There is not a single person who does not complain about the appearance of spasms in the gastrointestinal tract, muscle pain or headache. To reduce pain of various kinds, pharmacists have developed many different drugs. One such medicine that is used for pain relief, prevention and treatment of pain caused by spasms is no-spa. Its main component is drotaverine. It affects the smooth muscles of the biliary tract, genitourinary system and gastrointestinal tract, while reducing pain and relieving spasms.
What is No-shpa?
No-spa is a myotropic antispasmodic drug. Its main active ingredient is drotaverine hydrochloride, which is similar in its chemical structure and medicinal properties to papaverine, but has a stronger and longer-lasting effect.
Drotaverine reduces the tone of the smooth muscles of the gastrointestinal tract, biliary tract, urinary and reproductive systems, and consequently leads to pain relief. It also promotes vasodilation, thereby improving blood flow to tissues.
No-shpa - a classic of antispasmodic therapy
Introduction
Abdominal pain, or abdominal pain, usually reflects a pathological process in the abdominal cavity. In its duration it can be acute or chronic. Based on the mechanisms of occurrence, the following types of abdominal pain can be distinguished :
Abdominal pain, or abdominal pain, usually reflects a pathological process in the abdominal cavity. In its duration it can be acute or chronic. Based on the mechanisms of occurrence, the following can be distinguished:
- spastic
(arising from spasms of the smooth muscles of the gastrointestinal tract), - distensional
(arising from stretching of the hollow organs of the abdominal cavity), - peritoneal
(associated with a pathological process in the peritoneum), - vascular
(associated with ischemia of the abdominal organs).
Thus, with diseases of the esophagus, stomach, and duodenum, pain is observed in the epigastric region. However, with myocardial infarction, lower lobe pneumonia, pleurisy, acute pyelonephritis, similar localization of pain may be observed.
In diseases of the biliary tract, gallbladder and liver, pain is most often noted in the right hypochondrium; with pancreatitis - often localized in the left hypochondrium (it should be remembered that pain in the right or left hypochondrium also accompanies lower lobe pleuropneumonia, renal colic, splenic infarction).
Pain in the umbilical area
are characteristic of diseases of the small intestine, and may also be associated with vascular damage, for example, an abdominal aortic aneurysm or a disorder of the mesenteric circulation.
Pain in the right iliac region
usually associated with disease of the cecum and appendix. Such pain can also accompany pathology of the ureter.
Pain in the left iliac region
, as a rule, are caused by pathology of the sigmoid colon, often by diverticulitis.
Pain in the suprapubic region
in most cases they are caused by pathological processes in the bladder, uterus and its appendages.
In addition to eliminating pain, relaxing the spasm is very important. Spasm
– pathological or physiological contraction of individual muscles or muscle groups (and sometimes many muscle groups) is an accompanying symptom of many diseases. It impairs the blood supply to the affected area, and in itself can be the beginning of the development of a pathological condition.
As is known, the state of the contractile apparatus of a muscle cell is directly dependent on the concentration of calcium ions in the cytoplasm. The latter, interacting with the cytoplasmic calcium-binding protein calmodulin, activate myosin light chain kinase. The kinase cleaves the phosphorus residue from the adenosine triphosphate molecule associated with the fibers of the myosin motor protein. Thanks to this, myosin acquires the ability to interact with another motor protein, actin. Active “molecular” bridges are established between actin and myosin, due to which actin and myosin “move” relative to each other, which leads to cell shortening.
Molecules of cyclic adenosine monophosphate (cAMP) and cyclic guanosine monophosphate (cGMP) reduce the content of calcium ions in the cytoplasm and thereby contribute to a decrease in the contractile activity of the cell.
Cyclic forms of AMP and GMP are formed from inactive monophosphates. The enzyme phosphodiesterase catalyzes the breakdown of cyclic AMP and GMP to inactive forms. Thus, one of the necessary conditions for muscle fiber contraction is high phosphodiesterase activity; for relaxation, on the contrary, its low activity is needed.
What are the possibilities for therapeutic relief and prevention of attacks of abdominal pain?
Today, the following groups of drugs are used: nitrates, anticholinergics, calcium antagonists, b-agonists used in the treatment of bronchial asthma and myotropic antispasmodics - the most effective group for abdominal pain caused by spasm.
The main range of uses of antispasmodics
in everyday practice:
- Symptomatic treatment if spasm is a characteristic accompanying symptom of the disease, but does not play a role in pathogenesis.
- The antispasmodic is used as a means of etiotropic therapy if spasm underlies the pathological condition.
- Antispasmodics are used as premedication in preparing patients for various procedures, for example, ureteral catheterization, etc.
Mechanism of action of antispasmodics
Depending on the mechanisms of action, antispasmodics are divided into two groups: neurotropic and myotropic.
Neurotropic antispasmodics
act by disrupting the transmission of nerve impulses in the autonomic ganglia or nerve endings that stimulate smooth muscles.
Myotropic antispasmodics
reduce muscle tone due to a direct effect on biochemical intracellular processes.
The most important neurotropic antispasmodics are M-anticholinergic blockers.
M-anticholinergic agents (atropine-like drugs) have an antispasmodic effect in the upper gastrointestinal tract (GIT): they are 3–10 times more effective on the stomach than on the colon. Firstly, this is due to the unequal distribution density of M-cholinergic receptors in the gastrointestinal tract (the largest number of them is located in the stomach). Next in descending order are the colon, rectum, cecum, jejunum and duodenum. Secondly, the tone of the colon wall is regulated by the sacral parasympathetic nerve, which is resistant to the action of anticholinergic drugs. In addition, only 20–40% of contractions of the muscles of the colon are carried out through M-cholinergic receptors. Most contractions are activated by noncholinergic transmitters. This explains the limited effectiveness of anticholinergic drugs for spastic phenomena in the lower gastrointestinal tract.
Side effects of M-anticholinergics include a decrease in the secretion of various exocrine glands (salivary, mucous, sweat), HCl in the stomach, an increase in heart rate, mydriasis, paralysis of accommodation and an increase in intraocular pressure.
M-anticholinergic drugs according to their chemical structure are divided into tertiary, penetrating the blood-brain barrier and having a central effect (atropine, scopolamine, platyphylline), and quaternary ammonium compounds that do not penetrate the blood-brain barrier (methacin, chlorosyl).
The number of side effects and low antispasmodic activity make the use of atropine-like drugs very limited.
The first truly effective myotropic antispasmodic drugs were opium extracts. The further development of their use was driven by the knowledge that among opium alkaloids, papaverine is the drug that has the most pronounced antispasmodic effect on smooth muscles and the least effect on the central nervous system. Production of the drug in industrial quantities in the form of hydrochloric acid salt was carried out in 1930 at. In 1931, by replacing the methoxy groups of papaverine with ethoxy radicals, the drug perparin was developed with a stronger antispasmodic effect than papaverine, but less absorbable. Research continued with the goal of obtaining a more effective myotropic antispasmodic than papaverine, and, if possible, without side effects. Finally, in 1961, Meszaros, Szentmiklosi and Czibula developed hydrogenated derivatives of papaverine, namely drotaverine
, which received the trade name
“No-shpa”
. All pharmacological and clinical studies have proven the higher effectiveness of drotaverine in comparison with papaverine.
Myotropic antispasmodics exhibit a certain tropism for individual smooth muscle organs. Among them are bronchodilators, vasodilators, and gastrointestinal antispasmodics. They reduce the tone of smooth muscle cells by directly influencing biochemical intracellular processes, either leading to an increase in intracellular cAMP or a decrease in intracellular cGMP. cAMP activates the release of Ca2+ ions from the cell and its deposition, which leads to a decrease in cell contractility. cGMP, on the contrary, increases the contractility of smooth muscle cells due to stimulation of the release of Ca2+ ions from intracellular stores.
Antispasmodics with myotropic action also include calcium antagonists.
The muscle cell of the intestinal wall carries out its contractility with the help of Ca2+ ions. There are two possible ways for Ca2+ ions to enter the cell:
entry of Ca2+ from the extracellular space through slow voltage-dependent Ca2+ channels of membranes and release of Ca2+ from intracellular stores through receptor-dependent Ca2+ channels. There are two types of contractions of intestinal smooth muscles: tonic and phasic. Tonic contractions maintain the basal tone of the intestinal wall and sphincters during fasting; phasic contractions are rhythmic contractions of the intestinal wall that provide propulsive movement of food through the intestines. The mechanism of development of tonic and phasic contractions depends on different levels of Ca2+ ions entering the cells. The entry of Ca2+ ions into the cell through Ca2+ channels causes tonic contraction; mobilization of Ca2+ under the influence of neurotransmitters (acetylcholine, catecholamines) from dense Ca2+ stores, for example, the sarcoplasmic reticulum, leads to phasic contraction. The number of intracellular depots in the gastrointestinal tract varies: most of them are localized in the smooth muscles of the colon, least of all in the duodenum and small intestine.
The action of calcium antagonists is associated with blocking slow voltage-dependent Ca2+ channels in the smooth muscles of the gastrointestinal tract. These drugs have little effect on receptor-dependent Ca2+ channels and cannot block the release of Ca2+ from the depot, therefore they have an antispasmodic effect mainly in the upper gastrointestinal tract.
Mechanism of action of drotaverine
Phosphodiesterase inhibition
Phosphodiesterase inhibition
Adenosine 3'-5'-cyclomonophosphate (cAMP) and guanosine 3'-5'-cyclomonophosphate (cGMP) play an important role in the regulation of smooth muscle cell tone. An increase in the concentration of these substances is directly related to muscle relaxation.
The intracellular concentration of cyclic nucleotides is determined by the relative rate of their formation with the help of agonist-induced stimulation of adenylate cyclase (agonist - norepinephrine) and guanylate cyclase (agonist - acetylcholine), as well as the rate of their hydrolysis by cell phosphodiesterase enzymes (PDE).
cAMP and cGMP are synthesized from the corresponding nucleoside triphosphates using the membrane-bound enzymes adenylate cyclase and guanylate cyclase, respectively, cAMP and cGMP are inactivated by PDE to inactive non-cyclic ribose phosphates.
The adenylate cyclase system is universal, and cAMP and cGMP are the most important intracellular second messengers for smooth muscle cells of various organs (smooth muscles of the gastrointestinal tract, trachea, bronchi, uterus, ureters, blood vessels, myocardium), as well as for cells of other tissues (platelets, lymphocytes, secretory cells , CNS, etc.). The system provides various functions (muscle tone, secretion, aggregation, etc.). The wide range of functions of the adenylate cyclase system is ensured by the existence of numerous PDE isoenzymes in various types of tissues (tissue-specific and species-specific). PDE isoenzymes differ in physical and kinetic characteristics, substrate (cAMP or cGMP) specificity, sensitivity to endogenous activators and inhibitors, sensitivity to phosphorylation by protein kinases, tissue distribution and cellular localization. Thus, differences in the intracellular distribution of PDE isoenzymes are an important factor determining their individual regulatory role. According to a series of experimental studies, about 7 different families of PDEs have been established: Ca2+-calmodulin-dependent (PDE I), cGMP-stimulated (PDE II), c-GMP-inhibited (PDE III), cAMP-specific (PDE IV), cGMP- specific (PDE V), photospecific (PDE VI), high-affinity (resistant) (PDE VII).
Thus, PDE plays a major role in the regulation of smooth muscle tone
and represents a convenient cellular target for drug development.
PDE isolated from various tissues contain all isoenzymes, but in different quantities. Experimental studies have established the most significant types of PDE in different tissues and created selective PDE inhibitors. Thus, the selective PDE III inhibitor milrinone, the selective PDE IV inhibitor rolipram, and the selective PDE V inhibitor zaprinast are known. Milrinone is a non-catecholamine inotropic for cardiomyocytes and causes relaxation of vascular smooth muscle; Rolipram, according to initial data, was an inhibitor of brain PDE, and then its effect was shown on PDE IV of the respiratory tract muscles, liver cells, and lymphocytes. Research results have shown that the smooth muscle of the large intestine contains almost all isoforms of PDE, the main one of which is PDE IV.
In smooth muscle cells of the urinary tract, the existence of at least three different isoforms (I, II, IV) has been found, but PDE IV also predominates.
Myometrium during pregnancy contains large doses of PDE IV (50%) and PDE III (10%). PDE IV is found both in the initial period of pregnancy and in the last trimester. It is assumed that PDE IV at the end of pregnancy contributes (through changes in cAMP levels) to the preparation of the myometrium for childbirth. Studies in the isolated uterus have shown that selective PDE IV inhibitors can reduce the sensitivity of the organ to oxytocin and lead to rapid relaxation of the uterus after the application of maximum concentrations of oxytocin. This phenomenon can be used for premature birth.
Drotaverine and its main metabolites (CH 280895 and CH 281095) are strong and selective inhibitors of PDE IV smooth muscle cells. Thanks to the effects of drotaverine, not only an antispasmodic effect is provided, but also swelling and inflammation are reduced, in the pathogenesis of which PDE IV is also involved.
Action as a calcium antagonist
Smooth muscle contraction is a Ca2+-dependent process. The contractile process is initiated by any stimulus that causes an increase in the concentration of Ca2+ ions in the cytosol. Ca2+ ions required for contraction can come from an extracellular source through transmembrane Ca2+ channels, or intracellular cytoplasmic organelles (sarcoplasmic reticulum, mitochondria). Ca2+ channel antagonist drugs inhibit the penetration of Ca2+ ions from the extracellular space, which prevents spasm and promotes relaxation of smooth muscles. This is what determines the value of this class of drugs. This mechanism is especially useful in the treatment of cardiovascular diseases, including cardiac arrhythmia, angina pectoris, and hypertension.
Another class of Ca2+ antagonists are drugs that interact with calmodulin, a cytoplasmic Ca2+-modulating protein. Calmodulin functions as a necessary mediator of the action of Ca2+ ions in Ca2+-dependent intracellular processes: with an increase in the concentration of Ca2+ ions in a stimulated cell, calmodulin binds them, which leads to a conformational change in the calmodulin molecule, and it acquires the ability to bind to the actin-myosin contractile system.
Calmodulin antagonists prevent the formation of the active Ca2+–calmodulin complex and thus inactivate the enzyme. In addition, calmodulin antagonists are able to inhibit calmodulin-dependent PDEs, some of which affect the function of Ca2+ channels. Drotaverine and papaverine have virtually no effect on calmodulin-dependent type I PDEs. According to experimental studies, drotaverine has weak activity as a calmodulin antagonist and significant activity as a Ca2+ antagonist. Papaverine is 5 times stronger than drotaverine as a calmodulin antagonist, and does not exhibit the properties of a Ca2+ antagonist. Due to its special properties, drotaverine is classified, according to the classification of Ca2+ antagonists, in group III - calmodulin antagonists.
Sodium channel blocking effect
Sodium channels play a fundamental role in the generation and conduction of electrical stimuli and may be involved in the pathogenesis of many diseases. Binding sites for drugs have been identified on sodium channels. Na+ channel blockers are widely used as antiarrhythmics, antiepileptics and local anesthetics. Experimental studies have shown that drotaverine has an affinity for Na+ channels; its activity towards Na+ channels is 10 times higher than towards Ca2+ channels.
Drotaverine is an effective antispasmodic drug without cardiovascular effect
. PDE is an enzyme that hydrolyzes cAMP in cardiomyocytes and vascular smooth muscle cells, represented predominantly by type III PDE. cAMP is synthesized through stimulation of b1- and b2-adrenergic receptors, which activate membrane-bound adenylate cyclase. Elevated levels of intracellular cAMP in cardiomyocytes increase intracellular Ca2+ levels through activation of protein kinase, which phosphorylates proteins in the sarcolemma and sarcoplasmic reticulum. During the period of depolarization, Ca2+ channels open, through which Ca2+ enters the cell and activates contractile proteins. Intracellular cAMP is metabolized by PDE III, and inhibition of this enzyme increases the level of cAMP, which leads to an increase in intracellular Ca2+ concentration. An increase in intracellular Ca2+ concentration in myocardiocytes causes a positive inotropic effect. Elevated levels of intracellular cAMP and Ca2+ may also cause electrophysiological effects. Vascular smooth muscle cells also contain PDE III; inhibition of this enzyme and the resulting increase in cAMP levels causes relaxation of the smooth muscle cells of the vascular wall. This is achieved by depositing Ca2+ ions in the sarcoplasmic reticulum.
PDE III inhibitors may cause arrhythmias that occur due to an increase in intracellular cAMP levels and, consequently, an increase in Ca2+ levels in cardiomyocytes. Not only PDE III inhibitors, but also PDE V inhibitors have a pronounced cardiovascular effect.
Since drotaverine is a selective inhibitor of PDE IV and an antagonist of the action of Ca2+, its cardiovascular effect is weakly expressed.
Pharmacokinetics of drotaverine
Absorption
The peak concentration of drotaverine in plasma occurs between 45 and 60 minutes after administration, which characterizes it as a rapidly absorbed drug. After a single oral dose of 80 mg of drotaverine hydrochloride, the maximum plasma concentration of the parent compound (136–320 ng/ml) is achieved after 2 hours. The bioavailability of drotaverine when taken orally is 60%.
Drotaverine binds to plasma proteins (95–98%), especially albumin, b- and g-fractions of globulins and a-lipoproteins.
The drug penetrates well into various tissues: the central nervous system, adipose tissue, myocardium, lungs, kidneys, liver, walls of the urinary and gallbladder, intestines, vascular wall.
Removal
The half-life is 16 hours. About 60% of drotaverine when taken orally is excreted through the gastrointestinal tract and up to 25% in the urine.
Metabolism
The main metabolic pathway of drotaverine is oxidation. The drug is metabolized almost completely to monophenolic compounds. Its metabolites are rapidly conjugated with glucuronic acid.
Application of drotaverine
Many of the symptoms encountered by therapists and gastroenterologists are explained by a disorder of contraction of the smooth muscles of the gastrointestinal tract. Symptoms of spastic gastrointestinal dysfunction occur in almost 30% of healthy people. The majority of patients seeking consultation with a doctor suffer from various functional gastrointestinal disorders. First of all, these are non-ulcer dyspepsia and irritable bowel syndrome. Understanding the pathophysiology of visceral spasm may facilitate rational treatment approaches. Drotaverine is effective in the treatment of various gastrointestinal diseases characterized by spasm of smooth muscles.
Dosage forms of drotaverine (No-shpy)
1 ampoule of No-shpa (2 ml) contains 40 mg of drotaverine
1 tablet of No-shpa contains 40 mg of drotaverine
1 tablet of No-shpa forte contains 80 mg of drotaverine
Esophageal smooth muscle spasm
The main symptoms associated with spastic esophageal dysfunction are dysphagia and chest pain
.
Dysphagia is a feeling of slowness or obstruction in the movement of food through the pharynx and esophagus into the stomach.
Functional dysphagia develops due to impaired swallowing and decreased peristaltic activity of the esophagus due to pathology of its striated and smooth muscles. The most significant diseases of this group are achalasia, diffuse esophageal spasm and gastroesophageal reflux.
Chest pain in gastrointestinal diseases is spastic in nature, highly intense, localized in the middle third of the sternum and often radiates to the anterior surface of the chest. Such pain occurs with hypermotor dyskinesia of the thoracic esophagus (esophagospasm) and is a consequence of a violation of the peristaltic function of the smooth muscles of its wall. Pain can appear during eating or at any other time.
To treat dysphagia and pain associated with spastic dysfunction of the esophagus, nitrates, anticholinergic drugs, antispasmodics from the group of phosphodiesterase inhibitors and calcium antagonists (drotaverine) are used. They lead to a decrease in pressure in the esophagus. However, no drug alone provides complete effectiveness in the treatment of spastic disorders of the esophagus.
Non-ulcer dyspepsia
The term “non-ulcer dyspepsia” refers to a symptom complex that includes complaints of pain in the epigastric region, a feeling of heaviness and fullness in the epigastrium after eating, early satiety, nausea and vomiting, belching of air, heartburn, regurgitation, etc. Synonyms of this term are functional, idiopathic, inorganic dyspepsia. During a thorough examination, it is not possible to identify any organic disease (peptic ulcer, reflux esophagitis, stomach cancer, etc.). The prevalence of dyspeptic complaints among the population is very high - from 19 to 41% according to different authors, while from a third to half of all cases of dyspeptic disorders account for functional dyspepsia.
Depending on the main clinical symptoms, there are four types of non-ulcer dyspepsia:
ulcer-like, reflux-like, dyskinetic and nonspecific.
The leading place in the pathogenesis of non-ulcer dyspepsia is given to motility disorders of the upper gastrointestinal tract.
Treatment of patients includes a healthy lifestyle, prevention of infection with Helicobacter pyloricus, the use of antacids and antispasmodics for ulcer-like variants (especially when pylorospasm and hypermotor dyskinesia of the duodenum are detected). For reflux-like and dyskinetic variants, prokinetics are used.
Sphincter of Oddi dysfunction
Many other terms have been used to describe this functional biliary disorder: biliary dyskinesia, hypertensive sphincter of Oddi dyskinesia, spasm of the sphincter of Oddi, papillary dysfunction.
Disorders and the mechanism of development of pain with dysfunction of the sphincter of Oddi is the development of spasm of sphincter muscle fibers and increased pressure in the bile and/or pancreatic duct system.
The fact that dysfunction of the sphincter of Oddi most often manifests itself in patients with a removed gallbladder serves as indirect confirmation that the gallbladder serves as a reservoir that “quenches” excessive pressure surges throughout the biliary tract. After removal of the gallbladder, even a moderate contraction of the sphincter of Oddi can lead to a significant increase in pressure in the entire biliary tract and, as a result, pain may appear, as confirmed in experiments with the administration of morphine, which increases pressure in the biliary tract.
The factors that cause prolonged spasms of the sphincter of Oddi are unknown.
For therapeutic purposes, myotropic antispasmodics are most often used in practice, having a targeted effect on smooth myocytes of the gastrointestinal tract.
The main representatives of this group of drugs are drotaverine (No-shpa, No-shpa forte), otilonium bromide, etc. These drugs are used short-term (from a single dose to two to three weeks) to relieve spasm, and therefore pain.
In a double-blind, placebo-controlled clinical trial, the effectiveness of No-shpa was studied in patients with sphincter of Oddi stenosis as an adjuvant, including in patients with surgical interventions. The use of No-shpa showed a significant significant reduction in pain in 60% of patients and a small effect in another 23%
, while placebo in 55% of cases did not affect the intensity of pain. In this study, No-shpa was 2 times more effective than analgesics.
In addition, in a pilot study it was found that the use of No-shpa reduces AST activity by 15–60% in patients with diseases of the biliary system
.
The results of these studies showed that No-shpa is the drug of choice for spasms of the smooth muscles of the biliary system. No-shpa can be used both in monotherapy and in combination with antibiotics and surgical treatment methods.
Irritable bowel syndrome
Symptoms of hypertensive lower gastrointestinal motility disorder include constipation, with or without lower abdominal pain. Most often, patients with such symptoms are diagnosed with irritable bowel syndrome and chronic constipation.
Irritable bowel syndrome (IBS) is a common clinical problem encountered by emergency physicians and gastroenterologists. IBS is one of the manifestations of functional disorders of the gastrointestinal tract, in which the colon is predominantly involved in the pathological process. IBS is characterized mainly by disturbances in the motor and secretory function of the colon without morphological changes in the mucous membrane.
Epidemiological studies indicate a high incidence of the disease in the general population: 14–24% of women and 5–19% of men. IBS is a biopsychosocial disorder in which abnormalities in psychoemotional order, motor skills and sensitivity lead to abdominal pain and defecation disorders. To evaluate symptoms, a unified set of criteria, the Rome Diagnostic Criteria, is used.
Principles of IBS treatment
include normalization of the diet and nature of nutrition, normalization of the psycho-emotional sphere, correction of movement disorders of the colon. In case of IBS, which occurs predominantly with pain, the optimal prescription should be considered drugs that have an antispasmodic effect (drotaverine, pinaverium bromide, butylscopolamine).
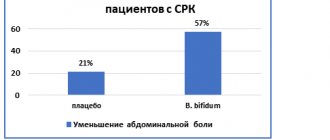
Several clinical studies have been conducted to evaluate the effectiveness and tolerability of No-shpa in patients with irritable bowel syndrome and other intestinal disorders.
A double-blind, randomized, placebo-controlled study included 62 patients (age 50.8±14.2 years) with IBS and constipation. Patients recorded their complaints daily for 2 weeks before the start of treatment and during 8 weeks of treatment with No-shpa 80 mg 3 times a day or 2 placebo tablets 3 times a day. Active treatment significantly reduced abdominal pain by 47%, while in the placebo group pain increased by 3% (p < 0.05). While taking No-shpa, other symptoms, including flatulence, also decreased.
In another randomized, double-blind study, the effectiveness of No-shpa was studied in 70 patients aged 18–60 years diagnosed with IBS according to their own criteria. Patients received No-shpa 80 mg 3 times a day for 4 weeks, and then were observed for another 4 weeks. The results showed that No-shpa significantly reduces the incidence of pain compared to placebo – by 47% (p<0.001) (Fig. 1), flatulence by 21% (Fig. 2) and dyspepsia – by 20% (p<0.001) (Fig. 3). At the same time, normalization of stool frequency occurred in 40% of patients receiving No-shpa and placebo, but an improvement in passage time in the colon was noted significantly more often with the use of No-shpa (Fig. 4 and 5).
Rice. 1. Frequency of abdominal pain syndrome while taking No-shpa and placebo
Rice. 2. Frequency of flatulence while taking No-shpa and placebo
Rice. 3. Frequency of dyspepsia while taking No-shpa and placebo
Rice. 4. Frequency of constipation while taking No-shpa and placebo
Rice.
5. Change in passage time in the colon while taking No-shpa and placebo Chronic constipation
Constipation is a very common complaint. Constipation can be caused by a variety of factors affecting smooth or striated muscle, impairing the function of autonomic or somatic nerves, or factors associated with changes in colorectal anatomy or intestinal contents.
Constipation is a very common complaint. Constipation can be caused by a variety of factors affecting smooth or striated muscle, impairing the function of autonomic or somatic nerves, or factors associated with changes in colorectal anatomy or intestinal contents.
Among the diseases that cause secondary constipation are systemic endocrine and metabolic diseases, disorders and diseases of the central nervous system (damage to the spinal cord, peripheral nerves), as well as myopathy and muscular dystrophy. Constipation can be caused by a number of drugs belonging to different groups, including drugs that interact with neurons of the central nervous system (eg, opiates), drugs that directly affect smooth muscle (calcium antagonists), and drugs that alter the contents of the intestines (cholestyramine). Habitual consumption of low-fiber foods can lead to infrequent bowel movements and complaints of constipation.
In the treatment of constipation, a diet with a high content of fiber and cellulose, various laxatives and medications that improve the neuromuscular regulation of motor function of the colon (prokinetics) or antispasmodics are used. Drugs that activate intestinal motility, in combination with antispasmodics, help avoid the use of toxic laxatives.
Conclusion
Pain is a universal symptom for a wide variety of lesions of the gastrointestinal tract; its occurrence is often based on spasm of the smooth muscles of the abdominal organs. Of the entire group of antispasmodic drugs, the most popular today is drotaverine (No-shpa)
.
A review of the results of clinical studies shows that No-shpa is an effective drug for the rapid relief of spasms and pain. For a quick onset of effect, the first administration of No-shpa should be intravenous or intramuscular; for long-term treatment, it should be administered orally. Literature:
1. Belousov Yu. B. Antispasmodics. Pharm. Bulletin, 36 (235, 2001).
2. Belousov Yu. B., Leonova M. V. Clinical pharmacology of no-shpa. Methodological manual for doctors. M., 2002.
3. “Gastroenterology” Directory. P/r V. T. Ivashkin and S. I. Rappoport. M., Russian doctor, 1998, pp. 84–90
4. Grigoriev P. Ya., Yakovenko E. P., Pryanishnikova A. S. et al. The place of the drug No-shpa forte in the management of patients with abdominal pain syndrome. Practitioner, 16 (3, 1999), pp.39–40
5. Ivashkin V. T., Shulpekova Yu. O., Drapkina O. M. Abdominal pain syndrome. Submitted for publication in the Russian Journal of Gastroenterology, Hepatology and Coloproctology.
6. Leonova M.V., Shishkina T.I., Belousov Yu.B. New dosage form No-shpa forte in clinical practice.
7. Akos Pap MD The management of smooth muscle spasm. Budapest, 1998, 266 p.
8. Blasko G. Pharmacology, mechanism of action and clinical significance of a convenient antispasmodic agent: drotaverine. JAMA India – The physician's update, 1998, v.1, N 6, p.63–70.
9. Kapui Z., Bence J., Boronkay E. et al. Behavioral effects of selective PDE4 inhibitors in relation to inhibition of catalytic activity and competition for [3H]rolipram binding. Neurobiology, 1999, v.7, N 1, p.71–73.
What do you need to know before you start taking No-shpa?
Despite the fact that No-shpa is a fairly safe drug, its use is still contraindicated for people with the following conditions:
- severe kidney, liver and heart failure;
- low blood pressure;
- patients who are allergic to drotaverine;
- women who are breastfeeding;
- children whose age is less than 1 year.
Before using No-shpa, consult your family doctor.
No-Spa does not affect the reaction speed, but if you feel dizziness or other side effects, then do not drive or use complex mechanisms and devices.
Note!
If you suffer from lactose intolerance, then consult your doctor before using No-Spa, because each tablet contains 52 mg of lactose.
Characteristics of the medicine
The main component in the warehouse is considered to be drotaverine hydrochloride. It affects the smooth muscles of the digestive organs, spasms stop, severe pain disappears, and the muscles relax. Drotaverine helps dilate blood vessels so that enough oxygen enters the cells.
The drug is approved for use by pregnant women, practically does not penetrate the placenta, and does not pose a risk to the health of the child (of course, subject to the doctor’s prescriptions and taking into account the risk for the expectant mother and baby). When breastfeeding, taking No-shpa is contraindicated; no studies have been conducted in this direction.
The medicine is used for therapeutic and prophylactic purposes.
Stock:
- In the form of tablets. The medicine looks like small, round, yellowish tablets. Contains 40 milligrams of the main component - drotaverine hydrochloride and a number of additional components - talc, starch, magnesium stearate, lactose, povilone.
- In the form of injections. The ampoule contains 2 milligrams of a transparent, yellow-green solution. Includes 40 milligrams of drotaverine, 96% ethanol, sodium disulfite and water for injection.
Side effects
Like any medicine, No-shpa has side effects. Highlight:
- allergic reactions to individual components (itching, rash, swelling);
- disruptions of the heart and blood vessels (jumps in blood pressure, rapid heartbeat);
- poor sleep, dizziness;
- sweating;
- feeling of heat;
- disruptions in the functioning of the digestive system (constipation, nausea).
Negative reactions as a result of taking an antispasmodic are extremely rare. If it develops, you should stop taking it and consult a doctor.
Directions for use and dosage No-shpa
No-spa tablets are taken orally (orally).
If you have difficulty swallowing a whole tablet, you can break it along the score line and take the tablet in small portions to make it easier to swallow.
Dosage:
- for adults - recommended 120-240 mg per day in 2-3 doses;
- for children over 12 years old - maximum 160 mg in 2-4 doses;
- for children from 6 to 12 years old - maximum 80 mg in 2 doses.
Note!
The effect on children has not been studied in a clinical setting, so give the drug to a child with caution, as this may affect his health.
When using the drug without consulting a doctor, it is recommended to take No-spa for 1-2 days. With auxiliary therapy 2-3 days. Contact your doctor if the pain does not improve.
Solution for injection is used for adults:
- intramuscularly 40-240 mg, divided into 1-3 separate injections;
- intravenously for acute colic (urinary and cholelithiasis) 40-80 mg.
Note!
The dose for children is calculated by the doctor; adjustments for elderly people or those with liver or kidney failure are not required.
Release forms and price category
No-spa is available in the form of tablets, as well as in ampoules for intramuscular and intravenous administration. The dosage of one tablet is 40 mg of drotaverine hydrochloride. The tablets have a yellowish-greenish color and are bitter to taste. On one side there is a marking with the inscription “spa”. There are blisters of 6 and 24 pieces. For larger quantities, bottles with stoppers are used, which have 60, 64, 100 pieces. Ampoules are available in two milliliters. The amount of drotaverine per 1 ml of solution is 20 mg; only 2 ml of solution contains 40 mg of drotaverine hydrochloride. The ampoules are made of dark glass and have a marked break point for ease of opening.
No-spa is available in the form of tablets and ampoules.
The drug is affordable. It all depends on the manufacturer, but in any case, no-silo can be classified as a budget drug.
Symptoms and consequences of an overdose of No-shpa
Too large a dose of the drug can cause the following overdose symptoms :
- weakness;
- malaise;
- dizziness;
- vomiting;
- headache;
- drop in blood pressure;
- drowsiness;
- disturbances of heart rhythm and conduction.
Note!
Cardiac arrest has also been reported after an overdose of No-shpa.
In case of accidental or intentional overdose, consult a doctor immediately.
No-spa as an effective antispasmodic
No-shpa will be an option for treating the disease. It acts specifically on the source of pain. The drug is available in two versions - tablets and injection. No-spa today is an effective and relatively inexpensive antispasmodic. It is permissible to take the drug only after a doctor’s prescription. The doctor determines the desired form and dosage. The big plus of No-shpa is its quick effect, which occurs in a couple of minutes.
No-spa for gastritis is used during the acute period of the disease. An antispasmodic is often an additional medicine that quickly relieves painful spasms, but it cannot be treated constantly.
Interaction of No-shpa with other drugs and substances
Tell your doctor if you are taking, have recently taken, or are about to take any other medications, as the medications may be incompatible with each other.
In case of simultaneous use with other medications taken for a long time, seek advice from your doctor before taking No-shpa.
No-spa interacts with the following medications:
- Levodopa - No-spa can increase muscle tone and tremors);
- antispasmodics (Papaverine, Bendazole) and Phenobarbital - the antispasmodic effect may increase;
- Morphine - its spasmogenic activity may decrease when interacting with No-shpa.
General indications for use
- Spasmodic pain in the digestive organs due to gastritis, ulcers and other diseases.
- Spasms of the ducts of the urinary and gall bladders in diseases of the urinary and reproductive system.
- Spasms of the arteries of the brain.
- Convulsive contractions as a result of operations.
- Severe colic in the intestines.
- The drug is used in gynecology if a threat of miscarriage or sharp pain during childbirth is detected, if during pregnancy there is a feeling of heaviness and aching pain in the lower abdomen.
- Severe throbbing headache and angina.
In case of an overdose of the drug, a disturbance in the activity of the heart is observed. In the latter case, the patient must be in a medical facility under the supervision of a doctor. A number of actions are taken to improve the body’s condition (gastric lavage and appropriate therapy).
No-spa for gastritis is an effective medicine that quickly and permanently relieves pain and muscle spasms of the digestive tract. The antispasmodic is not absorbed into the bloodstream, acting specifically at the site of inflammation. This is an auxiliary, additional remedy, allowed for use for a maximum of 2-3 days. The remedy does not cure the disease, it only eliminates the painful symptoms.
No-shpu for gastritis can be taken with other painkillers (as prescribed by a doctor). This medicine has a wide spectrum of action and is used in the treatment of diseases of various organs and systems: digestive, nervous, cardiovascular, genitourinary. When taking the drug, you must take into account the recommendations and contraindications. You should not take more than the prescribed dose in order to quickly eliminate the pain syndrome, preventing unpredictable consequences (reaching hallucinations, convulsions, uncontrollable desire to urinate). It is better not to self-medicate, but to consult a doctor who will select the most optimal treatment regimen.