Chronic viral hepatitis is a group of infections caused by viruses that affect liver cells.1 Under the influence of the virus, liver cells are damaged, inflammation begins in the organ, that is, hepatitis itself, which can manifest itself both in the form of emerging complaints and symptoms, and in form of pathological abnormalities in laboratory parameters. It is important to understand that these manifestations are only a consequence of cell damage and death, as well as the inflammatory process occurring in the organ. Chronic hepatitis is called if the inflammatory process continues for more than six months.2
Causes of chronic viral hepatitis
The disease is caused by hepatitis B, C and D (delta) viruses - the hepatitis A virus, as a rule, provokes an acute form of the disease. The most common cause of chronic hepatitis is the hepatitis C virus; it is found in 77.97% of cases of newly diagnosed chronic hepatitis in Russia. Every year, it infects about 50 thousand people throughout the country.3 The next most common is the hepatitis B virus. According to WHO, at least 257 million people worldwide are sick with it.4 In Russia, the incidence averages 10.78 people per 100 thousand ,5 but varies greatly by region. Hepatitis D can only accompany and aggravate hepatitis B, since it is not self-sufficient in terms of reproduction.
Invading liver cells, hepatitis B and C viruses leave particles of their antigens on the surface of the membranes. The immune system begins to view infected hepatocytes as foreign cells and attacks them. If the immune response is adequate, such an attack, although accompanied by symptoms of liver damage (clinical manifestations of acute viral hepatitis), quite quickly destroys infected cells. But the immune system cannot cope with the virus itself, and its activity is not enough to completely eliminate the infectious agent, as a result of which chronic hepatitis develops.
The liver has enormous regeneration capabilities, but since in chronic hepatitis the inflammatory process can last for years and decades, sooner or later the organ’s reserves may be depleted. In this case, connective (fibrous, scar) tissue is formed in place of the dead cells. It is not able to perform the functions of hepatocytes, and fibrotic degeneration of the liver can result in the development of liver failure. Another long-term, but very dangerous outcome of chronic hepatitis is the degeneration of hepatocytes and the formation of hepatocellular carcinoma (liver cancer).
If the infection occurs in adulthood, and the activity of the inflammatory process is low, chronic viral hepatitis can last for several decades. In this case, there is a possibility that the patient will die from causes unrelated to chronic hepatitis. If the infection entered the body in youth, and the inflammatory process is active, the likelihood of unfavorable developments is much higher. According to WHO, 720 thousand people die annually from liver cirrhosis due to viral hepatitis and 420 thousand die from hepatocellular carcinoma.4 Chronic hepatitis B with the delta agent (combined infection B and D) develops especially quickly and unfavorably.6
Classification of hepatitis
Chronic viral hepatitis is classified according to its causes and is divided into the following types:
- chronic viral hepatitis B;
- chronic viral hepatitis C;
- chronic viral hepatitis B with delta agent.
According to the degree of activity of the pathological process, the following types of chronic hepatitis are distinguished:
- with minimal activity;
- with moderate activity;
- with pronounced activity.
In addition, there are four stages of development of liver fibrosis - from mildly expressed to entailing a violation of the architectonics (characteristic structure of tissues) of the organ. The higher the stage of fibrosis, the more pronounced the pathological changes.
Publications in the media
Chronic viral hepatitis (CVH) is a chronic infectious disease caused by hepatotropic viruses; are characterized by a clinical and morphological picture of diffuse liver inflammation (lasting more than 6 months) and a symptom complex of extrahepatic lesions.
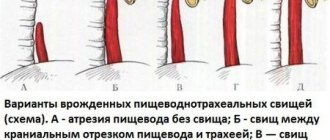
Etiology and epidemiology • CHV B (HBV infection). The causative agent is a DNA virus. The main route of transmission is parenteral, as well as through damaged mucous membranes and skin (perinatal, sexual contact, close household contact [shared razor, toothbrush, etc.]). At risk are drug addicts who inject drugs intravenously, homosexual men and persons in contact with blood and its products (for example, patients and medical personnel in surgery departments, hematology and hemodialysis centers). The incubation period is 1–6 months. Approximately 10% of patients experience a chronic course or long-term carriage of • CHV C (HCV infection). Previously, this hepatitis was designated by the term non-A non-B hepatitis, transmitted by the parenteral route. The causative agent is an RNA virus (HCV); isolated in 50–90% of cases of post-transfusion hepatitis. The routes of transmission (parenteral, sexual and possibly perinatal) are similar to those for chronic hepatitis B. The incubation period is from 2 weeks to 6 months. The chronic variant is observed in 30–50% and even 75% of patients (approximately 50% suffer from chronic active hepatitis); a significant proportion of patients develop cirrhosis of the liver • CHV D (HDV infection). The causative agent is a small defective RNA virus (HDV), d-virus); it is contagious only when infected with HBV (since, due to the incomplete genome, it uses HBV proteins for replication). The main route of transmission is parenteral (therapeutic and diagnostic procedures), as well as sexual and perinatal. The epidemiological significance of d-infection is great in regions where anti-d and HBS-Ag carriage is endemic. d-Infection exists in the form of acute infection with simultaneous infection with HBV and d-virus (co-infection) and acute infection with d-virus infection of HBV carriers or patients with chronic hepatitis B (superinfection). CVH D is characterized by a chronic, severe course • CVH E. The causative agent is an RNA virus isolated from patients with acute hepatitis in Mexico, Asia and Africa; outbreaks are observed in the CIS. The main mechanism of transmission is fecal-oral, the leading factor of transmission is infected water. People aged 15–40 years are affected. The incubation period is 15–45 days (average 40 days). The fulminant (fulminant) form of hepatitis is often registered in the 2nd–3rd trimester of pregnancy. Mortality among pregnant women can reach 10–20% • CHV G is classified as hepatitis transmitted parenterally; The disease is transmitted after a blood transfusion or organ transplant; the majority of those affected are adults. Giant multinucleated cells (syncytial giant cell hepatitis) are found in the liver. The virus was not isolated from liver biopsies; clinical and laboratory symptoms were not expressed. Hepatitis G is currently classified as non-A, non-B, non-C hepatitis.
Risk groups • Medical workers • Drug addicts • Recipients of blood and blood products (including patients with cancer and immunodeficiency conditions) • Newborns from mothers infected with HBV and HCV • Family members of persons infected with HBV and HCV • Patients on hemodialysis .
Clinical picture
• Signs of liver damage •• Active process - the liver is enlarged, dense, the edge is pointed, palpation is painful. With a decrease in activity, the size of the liver decreases, palpation is less painful (the consistency does not change significantly). Hepatomegaly is absent in patients with cirrhosis of the liver •• Pain in the liver area (the symptom is not constant, if present, the pain is constant, aching, sometimes intense, intensifies after physical activity) with an active process, with the subsidence of inflammatory phenomena - a decrease in the intensity of the pain syndrome •• Jaundice (parenchymal and secondary mechanical) is often accompanied by itchy skin, and scratches are found on the skin. Often CVH occurs without jaundice •• Telangiectasia and palmar erythema are caused by an increase in the concentration of estrogen and a change in the sensitivity of vascular receptors (opening and expansion of arteriovenous shunts). Their severity correlates with the activity of the process and does not indicate cirrhosis of the liver. Improvement in the functional state of the liver is accompanied by a decrease in the number of spider veins or their disappearance, hyperemia of the palms remains much longer (often until biochemical remission) •• Splenomegaly - with cirrhosis of the liver •• Dyspeptic syndrome (impaired detoxification function of the liver, concomitant pathology of the duodenum and pancreas ): nausea, worse after eating and taking drugs, vomiting, bitterness in the mouth, belching, diarrhea. Also, regardless of food intake, a feeling of heaviness and fullness in the right hypochondrium and epigastric regions is observed •• Asthenic syndrome: weakness, fatigue, decreased performance, irritability, decreased mood •• Amenorrhea, gynecomastia, decreased libido, associated with impaired metabolism of sex hormones in the liver •• Varnished tongue •• Minor liver failure syndrome: drowsiness, thrombohemorrhagic syndrome (bleeding and bruising on the skin, bleeding gums, nosebleeds, hematuria, uterine bleeding, etc.), transient jaundice and ascites; the syndrome is characteristic of an active inflammatory process in the liver •• Loss of body weight •• Increase in body temperature to subfebrile values.
• Extrahepatic manifestations •• Arthritis, arthralgia, polymyalgia •• Periarteritis nodosa •• Carditis •• Lung lesions: fibrosing alveolitis, pulmonary vasculitis, granulomatosis •• Pancreatitis •• Sjogren's syndrome •• Kidney damage: glomerulonephritis •• Skin lesions: late cutaneous porphyria, papular acrodermatitis (Gianotti-Crosti syndrome) •• Lesions of the endocrine system: autoimmune thyroiditis, ovarian dysfunction •• Raynaud's syndrome •• Damage to the nervous system: polyneuropathy, Guillain-Barre syndrome •• Secondary mixed cryoglobulinemia •• Hypoplastic or aplastic anemia.
Laboratory research. Biochemical blood test: increased ESR, hyperproteinemia, dysproteinemia (increased g-globulin content, increased thymol test, decreased blood albumin, decreased mercuric test), increased ALT and AST activity, increased conjugated (direct) bilirubin.
Serological studies
• Determination of CVH markers with the establishment of virus replication activity (in ELISA reactions, DNA hybridization, PCR). • HBV infection •• HBs-Ag (surface (Australian) HBV Ag) marks infection with the virus; appears in the blood 1.5 months after infection •• Ag Pre-S region HBs (Pre-S1 and Pre-S2) appear simultaneously or slightly earlier than HBsAg; mark an actively ongoing infection •• HBc-Ag (nuclear c-Ag) marks the replication of the virus in hepatocytes; discovered only during morphological examination of biopsy specimens or autopsy material of the liver; is not detected in free form in the blood •• HBe-Ag nuclear e-Ag (secretory part of HBc-Ag) indicates virus replication in hepatocytes; appears in serum almost simultaneously with HBs-Ag; may be absent in case of HBV infection caused by a mutant strain of the virus •• Anti-HBc (AT to nuclear Ag) is an important diagnostic marker of infection, especially with negative results of HBs-Ag indication •• Anti-HBc IgM (AT-immunoglobulins of class M to nuclear Ag ) is one of the earliest serum markers of chronic hepatitis B; the most sensitive marker of HBV infection; marks the replication of the virus and the activity of the process in the liver; its disappearance serves as an indicator of either the sanitation of the body from the pathogen, or the development of the integrative phase of HBV infection •• Anti-HBc IgG (AT-immunoglobulins of class G to nuclear Ag) persist for many years; indicate an existing or previously suffered infection •• Anti-HBe (AT to e-Ag) is a serological marker of virus integration; in combination with anti-HBc IgG and anti-HBs indicate the complete completion of the infectious process •• Anti-HBs (protective antibodies to surface Ag) indicate protection against infection; are formed during the vaccination process; may indicate the completion of a viral infection •• Anti-Pre-S (ATs to Pre-S1Ag and Pre-S2Ag) indicate the development of protective immunity at the completion of the infectious process; anti-PreS1 is registered simultaneously with anti-HBc, and anti-PreS2 - in the period of convalescence (evidence of recovery) •• HBV-DNA (HBV DNA) and DNA polymerase are diagnostic markers of virus replication •• HBV replication markers - HBe-Ag, anti-HBeAg IgM, HBV-DNA, HBV-DNA polymerase.
• HCV infection •• Anti-HCV (Ab to hepatitis C virus) appear in the blood within 6 months after infection (on average 3 months); indicate possible infection with the virus or a previous infection •• HCV RNA (HCV RNA) is a diagnostic marker of virus replication •• Markers of HCV replication are anti-HCV IgM and HCV RNA.
• HDV infection •• HDV-Ag (HDV Ag) - appears in the blood 3 weeks after infection; marks viral replication •• Anti-HDV IgM (class M antibody to hepatitis D virus) is considered a more reliable marker of HDV infection than HDV-Ag; indicate viral replication; recorded with high frequency during HDV superinfection as the most common cause of CHV D •• HDV-RNA (HDV RNA) is a diagnostic marker of virus replication •• Markers of HDV replication are anti-HDV IgM, HDV RNA.
Special methods • Ultrasound of the liver and spleen: increased echogenicity of the parenchyma, compaction along the liver vessels, with cirrhosis of the liver - splenomegaly • Radioisotope study of the liver: significant increase in cardioportal time (the time between peaks of activity above the heart and above the liver), enlarged liver, uneven accumulation of radiopharmaceuticals along the edges (fuzzy contours) • Laparoscopy: large compacted white or variegated liver with a pointed edge and a vague pattern of lobules, enhanced pattern of superficial vessels • Liver puncture biopsy: degeneration and necrosis of hepatocytes, lymphomacrophage infiltration and proliferation of connective tissue in the hepatic lobules. Changes are assessed using semi-quantitative methods (histological activity index according to RG Knodell et al and degree of fibrosis according to VJ Desmet et al.). Data from laparoscopy and liver puncture biopsy correlate with each other.
Differential diagnosis • Autoimmune hepatitis • Chronic drug-induced hepatitis • Primary biliary cirrhosis • Primary sclerosing cholangitis • Infectious mononucleosis • Primary and secondary liver tumors • Ischemic hepatitis • Chronic alcoholic hepatitis • Wilson's disease.
Treatment
• Etiotropic: IFN preparations (parenteral forms of natural and/or recombinant a- and b-IFN) - with a high degree of activity of the infectious process (presence of replication markers), as well as with extrahepatic lesions. The effectiveness of treatment is 20–60%.
• Criteria for the effectiveness of IFN treatment •• disappearance of HBV, HCV, HDV replication markers •• normalization of ALT and AST indicators •• improvement of the histological picture of the liver •• reduction or disappearance of symptoms of extrahepatic lesions.
• For chronic HBV infection, IFN is most effective in the presence of the following symptoms •• young age •• female gender •• onset of the disease in adulthood •• duration of the disease up to a year •• icteric form of the manifest manifestation of the disease •• high levels of ALT and AST in the serum blood •• low level of HBV-DNA (less than 200 pg/ml) •• absence of super- and coinfection with hepatitis C, D, G viruses, HIV infection, immunosuppressive therapy, renal failure, signs of cirrhosis.
• For chronic HCV infection, IFN is most effective in the presence of the following signs •• young age •• parenteral route of infection •• low concentration of HCV RNA •• HCV genotype 2a, 3, 4 (not 1b) •• normal iron content in the tissue liver and blood serum •• relatively short duration of the disease •• weakly expressed autoimmune component of inflammation •• absence of signs of cirrhosis, cholestasis.
• Chronic HDV infection is resistant to IFN therapy.
• Treatment regimens with IFN drugs •• For HBV infection ••• Recombinant a-IFN (interferon alpha-2b, for example, intron A) - 2.5–5 million (children up to 5–6 million) IU/m2 daily or 3 times/week subcutaneously or intramuscularly for 6 months ••• Natural a-IFN (interferon alpha-n1) 10 IU 3 times/week (for children - up to 10 IU/m2) for 12 weeks •• With HCV infections ••• Intron A 3 million IU/m2 3 times a week for 12–18 months ••• Interferon alpha-n1 3–5 IU 3 times a week for 48 weeks •• For HDV infection it is recommended intron A 5 million IU daily or 9–10 million IU 3 times a week for 12 months.
• Ways to increase the effectiveness of treatment with IFN drugs •• Combination with antiviral drugs with a different mechanism of action (for example, ribavirin) •• With low activity of the HBV replication process - preliminary treatment with prednisolone (for example, 30 mg / day for 3 weeks, then 15 mg/day for 1 week, then after 2 weeks treatment with IFN) •• For cholestasis, ursodeoxycholic acid is prescribed •• If the iron content in the liver tissue increases, bloodletting, antioxidants are prescribed.
Prevention • Prevention of the spread of infections transmitted parenterally (monitoring biological preparations for the presence of markers of viral replication, using disposable medical instruments, etc.).
Abbreviations • RFP - radiopharmaceutical • CHV - chronic viral hepatitis
ICD-10 • B18 Chronic viral hepatitis
Symptoms
Damage to liver cells inevitably leads to disruption of their functions. This can manifest itself in the form of several clinical and laboratory syndromes (combinations of symptoms).
Asthenovegetative syndrome:
- lethargy, increased fatigue, weakness;
- sleep disturbance (drowsiness during the day, insomnia at night);
- irritability.
Cytolysis syndrome is a complex of biochemical changes reflecting the destruction of liver cells. In the blood with this syndrome, the level of intracellular enzymes increases: AST, ALT, alkaline phosphatase, gamma-glutamyl transpeptidase (GGTP).
Dyspeptic syndrome:
- pain and heaviness in the right hypochondrium;
- nausea, vomiting;
- stomach ache;
- stool disorders.
Hepatosplenomegaly syndrome is an enlargement of the liver and spleen.
Jaundice syndrome is a yellow discoloration of the skin and mucous membranes. The intensity of its manifestation can vary - from a barely noticeable yellowness of the sclera (the white membrane of the eye) to a clear change in skin color. Jaundice is often accompanied by itchy skin. In addition, with the development of cirrhosis, other changes may appear: edema, abdominal enlargement due to the accumulation of fluid in the abdominal cavity (ascites), varicose veins of the anterior abdominal wall (with the appearance of the so-called head of the jellyfish), and a tendency to bleeding.
Diagnosis of chronic hepatitis
During the examination, the doctor may detect yellowness of the skin and mucous membranes, hepatomegaly, spider veins on the skin, xanthomas, xanthelasmas. If hepatitis is caused by alcohol abuse, characteristic changes in appearance occur: persistent redness of the face, jugular fossa area, and shoulder joints. Gynecomastia and atrophy of the muscles of the shoulder girdle are observed.
To clarify the diagnosis, the following may be recommended:
- Clinical blood test - reveals an increase in ESR;
- Blood chemistry. In the blood, the level of bilirubin, enzymes (alanine aminotransferase, aspartate aminotransferase, alkaline phosphatase, gammaglutamyl transpeptidase), ferritin, serum iron, cholesterol increases (a sharp decrease in cholesterol levels may indicate the development of liver failure and is considered an unfavorable prognostic sign);
- Analysis for hepatitis virus markers;
- Tests to detect antibodies to liver tissue antigens;
- Ultrasound of the liver;
- Biopsy of liver tissue (to determine the activity and stage of the process, as well as the severity of degenerative changes in the liver).
Diagnosis of the disease
Diagnosis of chronic viral hepatitis is based primarily on laboratory methods, since in the early stages the disease is often asymptomatic.
First of all, to confirm the cause of the disease, a blood test for specific markers of viral hepatitis is necessary. These are antigens of the hepatitis B or C virus (viral particles) and antibodies produced by the body in the fight against it. In addition to the qualitative determination (detection) of the antigen, it is also necessary to study the level of viral load (the amount of antigen in a certain volume of blood). This makes it possible to judge the activity of virus reproduction and determine indications for antiviral therapy.
To assess liver function, a biochemical blood test is recommended, which includes determining the level of liver enzymes, bilirubin, protein, protein fractions and other indicators. The doctor gives more specific recommendations based on the individual picture of the course of the disease.
To assess the size and structure of the organ, abdominal ultrasound is recommended: this is the simplest method of visualizing the liver.
To determine the degree of fibrosis, fibroelastography or liver biopsy can be performed - sampling a small amount of liver tissue under ultrasound guidance for further examination under a microscope.
Classification of hepatitis
By origin, chronic hepatitis can be:
- viral;
- toxic (this group includes drug and alcoholic hepatitis);
- metabolic (caused by genetic or metabolic disorders);
- autoimmune;
- idiopathic (the cause cannot be identified).
In addition, the clinical classification distinguishes several degrees of hepatitis activity (from minimal to severe) and several stages of fibrosis of the liver tissue (from absent to severe).
1.What is secondary hepatitis and its causes?
Hepatitis
, or inflammatory processes in the liver, differ significantly from each other in genesis (origin), type of course, severity, and prognosis. Thus, one of the criteria divides liver inflammation into primary and secondary. In primary hepatitis, the liver is the main target and the most affected organ - for example, due to a specific hepatic parasitic or viral infection.
Secondary hepatitis
called a hepatic inflammatory process that develops as a result of or against the background of another serious disease (which in this case is the main and chronologically earlier one). Hence the full name of secondary hepatitis: nonspecific reactive. Such a liver reaction is manifested not only by inflammation. Dystrophic and necrobiotic (preceding death, necrosis) irreversible changes begin in the cells of the liver parenchyma - working functional tissue - which in small foci is replaced by growing connective tissue.
Causes
Nonspecific reactive hepatitis can be caused by:
- irradiation;
- severe endocrine diseases (diabetes mellitus, hyperthyroidism);
- oncological diseases;
- diseases of the gastrointestinal tract (gastroduodenitis, colitis, etc.);
- chronic infections, helminthiasis;
- autoimmune diseases (systemic lupus erythematosus);
- chronic intoxication.
Sign up for a consultation
A must read! Help with treatment and hospitalization!
Prognosis and prevention
The prognosis for hepatitis is serious: chronic inflammation of the liver tissue sooner or later leads to the development of cirrhosis and significantly increases the likelihood of a malignant neoplasm. But a lot depends on the activity of the inflammatory process: the lower it is, the slower the adverse changes occur. With adequate treatment, the process can drag on for decades.
Prevention of viral hepatitis comes down to barrier contraception during sexual intercourse and compliance with hygiene rules. To protect against hepatitis B virus, you can get vaccinated. Toxic hepatitis can be avoided if you do not abuse medications and alcohol. There is no way to prevent autoimmune hepatitis.
Sources:
1https://emedicine.medscape.com/article/775507-overview
Hepatitis treatment
For the treatment of chronic viral hepatitis, antiviral agents of various pharmacological groups can be recommended. However, these drugs are difficult to tolerate and can cause serious adverse events. Therefore, they are not prescribed to all patients, but only to patients with a certain level of viral load and with an active inflammatory process.
Causes and symptoms of chronic hepatitis
For autoimmune hepatitis, hormonal anti-inflammatory drugs are prescribed. In severe cases (if glucocorticoids are ineffective), cytostatics may be recommended.
In case of toxic hepatitis, first of all, it is necessary to stop contact with the toxic agent - stop drinking alcohol, change the pharmacotherapy regimen, etc.
Regardless of the cause of chronic hepatitis, it is recommended:
- therapeutic diet Table No. 5
- Ursodeoxycholic acid (UDCA) preparations: protect hepatocytes from toxic damage and thus help the liver cope with its functions in conditions of illness, help reduce cholestasis (stagnation of bile), protect the nervous system from the negative effects of bilirubin and bile acids
- prokinetics: help restore normal motility of the gastrointestinal tract, including the biliary tract
- lactulose-based preparations help normalize intestinal microflora and eliminate toxic metabolic products that are not neutralized by the liver.
Chronic cholestatic hepatitis
Liver disease of a diffuse nature as a result of inflammation along the small bile ducts, stagnation of bile in the liver tissue.
The manifestations and complaints are the same as with other chronic hepatitis, but jaundice is more pronounced, which causes more severe skin itching, sometimes even before the skin turns yellow. Under the skin, in the corners of the eyes, yellow dense spots-xanthomas and xanthelasmas appear. A biochemical blood test shows a higher level of bilirubin, alkaline phosphatase (5 or more times higher than normal), and cholesterol. The principles of dietary nutrition and treatment are the same as for chronic active hepatitis, as well as vitamins A, E, B, Vicasol, to reduce skin itching - drugs that bind bile acids (bilignin, cholestyramine), choleretic.