity (glycyrrhizic acid drugs - Viusid, Phosphogliv) in the initial period of acute HS.
Chronic hepatitis C. Therapy of patients with CHC includes a number of aspects, among which the deontological one should be highlighted first. Thus, patients with HS must be informed in detail on a certain range of issues related to their disease, in particular regarding the features of the clinical course, rules of behavior of the patient in everyday life, sanitary and epidemiological nature, possible outcomes with an emphasis on a high percentage of chronicity, the use of therapeutic measures and means, including specific antiviral drugs and the associated difficulties and problems (duration and high cost of therapy, unwanted side effects, expected effectiveness of treatment). The result of such an interview between the doctor and the patient should be the patient’s conscious desire to be treated, as well as an optimistic attitude towards the upcoming long and persistent therapy.
Currently, a number of medications are used in world practice, the antiviral activity of which has been proven to one degree or another.
The first and main group of antiviral drugs consists of a-interferons (recombinant and natural) - such as: Reaferon, Roferon-A, Intron-A, Interal, Wellferon, Realdiron, etc. It is believed that their antiviral effect is based on inhibition of viral reproduction and stimulation many factors of the body's immune system.
The second group of antiviral agents consists of reverse transcriptase inhibitors and, in particular, nucleoside analogues (Ribavirin, Ribamidil, Rebetol, Ribavirin-vera, Vidarabine, Lobucavir, Sorivudine, etc.), blocking the synthesis of viral DNA and RNA by replacing natural nucleosides and thereby inhibiting viral replication. Remantadine and Amantadine also have an antiviral effect.
The third series of drugs is represented by interferonogens (Amiksin, Cycloferon, Neovir, etc.), the mechanism of action of which is to induce the macroorganism to produce additional amounts of its own interferons.
Treatment of any disease and especially the chronic form of HS requires an exclusively individual approach, since the nature of the pathological process in each individual patient is determined by a number of important components, such as: the patient’s age, the nature of the concomitant pathology, the duration of the disease, the genotype of the virus and the level of viral load, tolerance drugs, the presence and severity of side effects associated with the therapy and, in the end (and in some cases at the beginning), with the economic capabilities of a particular patient.
It is appropriate to note that monotherapy with interferon drugs, initially used in patients with CHC according to the literature (1999–2000) - Intron-A 3 million IU 3 times a week or Wellferon in the same regimen for 12 months, gave a positive result from 13 up to 48% (meaning normalization of aminotransferase levels and disappearance of HCV RNA in the blood according to PCR data). The results depended on the genotype of the pathogen and included the so-called. positive unstable responses, i.e., the new appearance of RNA in the blood of patients during a 6-12 month follow-up after completion of treatment.
In order to increase the effectiveness of treatment of chronic viral hepatitis, complex antiviral therapy has recently been used, usually the combined use of a-interferons with nucleoside analogues. For example, the combined use of Intron-A 3 million IU 3 times a week with Ribavirin analogues (Ribamidil, Rebetol, Vidarabine, Lobucavir, Sorivudine, etc.), daily at a dose of 1000–1200 mg for 12 months, allowed us to obtain a stable, sustainable response in 43% of patients, i.e. the absence of HS virus RNA in the blood according to PCR data over the course of 12 months of observation of patients after cessation of such therapy. However, it should be taken into account that nucleoside analogues themselves have a whole range of adverse reactions, which appear more often with long-term use of the drugs. The patient should also be warned about these nucleoside reactions.
Among other factors, the insufficiently high positive stable effect of even combination therapy was explained by the fact that the interferon therapy regimens used did not create a constant therapeutic concentration of the active substance in the blood and tissues, since the half-life of interferon introduced into the body is 8 hours, while the virus only needs the intervals between interferon injections are only a few hours to reach its original concentration again. Replacing the drug Intron-A in the above treatment regimen for patients with CHC with PEG-interferon (PEG-intron, Pegasys) at a dose of 180 mcg in the form of 1 injection per week (the addition of polyethylene glycol to the interferon molecule leads to an extension of the half-life of the active substance in the body to 168 hours) ultimately made it possible to obtain a stable therapeutic response in an average of 72% of all patients treated in this way, of which 94% with pathogen genotypes 2 and 3.
There are reports that such complex therapy, undertaken for 6 months in patients with acute viral hepatitis C, provided a complete cure and eliminated chronicity of the process in almost all patients (98%), regardless of the genotype of the pathogen. The same impressive data were obtained in the treatment of CHC. It should be added that the optimistic results obtained with the use of PEG-interferon are overshadowed by the unacceptably high price of the drug.
Treatment of HS is a rather complex undertaking, therefore, when prescribing and conducting specific therapy, it is appropriate to be guided by the following principles:
- it is necessary to detect the RNA of the virus in the blood using PCR data, determine its genotype and the level of viremia (by a quantitative or semi-quantitative method);
- conduct a comprehensive laboratory examination (peripheral blood test, biochemical blood test);
- assess the nature of the patient’s concomitant pathology (for example, renal with impaired excretory function, cardiovascular, autoimmune diseases, thyroid diseases, severe abnormalities in the peripheral blood, in particular anemia, thrombocytopenia, leukopenia), which may even be a contraindication for the planned antiviral treatment. Specific therapy is prohibited during pregnancy;
- Both acute (and even preferably!) and chronic forms of viral hepatitis are subject to treatment, including those when, in the presence of pathogen RNA in the blood, a consistently normal level of aminotransferases is recorded;
- the combined use of antiviral drugs is recommended;
- taking into account the possibility of developing tolerance to the medications used or the formation of antibodies to them, at certain stages of treatment it is advisable to change combinations of therapeutic agents from time to time;
- the effectiveness of treatment depends more on the duration of its implementation than on the dose of the drug (depending on the specific characteristics of the patient, the duration of treatment ranges from 6 to 18 months);
- monthly and, if necessary, more frequent monitoring of clinical and laboratory data, including a detailed analysis of peripheral blood, is required in order to correct possible side effects;
- the patient should be remembered and informed that during therapy, chills, fever, myalgia, allergic phenomena, anorexia, depression, thyroiditis, baldness, anemia, leukopenia, thrombocytopenia, agranulocytosis are possible.
A priori, one should expect a lower effectiveness of treatment with HS, and sometimes its complete absence in the following cases: in persons with immunosuppression of various origins, in patients with obesity, with a combined chronic process caused by hepatitis C and B viruses, in patients with genotype 1b virus, with high concentration of HCV-RNA in the blood, with a long duration of the chronic process (many years), in the presence of autoimmune diseases, in cases where treatment occurs while taking narcotic drugs, and also when treatment is carried out in only one of the two patients with HS, sexually transmitted diseases partners (possibility of reinfection with a virus of the same genotype).
The situation is complicated by the exceptionally high cost of treatment for the patient, since both domestic and foreign antiviral drugs used in Russia are not yet included in the register of medications provided free of charge.
S. N. Zharov , Doctor of Medical Sciences, Professor B. I. Sanin , Candidate of Medical Sciences, Associate Professor V. I. Luchshev , Doctor of Medical Sciences, Professor of the State Educational Institution of Higher Professional Education of the Russian State Medical University of Roszdrav , Moscow
Transmission routes
Be careful with personal hygiene products as they may contain blood particles
The main route of transmission of infection is parenteral, that is, through the blood. Microbes have low resistance to the external environment and die at a temperature of +50 degrees and from exposure to ultraviolet radiation.
The source of infection is a sick or infected person. Almost 70% of cases of infection are associated with intravenous drug use if non-sterile syringes are used.
The infection can also be introduced into the blood in a tattoo parlor, during cosmetic procedures, or in dentistry. In other words, all manipulations associated with human blood are dangerous.
Sexual transmission is very rare, since semen, saliva, and urine contain very low concentrations of viruses. It is almost impossible to become infected through everyday contact (through a utensil or a handshake).
Transmission of the virus from mother to child is possible if the woman is diagnosed with an acute period of the disease or the child suffers from immunodeficiency.
The human body is susceptible to only a large number of microbes. When isolated microorganisms enter the bloodstream, they are destroyed by the immune system.
Hepatitis C is most widespread among drug addicts and patients with immunodeficiency. Very often it is not possible to trace the route of transmission of infection.
Watch a video about the modes of transmission of hepatitis:
How to protect yourself
The long incubation period is a serious problem for the infected person. This prevents the rapid identification of the source of the disease and the initiation of timely therapy. To protect yourself at least a little from the virus, you should strictly follow a number of recommendations given by experts:
- It is unacceptable to use other people's items. They may contain some of the blood of infected people.
- We check the sterility of equipment in a hairdressing salon.
- If there is a need to use a syringe, preference should be given to a disposable injection instrument.
Following these recommendations will help you avoid the virus of such an insidious disease as hepatitis C.
Symptoms
From the moment it enters the bloodstream until the first symptoms appear, several days or months may pass. If a man is of strong build and has good immunity, then the virus will remain dormant for a long time.
In this case, the person will infect others. The development of the disease and the clinical picture depend on the body's resistance. It happens that men live with hepatitis C for 10 or 20 years without experiencing serious health problems. Almost 80% of cases of pathology become chronic.
The symptoms of the acute stage are similar to those of influenza or ARVI, and therefore remain unattended by men. In acute hepatitis, the following manifestations occur:
- Weakness.
- Fever.
- Fatigue.
- Headache.
- Decreased appetite.
- Sleep disturbance.
- Slight increase in temperature.
- Sweetish taste in the mouth.
- A slight decrease in platelets and leukocytes in the blood.
The severity of clinical manifestations depends on the patient’s immunity.
Watch a video about the symptoms of hepatitis C:
Why is hepatitis a disease of drug addicts?
People with drug addiction experience symptoms of the pathology more often than others. There are several reasons for this:
- they have lowered immunity;
- many of them suffer from HIV infection;
- periodically they use one needle for the entire group when administering drugs;
- they are promiscuous.
It also matters that drug addicts do not care about their health at all. After all, the virus can enter the body through wounds and damaged mucous membranes. Drug addicts do not pay enough attention to treating cuts, ulcers, and abrasions.
If the disease is started, it gradually becomes chronic. This is very dangerous as liver cancer may develop. It must be taken into account that drug addicts tolerate the disease worse, since they have reduced immunity. Many of them do not begin treatment, even if they learn about a terrible diagnosis.
It is difficult for addicts to recover from hepatitis C because their liver functions poorly. Organ cells - hepatocytes - are subject to a serious toxic attack from surfactant metabolites. Many of them are completely destroyed. Under such conditions, necrosis of individual tissues often develops. If the virus attacks a diseased liver, it is very difficult to recover.
Signs of severe disease
Severe form of hepatitis C occurs no more often than 2% of cases. It is usually observed in people with immunodeficiency, chronic alcoholism, or concurrent infection with hepatitis B and or HIV.
This form of infection is called fulminant. With it, hepatocytes rapidly die and acute liver failure develops. Mortality reaches 70%.
Signs of a severe course are:
- severe fatigue in the evening;
- a sharp decrease in performance;
- development of jaundice;
- skin itching;
- darkening of urine;
- enlarged liver and spleen;
- weight loss.
These symptoms in men are accompanied by pain in the right side, signs of intoxication, encephalopathy, and bleeding. Often patients suddenly fall into a hepatic coma. The survival rate is no more than 15%.
How should relatives behave if they live with an infected drug addict?
If there is a drug addict in the house, it is important to follow basic safety rules. The virus easily tolerates temperatures of 50-60°C, so dishes and bed linen must be treated with boiling water and disinfected.
Under no circumstances should you share a toothbrush, razor, or manicure accessories with a contaminated one. You should also not smoke the same cigarette with him. It is advisable that the infected person have his own cutlery.
Danger
Hepatitis C got its name because the disease develops asymptomatically for a long time.
Hepatitis C is not called “the gentle killer” for nothing. A long latent period gives way to acute manifestations of fatal complications that leave little chance of survival.
Complications of the disease are:
- Cirrhosis of the liver.
- Malignant organ tumor.
- Portal hypertension.
- Ascites.
- Hepatic encephalopathy.
- Involvement in the process of other organs of the gastrointestinal tract (pancreas, stomach, intestines).
- Liver failure.
- Peritonitis, sepsis.
- Coma.
Diagnostics
To make a diagnosis, the patient is prescribed the following types of studies:
- Serological test for antibodies to the virus. Performed using enzyme immunoassay.
- Isolation of pathogen RNA using polymerase chain reaction.
Changes in the liver are detected using additional examinations:
- Coagulograms. With hepatitis, blood clotting is reduced.
- Ultrasound of the liver. Detects changes in organ size, structure, and vascular condition.
- Liver biopsies. Prescribed for suspected cirrhosis or cancer.
Treatment of acute viral hepatitis
Today, interferon alpha is used in the world as the main antiviral agent for the treatment of viral hepatitis. When treated with interferons, the percentage of chronicity decreases approximately 5 times. In the complex therapy of chronic viral hepatitis B, various immunomodulators are used.
In addition to basic antiviral therapy, hepatoprotectors, for example based on essential phospholipids, are recommended to maintain liver function. They help restore the integrity of liver cells, promote their regeneration, and limit the formation of connective tissue in the liver.
Patients are advised to take a gentle regimen and diet. Fried, smoked, pickled foods, and refractory fats are excluded from the diet. Alcohol in any form is strictly prohibited.
Innovations in treatment
Generics are a worthy replacement for expensive drugs from the USA
Until recently, treatment for infection was carried out using interferon drugs and antiviral drugs. These methods initially give positive results; no viruses are detected in the patients’ blood.
However, the RNA of the virus is stored in liver cells. This means that the disease will begin to develop again at any moment. In addition, microorganisms are able to adapt and develop resistance to drug components.
The disease is now considered curable. New agents have been invented that act at the cellular level. Their components are integrated into the DNA of the virus and destroy it.
Such drugs are Sofosbuvir, Sovaldi and Daclatasvir. Positive dynamics are observed even in the case of carriage of a highly resistant mutated genotype.
The optimal therapy is a combination of Sofosbuvir and Daclatasvir. The disadvantage of this treatment is its high cost. For example, two standards of funds cost about 50 thousand rubles.
Chinese, Indian and Egyptian generics have appeared on the pharmaceutical market. They are not inferior in their effect to the main product, but are several times cheaper. True, you won’t be able to purchase them in official pharmacies. The only way out is to order online.
Mechanism of disease development
Having entered the liver cells (hepatocytes) through the blood, the virus begins to multiply there. The immune system detects infected cells, destroys the virus, but the cell itself dies. At the initial stages of the disease, destroyed liver cells are replaced by new ones. The organ is constantly being restored, and with the hepatitis C virus, the restoration of hepatocytes occurs at an accelerated rate.
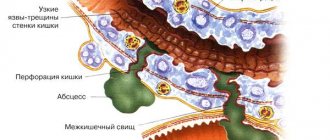
But if the virus is very active, if the liver cells are attacked by other infections, and the body is also affected by toxins - drugs, alcohol, medications - the liver cells do not have time to regenerate. Then scars begin to form in the organ: working liver cells are replaced by connective tissue. Fibrosis develops. The functioning of the organ is not yet impaired. However, if the process continues to develop actively, the connective tissue grows widely. The liver lobules begin to collapse. Severe processes associated with liver cirrhosis develop:
- scars block blood flow in the liver, blood seeks bypass routes through the esophagus and rectum, which can cause bleeding;
- toxins do not enter the liver and, accordingly, are not neutralized.
The liver cannot cope with its work, as there are few working cells, and liver failure develops. Swelling forms and blood clotting is impaired. The course of the disease is influenced by many factors. The following signs of infection have a bad effect on the development of chronic hepatitis:
- alcohol consumption;
- excess body weight – obesity;
- iron metabolism disorder;
- metabolic syndrome - impaired metabolism of fats and carbohydrates, persistent increase in blood pressure;
- re-infection;
- a man fell ill with hepatitis;
- At the time of infection, the patient was over forty years old.
With chronic alcoholism, hepatitis C in men progresses very actively to liver cirrhosis.
Prevention and prognosis
With adequate treatment, the disease can be overcome. The prognosis depends on the timeliness of therapy, the state of the patient’s immunity, the presence of immunodeficiency and the degree of liver damage. The least favorable prognosis is for patients with HIV and infection. The mortality rate from cancer or cirrhosis is 5%.
Since there is no vaccine against hepatitis C, prevention consists of avoiding situations that increase the risk of infection. This:
- use of disposable syringes;
- visiting medical institutions and beauty salons with a good reputation;
- avoiding contact with other people's blood.
The state also carries out prevention in the form of educational work among the population and monitoring compliance with sanitary standards.
Preventive measures
Hepatitis C poses a large-scale social threat. Delayed diagnosis, negligent attitude to treatment, ignoring primary and secondary signs, addictions - a potential patient puts many lives in danger, including his own. To minimize the risk of infection, you should follow simple rules:
- Maintaining personal hygiene;
- Practice only protected sexual intercourse;
- Avoid visiting questionable medical institutions;
- Regularly take general and biochemical blood tests for the purpose of early detection of the disease.
In the IMMA network of medical clinics, each person can undergo an examination to determine markers of hepatitis C. A preventive examination is the key to timely diagnosis and successful treatment. It should be remembered that most cases of the disease are detected randomly. Postponing an important check for an indefinite period of time means putting your health and that of many people around you at risk.
Author of the material: general practitioner, gastroenterologist at the clinic on Nikulinskaya Nichman E. G.