What is intestinal colitis
Cramping pain is one of the symptoms of colitis
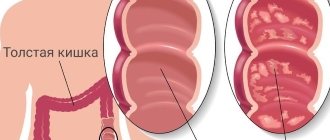
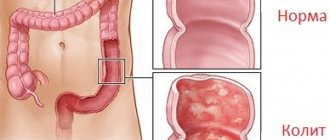
Intestinal colitis is a disease of the digestive system, namely inflammation of the mucous membrane of the large intestine. Colitis occupies one of the first places among diseases associated with digestive disorders. A survey was conducted among the population about what they know about this disease. It turned out that people do not consider it dangerous, but in fact this is far from the case.
Causes of colitis
- Poor nutrition. Abuse of spicy, fried and salty foods. Monotonous and poor diet with a lack of vitamins and minerals
- Drug therapy. Long-term use of drugs that disrupt the intestinal microflora (antibiotics, laxatives, etc.)
- Intestinal dysbiosis
- As a concomitant disease. Occurs against the background of various infectious diseases (dysentery or constipation, salmonellosis, helminthiasis), etc.
- Hereditary predisposition
- Decreased immunity
Colitis comes in many forms and types due to the fact that it can be caused by many other diseases. The most common of them are:
- Spicy
- Chronic
- Ulcerative
- Drug
- Ischemic
The symptoms of each individual type of disease differ from each other. In order to find out what kind of colitis it is, it is necessary to conduct a full examination and diagnosis of each individual case of the disease. We will touch on this issue a little later.
Diagnosis of colitis
Colitis is diagnosed as a result of a whole range of tests. This includes: macro and microscopy of stool, general blood test, contrast irrigoscopy and colonoscopy. These tests make it possible to detect the presence of helminth eggs, inflammation, and also to study the anatomical and functional features of the large intestine and the condition of the colon mucosa. During a colonoscopy, samples are taken for further histological examination. A proctologist also examines the patient; he examines the anus to exclude the possibility of hemorrhoids, paraproctitis and other pathologies.
Intestinal dysfunction can be complicated by inflammation. In addition, colitis may not be the main disease, but accompany the development of a colon tumor. Therefore, doctors take a biopsy of suspicious areas of the intestinal wall to conduct additional tests and exclude the possibility of malignant neoplasms. If enteritis or other diseases are suspected, a number of diagnostic procedures may be prescribed, for example, an ultrasound of the abdominal organs and functional tests to identify markers of inflammation of the liver and pancreas.
Acute colitis
Acute colitis develops rapidly
It occurs quite quickly and all the symptoms of this disease also develop rapidly. Symptoms:
- Repeated loose stools and vomiting
- A sharp increase in temperature, which can reach 38-39 degrees
- Ailments, weakness
- Loss of appetite
- Headache
- Dull or spasmodic pain in the abdominal area
Acute colitis is very dangerous for children under one year of age. Frequent bowel movements and repeated vomiting may cause dehydration or seizures. If acute colitis does not go away within 2 weeks, it becomes chronic. In this case, such patients periodically experience exacerbations.
Diagnosis and treatment
The diagnosis is made based on examination of the patient, as well as additional laboratory tests. In order to determine the causative agent of the disease, stool and blood tests are taken. To examine the intestinal mucosa, modern technologies are used in the form of endoscopy or x-rays.
Only after a thorough examination is a final diagnosis made.
Treatment occurs in two methods, which are used in parallel to each other. Maintenance therapy, which is aimed at preventing dehydration of the body. Drink plenty of water using water-salt solutions that restore water balance in the body.
Prevention of colitis
A good preventative measure to prevent the occurrence of colitis is a balanced diet. Proper nutrition will minimize the risk of various gastrointestinal diseases. It is recommended to exclude the consumption of alcohol, spices, canned food, and switch to fractional meals.
People with diagnosed chronic diseases of the large intestine should be under the supervision of specialists and undergo periodic medical examinations. It is better for them to avoid excessive physical activity and stress, not work at night and monitor their sleep patterns.
Even if you have not suffered from colitis before, no one is immune from this disease. Timely diagnosis and proper treatment of the disease are important, so undergo regular preventive examinations and consult a doctor at the first symptoms of colitis. Do not experiment with self-medication; drug abuse can only harm you.
Ulcerative colitis of the intestine
Refers to the chronic form of this disease, which has different degrees of severity:
- mild degree
- average degree
- severe disease
With mild to moderate ulcerative colitis of the intestine, a rise in temperature to 38 degrees, weakness, and malaise are observed. Changes in the digestive tract occur 2-3 days after the onset of an exacerbation. On the 3rd day, an increase in bowel movements is observed, which can be up to 10 times a day. In severe cases of the disease, the high temperature lasts for a long time, severe cramping pain, weakness, and dizziness.
As a rule, this form of colitis requires surgical intervention, since the danger is that ulcers on the intestinal mucosa can bleed. The presence of blood streaks in the stool indicates that the ulcer is bleeding. In this case, emergency hospitalization followed by surgery is necessary.
From clinical practice
Liver damage, although without obvious clinical manifestations, is quite common in chronic intestinal diseases. In adults, pericholangitis with the portal triad develops in 70% of cases. 50% have fatty liver changes. 10% acquire liver disease. Liver cirrhosis develops in 5%.Other, more severe and rare complications are chronic active hepatitis, sclerosing cholangitis and biliary tract carcinoma.
It should be noted that in children, chronic active hepatitis is a common complication, while pericholangitis and sclerosing cholangitis are very rare and are asymptomatic.
We present a clinical case of ulcerative colitis in a three-year-old girl. The initial phase of the disease was asymptomatic. Subsequently, pronounced hepatomegaly developed.
The girl was hospitalized at the age of three. 8 months before hospitalization, irritability, loss of appetite, intermittent abdominal pain, and stool mixed with scarlet blood were noted. With the symptoms described above, the girl was hospitalized. On examination, significant hepatomegaly was noted (+4 cm from below the costal arch along the right midclavicular line). In the blood test, ESR is 104 mm per hour; total blood protein 9.9 g%; albumin 2.5 g%; a1-globulin 0.3; a2-globulin 1.1; b-globulin 1.0; g-globulin 5.0; IgG 4810 mg%; alkaline phosphatase 1273 IU; Antinuclear and anti-smooth muscle antibodies are absent.
During hospitalization, the girl complained of frequent abdominal pain. There is an admixture of mucus and scarlet blood in the stool. Analysis of stool mucus revealed many neutrophilic leukocytes. Endoscopically revealed an extensive inflammatory process throughout the colon with swelling of the mucous membrane. Upon contact with the instrument, the mucous membrane bled easily.
With multiple biopsies, histological analysis was performed, which revealed thinning of the glandular ducts with mono- and polynuclear infiltration.
Percutaneous liver biopsy revealed inflammatory and granulomatous changes predominantly in the portobiliary spaces. Moreover, an inflammatory process such as pericholangitis and initial cholangitis in the interlobular ducts was noted.
Initial treatment with prednisone and subsequent salazopyridine (SAZP) resulted in complete remission of intestinal symptoms. Clinical remission with complete regression of hepatomegaly (the liver was palpated at the costal arch) was confirmed histologically. Laboratory parameters were also normalized (IgG 997 mg%).
It is known that ulcerative colitis is often accompanied by cow's milk protein intolerance, so a skin test and a test to determine specific IgE were performed. IgE levels were significantly increased.
Rapid clinical remission was due to two factors: the administration of salazopyridine (SAZP) and the simultaneous exclusion of cow's milk from the diet.
References 1. Walker Smith J., Crohn's Disease. In: Diseases of the small intestin in children. 1989. 2. Booth IW Chronic inflammatory bowel disease // Arch. Dis. Chid. 1991; 66: 742. 3. Elewaut D., De Keyser F., Culvelier C., Lazarovits AI, Mielants H., Verbruggen G., Sas S., Devos M., Veys EM Distinctive activated cellular subset in colon from patients with Chron's disease and ulcerative colitis 1998. 4. Casini-Raggi V., Kam L., Chong YJF, Fiocci C., Pizarro TT, Cominelli F. Mucosal imbalance of IL-1 and IL-1 receptor antagonist in inflammatory bowel disease. A novel mechanism of chronic intestinal inflammation // J. Immunol. 1995; 154: 2434-2440. 5. Olafsdottir E. J., Fluge G. and Hanf K. Chronic inflammatory bowel disease in children in Western Norway // J. Ped. Gastroen. North. 1989; 8: 454. 6. Castro M., Ansaldi N., Bianchi E. et al. Malattie inflammatorie chroniche intestinali: studio multicentrico italiano // Riv. Ital. Ped. 1991; 17:137. 7. Blaser MJ, Miller RA, Singleton J. W: Patients with active CD have elevated serum antibodies of seven enteric bacterial pathogens // Gastroenterology 1984; 87: 88-95. 8. Shanahan F., Duerr R., Rotter J. et al.: Neuthrophil autoantibodies in ulcerative colitis: familial aggregation and genetic heterogenety // Gastroenterology. 1992;103:456-461. 9. Halstensen T., Mollnes T., Garred et al. Surface epithelial related activation of complement differs un Crohn's disease and ulcerative colitis // Gut. 1992; 33: 902-908. 10. McNeish AS La diagnosi e la terapia della m. Di Crohn in eta pediatrica // Prospettive in Pediatria. 1988; 71: 245. 11. Shurmann G., Bretzler M., Meuer S. et al. Soluble IL-2r, IL-6 and IL-1 beta in patients with CD and US: preoperative levels and postoperative changes in serum concentrations // Digestion. 1991; 51: 51-59. 12. Sciumert R., Towner J., Zipser R.: Role of eicosanoids in human and experimental colitis // Dis. Sci. 1988; 33: 58-64. 13. McLain B.I., Diridson P.N., Stokes K.B. et al. Growth after gut resection for Crohn disease // Arch. Dis. Child. 1990; 65: 760. 14. Davies G., Evans CM, Shand WS, Walker Smith J. Surgery for Crohn's disease in childhood: influence of sites of disease and operative procedure on outcome // Br. J. Surg. 1990; 77: 91. 15. Booth IW The nutritional concequences of gastrointestinal disease in adolescence // Acta Pediatr. Scand. Suppl. 1991; 373: 91. 16. Layden T., Rosenberg J., Neuncharnsky B. Reversal of growth arrest in adolescents with Chronic disease after parental alimentation // Gastroenterology. 1979; 70: 101. 17. Hunter JO Nutritional factors in inflammatory bowel disease. 18. Morin CL, Rulet M., Roy CC, Webwn A. Contnous elemrntal enteral alimentation in children with Crohn's disease and growth failure // Gastroenterology. 1980; 79: 1205. Belli DC, Seiduman E, Bouthiller L et al. Chronic intermittent elemental diet improves growth failure in children with Crohn's disease // Gastroenterology. 1989; 97: 905. 19. Aiges H, Mancovitz J, Rma J et al. Home nactural sullplemental naso-gastric feedings in growth retarded adolescents with Crohn's disease // Gastroenterology. 1989; 97: 905. 20. Sanderson IL, Udeen S, Davies PSW et al. Remission induced by elemental diet in small bowel Crohn disease // Arch. Dis. Child. 1987; 62, 1223. 21. Giaffer MN, Nath G., Holdsworth CP Controlled trial of Polvmenic versus elemental diet in the treatment of active Crohn's disease // Lancet. 1990; 335: 816. 22. Seidman E., Leleiko N., Ament M. et al. Nutritional issues in pediatric inflammatory bowel disease // J. Ped. Gastroenterol. Nutr. 1991; 12: 424. 23. O'Sullivan M. A, O'Mora CA Nutritional therapy in Crohn's disease. 1998. 24. Zoli G., Care M., Parazza M., Spano C., Biagi PL, Bernardi M., Gasbarrini G. A randomized controlled study comparing elemental diet and steroid treatment in Crohn's disease. 1997. 25. Malchow H., Ewe K., Brandes JW, Coebell H., Ehms H., Sommer H., Jesdinsky H. European cooperative Crohn's disease study (ECCDS): results of drug treatment // Gastroenterology. 1984; 86: 249-266. 26. Prantera C., Pallone F., Brunetti G., Cottone M., Meglioli M. The Italian IBD study group: Oral 5-Aminoswlieye acid (Asacol) in the maintenance treatment of Crohn's disease // Gastroenterology. 1992; 103: 363-368. 27. Steinhart AH, Hemphill DJ, Greenberg GR Sulphasalazine and mesalazine for the maintenance therapy for Crohn's disease. A meta-analysis. DDW Abstract Book. 1994. A-2842. 28. Tremaine WJ Maintenance of remission in Crohn's disease: is 5-fminosalicylic acid the answer? // Gastroenterology. 1992; 103: 697-704. 29. Bernstein IH, Frank MS, Brandt LG et al.: Healing of perineal Crohn's disease with metrondazolo // Gastroenterology. 1980; 79: 357-365. 30. Markovitz J., Grancher K., Mandel F., Daum F. Immunosopressive therapy in pediatric inflammatory bowel disease: results of a survey of the North American Society of Pediatric Gastroenterology an Nutrition // A J. Gastroenterol. 1993; 88(1): 44-48. 31. Lloyd-Still JD Azathioprine and the treatment of chronic inflammatory bowel disease // J. Pediatr. 1990; 117(5):732-735. 32. Verhave M., Winter HS, Grand RJ Azathiopine in the treatment of children with inflammatory bowel disease // J. Pediatr. 1990; 117(5): 809-814. 33. Feldman M., Achord JM, Chang EB Cyclosporine in Crohn's disease - low doses won't do it // Gastroenterology. 1990; 98 (5): 1383-1384. 34. Balfour RB Cyclosporine therapy for inflammatory bowel disease // N. Eng. J. Med. 1994; 330(26): 1897-1898. 35. Sachar DB Cyclosporine treatment for inflammatory bowel disease. A Step Backward or a Leap forward? // N. Eng. Med. 1995; 321(13):894-896. 36. Geagan BG, Rochon J, Fedorac RN, Irvine EJ, Wild G. et al. Metrotrexate for the treatment of Crohn's disease // N. Eng. J. Med. 1995; 332(5):292-297. 37. Martin LW, Torres AL, Fisher JE, Alexandre F. The critical level for preservation of continuity in the ileo-anal anastomosis // JPS 1985; 20:664
Drug-induced colitis
This type of disease occurs as a result of long-term use of drugs that negatively affect the intestinal microflora. These include: laxatives, antibiotics and individual intolerance to certain types of drugs.
Drug-induced enterocolitis occurs due to improper treatment, and most often in people who try to treat themselves. Incorrect dosage or choice of drug can lead to serious consequences, including the occurrence of colitis. Don't treat yourself.
Methods for diagnosing the disease and preparing for them
Human thick intestine
In order to make an accurate diagnosis of colitis and its type, I use special methods of examining the large intestine. The data obtained make it possible to determine the severity of the disease as accurately as possible and prescribe the most appropriate treatment accordingly. There are two methods for diagnosing colitis.
The first method includes laboratory blood tests, which show the presence of inflammation in the body. For reliable results, blood is donated on an empty stomach.
How are inflammatory diseases and bowel cancer diagnosed?
The specialists of the multidisciplinary clinic “Trit” are proficient in all the techniques that allow them to identify even the smallest changes in the intestinal mucosa.
- An ultrasound examination is performed to detect thickening of the walls of the large and small intestine and narrowing of their lumen.
- Ultrasound with Doppler function allows you to check blood flow parameters.
- If necessary, an MRI OR CT scan is prescribed, as well as an x-ray examination.
- To detect blood in the stool, indicating the presence of bleeding in the gastrointestinal tract, laboratory tests are performed (including determination of fecal transferrin and hemoglobin).
The “gold standard” of research is a modern endoscopic technique, intestinal colonoscopy under anesthesia. If the patient has extraintestinal manifestations of the disease, doctors of relevant specialties - an ophthalmologist, dermatologist or rheumatologist - are also involved in the diagnosis.