Tubular adenoma of the colon is a benign neoplasm on a pedicle or broad base, arising from the epithelium of the colon and rising above it. Tubular adenoma refers to adenomatous polyps, which, according to modern concepts, are precancerous diseases of the colon, which explains the close attention of coloproctologists to this problem.
- Tubular adenoma of the colon - what are its features?
- Tubular adenoma of the colon with dysplasia
- Reasons for development
- Diagnosis and treatment
- Prevention of the development of tubular adenomas
Tubular adenoma of the colon - what are its features?
Colon adenomas occur more often in men than in women, and mainly in older people. Tubular adenomas can have different sizes, but small ones are more common, up to 1 cm in diameter. When examining the colon, either one solitary adenoma or several can be detected. There is an opinion that it is numerous adenomas of the colon that are obligate precancer, that is, they have an almost one hundred percent risk of degeneration into a malignant tumor.
Tubular adenoma is the most common type of adenomatous polyps of the colon; according to the literature, they occur in 75-87% of cases. Can be detected in any part of the intestine. A feature of tubular adenoma is its histological structure, determined predominantly by tubular - as the name suggests - structures. At the microscopic level, tubular adenoma of the colon consists of glandular tubes that are longer than those in the normal mucosa.
Macroscopically, tubular adenomas have a stalk and a smooth lobulated surface, less often a wide base. They are similar in color to the surrounding mucous membrane, but have a denser consistency, move along with the mucous membrane, and rarely bleed or ulcerate.
In addition to tubular adenomas, there are two more types: tubulovillous adenoma and villous adenoma. Of the three listed, tubular adenomas have the least potential for malignancy (although it cannot be completely excluded), but over time, villous components may appear and predominate in their structure, that is, a tubular adenoma can turn into tubulovillous, and then into villous, which is at risk degeneration into a malignant tumor is already significant.
Diagnostics
The following diagnostic methods are used to detect intestinal neoplasia:
- Endoscopic examination of the intestine - total colonoscopy (examination of the entire surface of the colon) and its shortened version - rectoscopy and rectosigmoidoscopy - examination of the rectum and sigmoid colon. This method allows you to visualize tumors in the early stages, even before symptoms develop, to remove them, and if this is not possible, to perform a biopsy. Currently, colonoscopy is the gold standard for diagnosing colon neoplasia.
- Fecal occult blood test. This method is used to detect polyps and tumors that have an ulcerated surface and bleed. As a rule, we are talking about fairly large neoplasms. This examination is carried out as part of colorectal cancer screening. If the result is positive, further colonoscopy is indicated.
- Irrigoscopy is an X-ray examination of the colon. First of all, it makes it possible to detect exophytic neoplasms and tumors that deform the intestinal lumen and intestinal wall.
If malignant neoplasia of the intestine is detected, additional examination is carried out to determine the stage of the disease. This includes ultrasound, CT, MRI, and a number of laboratory tests.
Tubular adenoma of the colon with dysplasia
Each of the identified adenomas, regardless of type and structure, has signs of dysplasia. There are three degrees of dysplasia - mild, moderate and severe (or high). The degree of dysplasia is determined by histological examination of the removed adenoma based on a number of characteristics. Predominantly adenomas with a mild degree of dysplasia are diagnosed. The larger the size of the adenoma and the older the patient, the greater the risk of developing an adenoma with signs of severe dysplasia. The degree of dysplasia is one of the most important factors in the malignancy of an adenoma, along with its size, location, duration of the disease and replacement of the tubular structure with a villous one. An extreme degree of dysplasia is usually equated to cancer in situ. At the same time, epithelial dysplasia itself is not cancer, but since it is essentially a violation of the normal tissue structure of a part of an organ, in this case the colon, it can, with further progression and an increase in its severity, lead to the appearance of tumor cells.
Stages of the tumor process
When diagnosing malignant intestinal neoplasia, the stage of tumor spread is of great importance. The prognosis of the disease and its treatment regimen depend on this. The following stages are distinguished here:
Cancer in situ - malignant cells are found only in the intestinal mucosa.
Stage 1 – the tumor grows into the submucosal layer.
Stage 2 – the tumor spreads to the muscle layer of the intestinal wall.
Stage 3 – the tumor grows throughout the thickness of the intestinal wall and can spread to the visceral peritoneum and fatty tissue. Metastases are detected in regional lymph nodes.
Stage 4 – tumor of any size with distant metastases (liver, lungs, brain).
Reasons for development
The main reason for the development of tubular adenomas has not yet been established, but factors that can lead to their appearance have been identified.
Heredity plays an important role in the development of tubular adenoma of the colon.
Diffuse hereditary polyposis and familial adenomatous polyposis syndrome of the colon are diseases in which multiple colon adenomas develop, including tubular ones, which have the highest risk of degeneration into cancer. Therefore, patients with such syndromes require surgical treatment as early as possible, and their close relatives require careful screening monitoring.
Other reasons for the development of tubular adenomas include the following:
- A diet high in refined foods, animal fats and insufficient fiber intake,
- Dysbiosis of the colon, since in this condition local immunity is impaired and the restoration of the mucous membrane of the intestinal wall is impaired,
- Chronic diseases of the large intestine, primarily inflammatory,
- Diverticulosis,
- Frequent constipation and intestinal dyskinesia,
- Physical inactivity, excess body weight.
Causes of intestinal endometriosis
The immediate cause of intestinal damage is the spread (contact or hematogenous) of elements of the uterine mucosa into the wall with further implantation. This can occur due to hormonal imbalance, when particles enter during the rupture of an endometrioid ovarian cyst, there is also a version of retrograde menstruation, in which elements of the endometrium in the menstrual blood enter outside the uterus. Unfavorable factors that increase the likelihood of developing the disease are decreased immunity, diseases of the female genital area, stress, lack of mobility, and heredity.
Video from the operating room. Laparoscopic surgery for retrocervical endometriosis
Diagnosis and treatment
Colon adenomas usually do not manifest any symptoms and are an incidental finding during screening or examination for other complaints.
In rare cases, a tubular adenoma of the colon may bleed, which becomes a reason to consult a doctor. In addition, patients may complain of abdominal pain, frequent constipation or diarrhea.
The gold standard for diagnosis is colonoscopy. In addition to it, irrigoscopy and sigmoidoscopy may be prescribed.
There is an opinion according to which endoscopic removal of only adenomas with a diameter of more than 5 mm is recommended, since smaller formations become malignant extremely rarely and dynamic observation is acceptable. However, a more common tactic is in which all adenomas are removed, regardless of the size of the tumor, since histological studies show that polyps even less than 5 mm in diameter in 60-70% of cases have tubular-type areas and, accordingly, have the potential to degenerate into malignant formations.
There is currently no effective conservative treatment for tubular adenomas, and patients are advised to undergo surgical treatment. The tactics of surgical treatment largely depend on the diagnostic method used to diagnose colon adenoma with dysplasia. If the patient undergoes a colonoscopy, then all detected polyps larger than 5 mm are removed. If polyps were identified during another type of intestinal examination (for example, irrigoscopy), then if a small tubular adenoma of less than 1 cm is detected, a biopsy must be performed, and after confirming the diagnosis, the patient is shown a colonoscopy to remove all visualized adenomas and their histological examination. If a colon adenoma larger than 1 cm in size has been identified, then there is no need for a biopsy - the patient must be immediately referred for a colonoscopy. Thus, colonoscopy for detected adenomas becomes both a diagnostic and therapeutic measure.
When adenomas are localized in the colon, removal is carried out endoscopically through a colonoscope. If the adenoma is located in the rectum, removal can be performed using an endoscope or by transanal endomicrosurgery. The peculiarity of this operation is that in this case the tubular adenoma is removed simultaneously with resection of the intestinal wall. This is explained by the fact that when an adenoma is localized in the rectum, in almost every third case, cancer cells are already detected at its base.
In the case of multiple polyps (so-called diffuse lesions), it is advisable to perform a colotomy or resection of the affected area of the intestine.
Unfortunately, tubular adenomas are prone to recurrence. The most common cause of relapse is incomplete removal of the base of the adenoma, if it is not located on a long stalk. In case of recurrent tubular adenoma, surgical removal of the affected area of the colon by laparotomy may be required, since postoperative changes may be an obstacle to complete endoscopic removal of the recurrent adenoma.
Non-surgical treatment of atypical endometrial hyperplasia in 1 session of photodynamic therapy
Afanasyev Maxim Stanislavovich.
Doctor of Medical Sciences, Professor at Sechenov University, oncologist, surgeon, gynecological oncologist, gynecologist-immunologist, expert in the treatment of atypical hyperplasia and uterine cancer, as well as precancerous and tumor diseases of the cervix.
Atypical epithelial hyperplasia is a diagnosis that in gynecological oncology is clearly classified as a precancerous disease with a high degree of carcinogenicity - the ability to degenerate into cancer.
Doctors try to treat women of reproductive age. They carry out severe hormonal therapy or a surgical procedure - laser ablation of the endometrium. Both of these methods have quite serious consequences.
When taking hormones, women enter a menopausal state and experience complications such as weight gain, fatigue, decreased libido, and an increased risk of thromboembolism (1, 2).
A frequent complication of ablation is the development of the so-called Joseph Asherman syndrome, when the uterine cavity grows together during the healing process.
Unfortunately, atypical uterine hyperplasia is a very serious disease that is difficult to treat. Ablation and hormonal therapy for endometrial hyperplasia with foci of atypia are effective only in a certain percentage of cases.
Given the ineffectiveness of hormone therapy and ablation, medicine today can offer virtually the only way to avoid the malignancy of the process and save life. This method is removal of the uterus. Often, indications require removal of the uterus along with the appendages - that is, along with the fallopian tubes and ovaries. Therefore, the lack of effect against the background of hormonal treatment or ablation always ends in the same way - with a radical recommendation to get rid of the uterus.
I have been closely dealing with the problem of treating precancerous diseases of the cervix and uterus for more than 10 years and have reason to assert that even complex atypical hyperplasia can be successfully treated and does not require surgery. The new high-tech method of photodynamic therapy (PDT), which I use in my practice, ensures recovery in more than 80% of cases in 1-2 sessions.
The non-surgical PDT method allows you to save the uterus, and with it preserve women’s health, the ability to conceive and give birth independently.
Before continuing our conversation about atypical hyperplasia, let's define what is hidden behind this term and what is the nature of the disease. This will allow you to understand why classical methods are little effective against atypia and evaluate all the benefits of PDT.
What is uterine hyperplasia
The inside of the uterus is lined with a mucous layer - the endometrium. The endometrium is not homogeneous. It consists of:
1. uterine glands and
2. stroma - service tissue that supports the glands and provides them with nutrition.
Normally, the stroma and glands occupy approximately equal volume, 1:1.
| The structure of the healthy endometrium of the uterus and the endometrium with adenomatosis. |
Every month, at the time of ovulation, the uterus prepares to receive an egg, and the thickness of the endometrium increases. After the egg is released from the ovary, the endometrial glands are activated and begin to produce mucus (secret), creating a favorable environment for fertilization. When fertilization does not occur, the endometrium peels off and comes out along with the blood.
If for some reason the endometrium is not shed during menstruation (for example, the woman did not ovulate this cycle), it continues to grow. This condition is called endometrial hyperplasia.
Classification of endometrial hyperplasia
Endometrial hyperplasia is divided into:
1. simple endometrial hyperplasia,
2. atypical endometrial hyperplasia.
If the thickness of the endometrium increases locally, in certain areas, this condition is called focal hyperplasia. If everywhere throughout the entire uterine cavity - diffuse.
But since not all gynecologists and morphologists have adopted the new classification, in the article I will use all existing names for this diagnosis.
What is simple endometrial hyperplasia
This is the initial stage of hyperplasia, which is characterized by thickening of the endometrium and a slight uneven arrangement of the uterine glands, some of which turn into cysts - clogged glands, expanded from the inside with their own secretions. The ratio of the uterine glands and stroma is approximately healthy - 1:1.
Simple forms of hyperplasia today include the following diagnoses:
- glandular endometrial hyperplasia,
- cystic endometrial hyperplasia,
- glandular cystic endometrial hyperplasia.
The combination of several of these types was previously classified and interpreted by colleagues as complex hyperplasia.
Hyperplasia is manifested by bleeding or spotting during the period between menstruation. Ultrasound reveals a heterogeneous echostructure of the endometrium.
Due to stress - time zone change, lack of sleep, lack of ovulation (anovulatory cycle) and nervous overstrain - simple glandular hyperplasia can manifest itself in the most normal cycle even in the healthiest woman. Therefore, we can say that signs of simple hyperplasia are observed throughout life in 90% of women.
This condition can be quite easily corrected with gestagenic drugs, as well as Duphaston, Norkolut, Utrozhestan, etc. Young patients are often prescribed combined oral contraceptives for treatment - Jess, Janine and others.
Simple endometrial hyperplasia is not a precancerous condition and does not require special antitumor treatment.
What is atypical uterine endometrial hyperplasia, or adenomatous endometrial hyperplasia (code N85.1 in ICD-10 - International Classification of Diseases, 10th revision)
Endometrial adenomatosis, or atypical uterine hyperplasia, is a stage of development of hyperplasia, which is characterized by the appearance of atypical cells. The word "atypical" means almost the same thing as "atypical": these cells do not look like normal ones.
All our cells have a clear shape, are arranged in layers and perform a specific function. But for some reason (scientists have not come to a consensus on the reasons for the development of atypia in the endometrium of the uterus), they change their shape, size and cease to perform the function inherent in nature.
The appearance of atypical cells is a very serious call! This stage of development of hyperplasia in medicine refers to precancerous diseases of the uterus.
Atypical cells continue to divide and accumulate damage. If the process is not stopped, the atypical form of hyperplasia leads to the appearance of malignant cells and develops into uterine cancer.
Between a benign and a malignant cell there is a stage when the cell loses its typical properties and acquires atypical ones. Such cells have some properties of cancer, but are not yet full-fledged cancer.
Atypical endometrial hyperplasia in medical practice goes by several names - complex or complex hyperplasia with cell atypia, adenomatous endometrial hyperplasia, atypical glandular endometrial hyperplasia, focal endometrial adenomatosis, complex hyperplasia with atypia, glandular endometrial hyperplasia with atypia, cystic adenomatous hyperplasia, focal hyperplasia with cell atypia and atypical glandular hyperplasia of the endometrium. Some of them are outdated, but are still used today.
And no matter what diagnosis you are given from this list, when atypia appears, all these conditions are interpreted as precancerous and treated the same way.
This form of hyperplasia received the name “adenomatous” not by chance. Adenoma is a benign tumor formed from glandular epithelial cells, in our case from the epithelium of the uterine glands.
How does complex atypical endometrial hyperplasia manifest?
Complex endometrial hyperplasia with cell atypia is accompanied by proliferation of the glands of the uterine mucosa. A large number of uterine glands in a limited area are located very tightly to each other and are deformed. The ratio of glandular tissue and stroma shifts to a proportion of 2:1. The overall structure of the endometrium is significantly disrupted.
Many glands become clogged, overfilled with their own secretions, and form cysts and adenomas.
Complex atypical endometrial hyperplasia is a true precancer of the uterine body. According to the literature, the frequency of degeneration of atypical hyperplasia into cancer is about 30%.
Atypical endometrial hyperplasia can develop into cancer - this is its main danger
Unfortunately, not only can it, but it also passes on - atypical endometrial hyperplasia has a high risk of malignancy.
Statistics vary greatly, but in general, from 23 to 81%*** of cases of atypical hyperplasia lead to uterine cancer.
On the one hand, such a spread in numbers is explained by different periods of observation of patients with atypical hyperplasia (with long-term observation, the figure approaches 100%).
On the other hand, even a qualified pathologist who examines cells under a microscope and determines the degree of their malignancy has difficulty making a diagnosis.
We will not go into the intricacies of the work of a pathologist, but believe me, it is extremely difficult to unambiguously differentiate the precancerous and initial cancerous state of the endometrium. And some see atypia where others already see cancer.
Is atypical uterine endometrial hyperplasia cancer?
Atypical hyperplasia is not cancer in the true sense of the word:
- no tumor growth
- there is no growth of atypical cells beyond the basement membrane,
- there is no transfer of a large number of atypical cells into the bloodstream (the so-called “germination” of the tumor),
- cells have not acquired the ability to metastasize.
That is, atypical cells have already acquired the properties of cancer cells - they are of different sizes and have enlarged nuclei, but have not yet overcome the body’s resistance.
I repeat once again that the issue of atypical processes in the uterus is not at all easy. Making a diagnosis based on biopsy material or after curettage is extremely difficult. Therefore, if a diagnosis of “atypical uterine endometrial hyperplasia” is suspected, a review of the glasses is almost always accompanied by a new conclusion from the pathologist.
Accurate diagnosis of the nature of foci of adenomatosis is possible only after removal of the uterus, when a specialist has the opportunity to specifically examine the structure of the endometrium to its entire depth. That is, do not conduct a cytological examination (examination of cells), but a histological examination (examination of tissues), which allows you to obtain a more accurate result.
Meanwhile, according to literature data, diagnostics of uterine tissue after hysterectomy reveals endometrial cancer in every third and even every second (54%) patient***!
How was previously treated for atypical endometrial hyperplasia?
Previously, after making a diagnosis of “focal atypical endometrial hyperplasia,” gynecologists could not please their patients with the availability of an effective non-surgical treatment method and a favorable prognosis for recovery.
As I already said, the standard international approach to treating uterine adenomatosis in young women involves taking heavy hormonal drugs , such as Depo Provera and its analogues. This method is also called “hormonal curettage.” This hormonal treatment is aimed at enhancing secretion - rejection of hyperplastic endometrium.
If there is no effect, treatment of adenomatous endometrial hyperplasia is carried out surgically - by ablation (evaporation) of the endometrium using a laser, followed by curettage (curettage). Endometrial curettage is performed no more than three times, since this treatment method has a high risk of developing synechiae, a complication as a result of which the internal walls of the uterus often grow together during the healing process.
Women of reproductive age planning to have children are prescribed hormonal treatment with progesterone after curettage.
It is important to understand that in case of glandular hyperplasia with atypia, hormonal treatment can reduce the thickness of the endometrium, but has little effect on atypia, and atypical cells continue to divide . That is, progesterone therapy is not cancer prevention.
If all of the above methods are ineffective, the woman undergoes hysterectomy.
Here I will quote the words of my colleague, a professor, who quoted to me the patient management tactics adopted in the West: “Long-term observation after treatment should be carried out every 6-12 months until a hysterectomy is performed.” Yes, in recent years, European medicine, at the slightest appearance of atypia, often refers the patient to removal of the uterus, thus eliminating the risk of atypia degenerating into cancer.
“Hysterectomy”, or removal of the uterus, is the modern international tactics for managing patients with hyperplasia with cell atypia, adopted in Europe and America. And although Western medicine also prescribes hormone therapy for women who have not given birth, the final outcome in the form of hysterectomy is considered inevitable for both women who have given birth and those who have not given birth of any age.
For women after 45 - 50 years old - at an age close to menopause or postmenopause, especially in the presence of adenomatous polyps, medicine does not offer any alternative options other than radical removal of the uterus and appendages.
This tactic saves lives, but leads to the development of extremely serious complications.
Consequences of hysterectomy
On this occasion, I wrote an article explaining the consequences of removing the uterus for a woman.
First of all, this concerns a different quality of life after surgery. As they say, nature did not intend to have extra organs. And it is clear that when an organ is lost, even for medical reasons, the function of this organ is also lost. But this is only part of the problem. Neighboring organs also experience extremely negative effects after surgery.
After removal of the uterus, the urinary system is seriously affected, the functioning of the colon is disrupted, high blood pressure develops, and the risks of heart attacks and strokes seriously increase.
Women of reproductive age who are sexually active have to adapt not only to changes in sensations during sex, but also to the changed size of the vagina.
In an effort to find an effective treatment without organ removal, I developed a protocol for the treatment of atypical endometrial hyperplasia using photodynamic therapy.
How does the photodynamic therapy procedure work?
- After a thorough examination, the patient is given the photosensitizer drug “Fotoran” or “Photodinazine” and its analogues intravenously. This substance selectively accumulates in old, atypical, damaged and inflamed cells of the uterine mucosa and almost does not accumulate in healthy ones.
- After 2.5 - 3 hours according to the protocol developed jointly with the Center for Laser Medicine of the First St. Petersburg State Medical University. acad. I.P. Pavlova (scientific director of the center, doctor of medical sciences, prof. Petrishchev N.N., researcher Grishacheva T.G.), using a special method that we have developed, irradiation of the uterine cavity is carried out with an intrauterine balloon light guide.
| Disposable intrauterine light balloon for photodynamic therapy. |
- Such a light guide allows you to evenly distribute the light of the laser beam and obtain a full therapeutic effect.
- In my practice, I use only disposable intrauterine light cylinders. Using a new cylinder each time ensures that it glows properly at the specified power, which is critical for achieving the desired photodynamic effect and protects against the risk of infection.
- To achieve an adequate photodynamic effect, I develop a treatment protocol for each patient individually.
- Under the influence of laser radiation in the red spectrum, the photosensitizer enters into a photochemical reaction with oxygen to form so-called active singlet oxygen, a powerful oxidizing agent that damages the membranes of atypical cells and causes their death.
- Singlet oxygen is also an aggressive environment for bacterial and viral infections and destroys them. This allows one procedure to treat concomitant inflammatory diseases of the uterus, such as endometritis.
- Since each atypical cell accumulates a photosensitizer, PDT eliminates all areas of adenomatosis. The photosensitizer is removed from healthy cells 1-1.5 hours after administration, and they are not damaged during the treatment.
It is this selective effect that ensures complete removal of atypical cells and hyperplastic endometrium and recovery after the procedure.
- After PDT, the body launches natural mechanisms for recycling damaged atypical cells and their decay products.
- Healing after PDT occurs with the formation of a healthy and complete endometrium of the uterus.
How does healing occur?
6–7 weeks after a session of photodynamic therapy, the mucous membrane heals without scars. A healthy uterine epithelium is formed.
Within six months, all patients undergo 3-fold monitoring, which includes:
- Ultrasound with a vaginal probe,
- conducting a scarification biopsy of the endometrium of the uterus with examination using liquid cytology.
In the future, you will need to visit a gynecologist once every six months for preventive examinations.
Patient, 34 years old, Moscow, diagnosed with atypical endometrial hyperplasia
I was diagnosed in the winter of this year. Since January 2015, menstruation stopped coming on its own. As prescribed by gynecologists, she took gestagenic drugs (Duphaston) continuously.
Here it should be noted that there are complaints characteristic of atypical (complex) endometrial hyperplasia - the absence of independent menstruation, a sign of endometrial pathology. In May 2016, when performing separate uterine curettage and hysteroscopy, the diagnosis was again confirmed. Histological report after revision in the laboratory of the Institute of Oncology named after. Blokhin No. 24730: in ready-made preparations and preparations prepared from the block in scraping, pieces of endometrial polyp with a picture of simple glandular hyperplasia without atypia and complex atypical hyperplasia. Special antitumor treatment including hysterectomy and hormone therapy is indicated. She was consulted at the same cancer center named after. Blokhina, decided to abstain from the proposed hormone therapy in favor of a session of photodynamic therapy.
In October 2016, photodynamic therapy of the uterus was performed. The postoperative period was without complications. Pipel endometrial biopsy dated 02/03/2017, histological conclusion No. 171005746: “most likely a fragment of a glandular endometrial polyp of the hyperplastic type with focal stromal fibrosis and foci of lymphocytic infiltration is identified.”
In order to prevent relapse of atypical hyperplasia, in April 2017, the patient underwent a second session of PDT of the uterus, before which separate curettage of the uterus was performed, histological conclusion No. 171020496: “focal simple glandular hyperplasia of the endometrium without atypia with a brush transformation of the glands.”
The patient is cured. Clinical sign of recovery: since December 2016, the patient’s cycle was restored and menstruation began to come.
Today the patient is healthy and planning a pregnancy.
Why should endometrial adenomatosis be treated using PDT?
I cannot guarantee that PDT can cure atypical endometrial hyperplasia 100%, since the cause of this disease is fundamentally complex (hormonal).
But my many years of practice and independent international research are very encouraging. After PDT, there is an obvious inhibition of hyperplastic processes in the uterine mucosa: hyperplasia stops its development and does not recur for a long time.
1. Photodynamic therapy specifically eliminates atypical cells and, as a result, eliminates the risk of developing uterine cancer.
After correctly performed photodynamic therapy with the occurrence of adequate photochemical reactions, we can say that there are no atypical cells left in the treatment area. This means that there is simply nowhere for relapse to occur.
2. Photodynamic therapy preserves the uterus - an organ that is important not only for the birth of children, but also for the normal functioning of the entire female body - from the intestines to the blood vessels.
3. The procedure does not affect the deep layers of the uterus, it allows you to preserve the integrity of the uterus and all the functions of a healthy organ. Such a uterus subsequently allows you to conceive, bear and give birth.
At the same time, obstetricians and gynecologists observe an interesting fact in their practice - pregnancy and lactation have a beneficial effect on a woman’s hormonal levels and serve as excellent prevention: after childbirth, endometrial hyperplasia develops extremely rarely.
4. Studies** on the effectiveness of PDT show the amazing ability of the procedure to inhibit the excessive growth of the uterine epithelium.
Over the course of 6 months of observation, after one PDT session, hyperplasia was not detected in 82% of patients, and in another 7% it regressed after a second PDT session.*
This is reassuring and gives time to everyone planning a pregnancy.
Of my five patients with treated atypical hyperplasia, four have already been controlled and are healthy. One is still under observation awaiting control.
5. PDT excludes fusion of the internal walls of the uterus - a common complication after surgical ablation.
Through the prism of my many years of experience in using PDT in the treatment of atypical endometrial hyperplasia, I can confidently speak about the successful implementation of the first commandment of a doctor - do no harm. It will not get worse, and the high – more than 80 percent – probability of cure is a good reason to eliminate the focus of atypical hyperplasia using PDT. You will always have time to make a decision to remove the uterus.
Thus, of all organ-preserving methods of treating endometrial hyperplasia with atypia, photodynamic therapy is the most effective.
Results of treatment of a 39-year-old patient, Moscow
The second patient, 39 years old, is also from Moscow. The nature of her complaints is a reason to see a doctor, which is completely non-specific, one might say, for a gynecological patient. Pain in the lower abdomen and in the area of the cross, radiating to the leg. During the examination, an ultrasound of the pelvic organs was performed, the conclusion: from December 2016: “echosigns of endometrial polyp, adenomyosis.”
It is worth noting the second sign, which allows one to suspect atypical endometrial hyperplasia - data from an ultrasound examination of the pelvic organs (ultrasound), namely the presence of polyps in the uterus or heterogeneous tissue in the uterine cavity.
In February 2022, separate curettage of the uterus was performed under hysteroscopy control. Histological conclusion No. 5618-57: “glandular-fibrous endometrial polyp with foci of complex glandular hyperplasia and cytoloic atypia with an area of glands under construction similar to adenocarcinoma.”
And here I made no mistake. Because it's cancer. The first revision of glass preparations at the Institute. Blokhin confirmed the diagnosis. And the third morphologist at City Clinical Hospital No. 62 and the review of another class specialist at the same institute named after. Blokhin (this was the fourth morphologist who gave his conclusion), histological conclusion No. 8203: “foci of atypical endometrial hyperplasia with foci of squamous metaplasia, developed in glandular fibrous polyps against the background of focal typical endometrial hyperplasia. No reliable signs of malignant tumor growth were found within the sent material.”
Before contacting me for a consultation, I recommend taking histological blocks and glass slides for review to the Institute named after. Blokhina on Kashirskaya metro station. Atypical endometrial hyperplasia is a true precancer or, one might say, stage 0 cancer. And different morphologists can interpret this in their own way.
It is often difficult to draw a clear line to distinguish severe precancer from the initial form of cancer, and this does not necessarily characterize the qualifications of the morphologist.
In March 2022, photodynamic therapy of the uterus was performed. The postoperative period was without complications. The operation was performed on Wednesday, and on Sunday the patient, with discomfort in her abdomen, flew on vacation to Europe. The next menstruation came on time. 1 month after the operation, at the end of April, a pipel biopsy of the endometrium was performed, histological conclusion No. 171028350: “endometrium of the middle stage of proliferation. Chronic endocervicitis with squamous metaplasia. The morphologist described artifacts of the healthy state of the uterine and cervical mucosa.”
The patient is healthy, 2 months after the follow-up examination we will plan a pregnancy.
Foreign experience in the treatment of uterine hyperplasia using PDT confirms its high effectiveness
The basis for improving my PDT technique was the work of doctors from South Korea (3), who treated several patients with well-differentiated adenocarcinoma of the uterine endometrium and obtained an indicative result.
Above, we have already talked about the difficulties of distinguishing between severe atypical endometrial hyperplasia (dysplasia) and well-differentiated endometrial adenocarcinoma. Therefore, the data from Korean colleagues can be considered relevant for cases of atypical hyperplasia.
The treatment included a group of patients of reproductive age 24-35 years old. In 10 out of 16 patients, recovery was achieved after one PDT session. Another two patients achieved recovery after the second and third PDT sessions, respectively.
Thus, the rate of positive response to PDT treatment was 75% (12/16).
Of the 7 patients who attempted to become pregnant after treatment, four patients (57%) had seven successful pregnancies, which resulted in 6 live births.
It is also worth noting that after successful treatment with PDT over 78 months of observation, no relapse of the disease was observed in any of the patients. There were also no serious side effects associated with photodynamic therapy.
The probability of a complete cure for atypical hyperplasia is at least 75% after just one PDT session.
Why is the field of PDT in medicine not developing?
The idea and experience of using photodynamic therapy in the treatment of atypical endometrial hyperplasia and uterine cancer is not new. Work on photodynamic therapy was carried out at the Department of Obstetrics and Gynecology of the II Medical University. N.I. Pirogov.
1. The method is technologically complex and combines three areas of science: medicine, biology and physics. None of these components can be considered secondary.
As a result, a PDT practitioner must take a multidisciplinary approach and be a specialist in different fields of knowledge. Not every doctor can do this.
2. Doctors know little about this method or don’t know at all , although it is already included in the federal standard of care in obstetrics and gynecology for cervical pathology with CIN - see Order of the Ministry of Health of Russia dated November 1, 2012 N 572n (as amended on June 11. 2015) “On approval of the Procedure for providing medical care in the field of obstetrics and gynecology (except for the use of assisted reproductive technologies)” (Registered with the Ministry of Justice of Russia on April 2, 2013 N 27960).
3. Catheters according to the shape of the uterus are not currently produced. As for the treatment of the uterus, the technology is complicated by the fact that the uterus is a hollow, triangular-shaped muscular organ. About 5 years ago, balloon catheters in the shape of the uterus were produced in Russia and Switzerland, but recently their production has been stopped.
Today, I, together with Doctor of Physical Sciences, Professor V.B. Loschenov. (BIOSPEC JSC) initiated the development and certified production of a new generation intrauterine balloon light guide.
Indications for photodynamic therapy of uterine precancer
- simple recurrent hyperplasia in the absence of effect after taking progestin drugs,
- complex endometrial hyperplasia, both against the background of hormonal treatment and in monotherapy - as the only method of treating hyperplasia.
- relapse of endometrial hyperplasia after lack of effect from hormonal treatment and 2-3 procedures of separate diagnostic uterine curettage.
- relapse of atypical endometrial hyperplasia after hormonal treatment or laser ablation of the endometrium.
- well-differentiated endometrial adenocarcinoma in the reproductive period,
- old age with concomitant diseases of the heart and other organs,
- refusal for objective reasons from standard surgical and chemoradiotherapy treatment.
To get advice on whether photodynamic therapy is indicated for you, and to calculate the price of the procedure, send your medical history and tests by e-mail or call by phone in Moscow.
The reception is conducted by Afanasyev Maxim Stanislavovich, obstetrician-gynecologist, oncogynecologist, oncologist, immunologist, Doctor of Medical Sciences, professor and member of the academic council of the First Moscow State Medical University. THEM. Sechenov Ministry of Health of the Russian Federation, expert in the treatment of atypical uterine hyperplasia.
Reception is carried out in two clinics in Moscow, as well as in St. Petersburg, Makhachkala, Kursk, Stavropol, Barnaul, Samara, Naberezhnye Chelny, Salavat, Chelyabinsk, Surgut and other regions of Russia. You can check the date, location of the appointment in your city and sign up for a consultation with the administrator by calling +7 (495) 204-18-93.
After treatment, I maintain feedback with all patients and resolve any issues that arise. Hepatitis and positive HIV status are not contraindications for treatment with PDT.
Used materials:
1. Ramirez PT, Frumovitz M, Bodurka DC, et al. Hormonal therapy for the management of grade 1 endometrial adenocarcinoma: a literature review. Gynecol Oncol. 2004;95:133-138.
2. Banno K, Kisu I, Yanokura M, et al. Progestin therapy for endometrial cancer: the potential of fourth-generation progestin [review]. Int J Oncol. 2012;40:1755-1762.
3. Preservation of fertility by photodynamic therapy in young patients with early stage endometrial carcinoma. Long-term study based on follow-up of patients. Authors: Min Chul Choi, Sang Geun Jung, Hyun Park, Yoon Hyun Cho, Chan Lee, Seung Jo Kim.
4. ** Pasman N. M., Nikonov S. D., Antonyuk I. V. et al. Hysteroscopic photodynamic therapy of patients with chronic endometritis and endometrial hyperplasia / Bulletin of NSU. Series: Biology, clinical medicine. 2011. T. 9. Issue. 2. pp. 7-13. — ISSN 1818-7943.
5. *** Novikova E.G., Chulkova O.V., Pronin S.M. Treatment of atypical endometrial hyperplasia / Practical Oncology. 2004. T. 4, No. 1. P. 52-59.
Prevention of the development of tubular adenomas
In many cases, colon adenoma is a sign of a hereditary disease, so patients with a family history of colon diseases, including cancer, form a risk group that should be under close medical supervision and regularly undergo screening tests for the early detection of adenomas.
Since chronic diseases of the large intestine, such as colitis, can contribute to the development of tubular adenomas, treatment or compensation of these diseases will also prevent the formation of adenomas.
Since nutritional factors such as high fat content, especially refined fat, and low dietary fiber content in the daily diet are directly related to the appearance of intestinal adenomas, diet correction will help not only prevent the appearance of tubular adenomas, but also have a positive effect on the growth dynamics of existing ones adenoma.
A connection has also been identified between smoking and the development of tubular adenomas, and the number of adenomas is directly proportional to the duration of smoking, so giving up this bad habit will have a positive effect not only on the lungs, but also on the colon.
Finally, since the development of colon adenomas is promoted by a sedentary lifestyle and excess body weight, exercise and weight management may also be a reasonable recommendation for the prevention of the development of tubular adenomas.
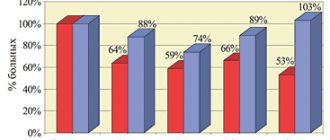
In the case of already identified tubular adenomas, dynamic monitoring of patients using endoscopic methods is indicated. The frequency of examinations is determined individually, based on the specific clinical situation, but the following regimen is considered optimal:
- after removal of large adenomas on legs and narrowed bases: in the first year - every 6 months, subsequently - once a year;
- after removal of large wide-based adenomas and tubular adenomas with dysplasia (regardless of their macroscopic properties): in the first year - once every 3 months, in the second year - once every 6 months, thereafter - once a year.
Tubular adenoma of the colon is a benign neoplasm that can be the source of a malignant neoplasm - colon cancer. Therefore, in no case should one be dismissive of this pathology. Euroonko has all the capabilities to conduct comprehensive diagnostics, professional removal of adenomas and follow-up with highly qualified specialists.
Book a consultation 24 hours a day
+7+7+78
Treatment
Intestinal neoplasms must be removed, regardless of whether they are malignant or benign.
If the neoplasia is small, it is removed during colonoscopy, and the resulting material is sent for morphological examination. For malignant intestinal tumors, extensive operations are performed to radically remove the tumor. This may involve resection of a piece of intestine or removal of the intestine (colectomy). In some cases, a colostomy is required - removal of the supra-tumor part of the intestine to the anterior abdominal wall.
For advanced tumors, treatment is supplemented with chemotherapy, and for the proximal intestine with radiation therapy.
Predictive data
The prognosis will be determined by the type of intestinal neoplasia. For example, lipomas and angiosarcomas are not prone to malignancy, but they need to be removed to prevent the development of complications - intestinal obstruction and bleeding. The situation with polyps is different. Polypectomy is recommended because there is a risk of malignant degeneration. The greatest risk of malignancy is observed in the following cases:
- Villous polyps.
- Polyps more than 1 cm.
- Broad-based polyps.
- Multiple polyposis.
The prognosis for colon cancer is determined by the stage of the disease. In the initial stages, the prognosis is favorable, there is a chance of complete recovery, the 5-year survival rate reaches 90%. At the second stage - 50-70%, at the third - 50%, and with the metastatic form of cancer, only 10% of patients survive the five-year mark.