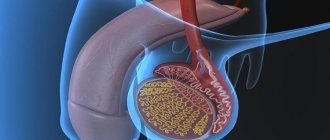
Hemorrhoids are an unpleasant, unbearable disease. Alleviation of suffering becomes the foremost issue for the victim. A proven and inexpensive drug is Diclofenac.
You can relieve inflammation, fever, and pain using Diclofenac anal suppositories for hemorrhoids. Ointment is a form of release of a medicine. Ointment for hemorrhoids Diclofenac, unlike suppositories, is used for external treatment of the disease, or when the use of suppositories is undesirable.
Pharmacology
The product is used to treat chronic and acute hemorrhoids, when you urgently want to relieve pain. Diclofenac's ability to quickly relieve inflammation allows you to get rid of the disease in a short time, when the moment is missed when you have to treat an advanced stage of the disease.
The drug will meet consumer expectations:
- will numb the affected area;
- slow down thrombosis;
- eliminates local allergic reaction;
- will reduce elevated body temperature.
Doctors are often asked about the permissibility of the drug for use in the treatment of hemorrhoids, when the rectal mucosa is damaged or wounded. Professional doctors say: suppositories are used if the anus is intact. The reason lies in the composition of the drug. The substances that make up Diclofenac treat intact membranes, and an irritating effect appears on damaged areas. The patient will feel a strong burning sensation that does not allow holding the candle for a long time.
Prospects and advantages of suppositories with diclofenac: Diclovit
Thus, diclofenac is one of the most powerful non-steroidal anti-inflammatory drugs [6]. In addition, diclofenac also has a very low probability of ulcerogenic effects [4]. Many years of positive experience in the use of diclofenac in different countries, the abundance of available dosage forms, a wide range of acceptable dosages - all this makes it possible to consider diclofenac the drug of first choice for most rheumatic diseases and for the relief of pain of mild and moderate intensity [1].
pharmachologic effect
According to modern concepts, diclofenac has a number of pharmacological effects, the main one of which is inhibition of the activity of the enzyme cyclooxygenase (COX)
, which catalyzes the formation of prostaglandins from arachidonic acid, powerful mediators of the inflammatory process [3].
The existence of two isoenzymes of cyclooxygenase, COX-1 and COX-2, has been established.
COX-1 induces the production of prostaglandins: prostaglandins (which have a cytoprotective effect on the gastric mucosa) and thromboxane A2 (which affects platelet aggregation).
COX-2 is expressed in areas of inflammation and promotes the synthesis of pro-inflammatory prostaglandins. Thus, the anti-inflammatory effect of diclofenac is associated with the suppression of COX-2 activity, and the development of side effects is associated with the suppression of COX-1.
Diclofenac is able to cause uncoupling of oxidative phosphorylation in mitochondria with a decrease in ATP synthesis and a decrease in energy supply to the inflammatory reaction, as well as inhibit lipid peroxidation.
The ability of diclofenac to affect acute exudative inflammation due to
inhibition of COX makes it one of the most powerful NSAIDs used to treat diseases of the musculoskeletal system (rheumatoid arthritis, ankylosing spondylitis, etc.) [1].
Diclofenac suppresses the exudative and proliferative phases of inflammation. This reduces the formation of various prostaglandins and prostacyclins in areas of inflammation and prevents the formation of free radicals from cyclic endoperoxides and the formation of lipid peroxides in cell membranes, which leads to limitation of inflammation.
By limiting exudation, diclofenac prevents blood plasma factors that stimulate guanylate cyclase and cGMP, which activates collagen synthesis by fibroblasts, from entering the tissue. As a result, diclofenac also suppresses the proliferative component of inflammation [7].
Immediate analgesic effect
diclofenac, as well as anti-inflammatory, is mainly due to blocking the synthesis of prostaglandins both in peripheral tissues and in the central nervous system.
The most common cause of chronic pain in old age is osteoarthritis. Due to the fact that inflammatory reactions of the synovium and periarticular tissues play a critical role in the pathogenesis of pain, diclofenac in osteoarthritis in most cases provides a more pronounced analgesic effect than non-narcotic analgesics [1]. The analgesic effect of diclofenac is also associated with a decrease in exudation, a weakening of mechanical pressure on pain receptors in tissues, and the prevention of the development of hyperalgesia [6].
Antipyretic effect
due to inhibition of the synthesis of prostaglandins E1 in the central nervous system and a decrease in its effect on the thermoregulation center. The antipyretic effect of diclofenac can also be explained by its inhibitory effect on the synthesis of endogenous pyrogens with a molecular weight of 10,000–20,000 D in polymorphonuclear neutrophils, monocytes and reticulocytes [6].
Antiplatelet effect
is characteristic of all non-selective COX inhibitors and is associated with inhibition of thromboxane A2 synthesis [1,6].
Desensitizing effect
diclofenac develops slowly. To receive it, the drug must be prescribed for 2 months or more. The following mechanisms are important in the mechanism of occurrence of the desensitizing effect:
1. Inhibition of the synthesis of prostaglandins E2 at the site of inflammation and in leukocytes, as well as a decrease in the chemotactic activity of monocytes.
2. Reduced formation of hydroheptranotrienic acid, which reduces the chemotactic activity of T-lymphocytes, eosinophils and polymorphonuclear neutrophils at the site of inflammation.
3. Inhibition of blast transformation of lymphocytes due to blocking the formation of prostaglandins [6,7].
The numerous physiological functions of prostinoids determine the use of NSAIDs in various fields of medicine, in particular in gynecology. Diclofenac can be successfully used for primary dysmenorrhea. Primary dysmenorrhea is associated with the formation of large amounts of prostaglandins in the uterus and its increased ability to contract, which serves as the basis for treatment with prostaglandin synthesis inhibitors [1,7].
Diclofenac is a short-lived NSAID: the drug's half-life is 1.5–3.5 hours.
However, it must be borne in mind that the kinetic parameters of NSAIDs in blood serum and in synovial fluid are different. In this case, the synovial concentration of long-lived drugs correlates with the serum level, and when taking short-lived drugs it is initially low, but then increases significantly and can exceed the serum concentration. This helps explain the long-lasting clinical effectiveness of short-lived drugs [3].
Diclofenac has a high degree of absorption and bioavailability. Up to 99% of the drug is metabolized in the liver. 75% of diclofenac is excreted through the kidneys.
Thus, diclofenac is indicated as a pathogenetic or symptomatic agent:
1) with inflammation of various origins;
2) to relieve pain of mild or moderate severity of various origins;
3) to reduce elevated body temperature (if necessary) [6].
Advantages of Diclovit
The dosage form of diclofenac in the form of suppositories has a number of advantages:
- Suppositories do not cause the complications that are possible with parenteral administration of drugs.
NSAIDs (primarily diclofenac, ketorolac) are characterized by long-term use of muscle necrosis at the injection site. Long-term (more than 2-3 days) parenteral use is fraught with the development of infiltrates and suppuration. - Of no small importance, especially for elderly patients, is to reduce the number of drug doses per day. Very often, suppositories are used in combination therapy: during the day the patient receives either injections or tablets, and at night - suppositories, which creates a better therapeutic effect due to a more uniform and long-term maintenance of the concentration of the drug in the blood.
- It is advisable to prescribe suppositories if it is impossible to take medications by mouth.
- When taken orally, there is a direct damaging effect of diclofenac on the cells of the gastric mucosa with damage to mitochondria and uncoupling of oxidative phosphorylation. That is why, in the presence of signs of damage to the stomach and duodenum, preference is given to suppository forms of diclofenac [1,5,8].
The clinical effectiveness and safety of suppositories with diclofenac are confirmed by the results of clinical trials.
In studies conducted at the Department of Propaedeutics of Internal Diseases of Moscow State Medical University named after. ON THE. Semashko suppositories with diclofenac (ortofen) were used in patients with a wide range of arthrological diseases (Fig. 1).
Rice. 1. Diseases for which clinical trials of suppositories with diclofenac were conducted
During treatment, the indicators of ESR, C-reactive protein, and blood seromucoids significantly decreased (Table 2).
The high therapeutic effectiveness of the drug was also demonstrated in studies conducted at the Institute of Rheumatology of the Russian Academy of Medical Sciences (Moscow).
The identified analgesic and anti-inflammatory effect of suppositories with diclofenac had a positive effect on joint function: exudative manifestations in the joints, the duration of morning stiffness, the severity of pain decreased or disappeared, the range of motion in the joints increased, the number of affected joints and the degree of their functional insufficiency decreased (Fig. 2) .
Rice. 2. Dynamics of articular syndrome during treatment with diclofenac suppositories
In a study of the effectiveness and safety of suppositories with diclofenac, conducted at the Main Military Clinical Hospital. Burdenko, it is shown that the duration of action of suppositories with diclofenac is longer than the duration of action of the tablet form.
Indications
- Inflammatory and degenerative joint diseases - rheumatoid arthritis, ankylosing spondylitis (ankylosing spondylitis), Reiter's disease, osteoarthritis, psoriatic arthritis, gout.
- Rheumatic lesions of soft tissues - bursitis, tendovaginitis, synovitis.
- Diseases of the nervous system – glenohumeral periarthritis, lumbago, lumbodynia, neuralgia, myalgia.
- Gynecological diseases – primary dysmenorrhea, adnexitis, perimetritis.
- Febrile conditions in infectious and inflammatory diseases of the ENT organs.
- Inflammation, pain, trismus, swelling due to dental, orthopedic, gynecological and other surgical interventions.
Directions for use and dosage regimen
Having freed the suppository from the contour packaging, it is introduced into the rectum after an enema or spontaneous bowel movement. After administration, you should stay in bed for 20–30 minutes. Use 1 suppository 2 times a day. The maximum daily dose is 150 mg per day.
The duration of treatment is determined by the doctor depending on the severity of the disease.
Side effect
The drug is usually well tolerated and rarely causes side effects.
However, dyspepsia, diarrhea, heaviness in the epigastrium, drowsiness, headaches and slight dizziness are possible (especially at the beginning of treatment). These phenomena usually go away on their own. In rare cases, a local irritant effect on the intestinal mucosa is possible.
Contraindications
Gastric or duodenal ulcer, hemorrhagic colitis, exacerbation of hemorrhoids, hematopoietic disorders of unknown etiology, increased individual sensitivity to diclofenac sodium, acetylsalicylic acid or other NSAIDs, third trimester of pregnancy, children under 15 years of age.
Cautions
Particularly careful medical supervision requires the use of Diclovit suppositories for high blood pressure or heart failure, induced porphyria, systemic erythematous lupus and mixed collagenoses, chronic obstructive respiratory diseases, asthma, hay fever, and in old age.
special instructions
Due to the fact that when using the drug, side effects such as dizziness and fatigue may occur, in some cases the ability to drive a car or other moving objects is impaired. These phenomena intensify when drinking alcohol.
Interaction with other drugs
With the simultaneous use of rectal suppositories "Diclovit" and:
- digoxin
,
phenytoin
or
lithium preparations
- the plasma levels of these drugs may increase; - diuretics
and
antihypertensive drugs
- their effect may be weakened; - potassium-sparing diuretics
- hyperkalemia may occur; - other NSAIDs
or
glucocorticosteroids
- increases the risk of side effects from the gastrointestinal tract; - acetylsalicylic acid
- the concentration of diclofenac in the blood serum decreases; - cyclosporine
- the toxic effect of the latter on the kidneys may increase; - antidiabetic drugs
- hypo- and hyperkalemia may be observed. With this combination of drugs, control of blood sugar levels is necessary; - methotrexate
- within 24 hours before or after taking it - there may be an increase in the concentration of methotrexate and an increase in its toxic effect; - anticoagulants
- regular monitoring of blood clotting is necessary.
Compound
One suppository contains 50 mg of diclofenac and the base – vitepsol.
Release form
Suppositories containing 0.05 g of diclofenac, in 2 contour packages, 5 pieces in a contour package.
Storage conditions
In a dry, cool place, protected from light. List B.
Keep out of the reach of children.
Vacation rules
Dispensed by prescription.
Literature:
1. Karateev D. Non-steroidal anti-inflammatory drugs.//Medical newspaper. No. 82. 1999. pp. 8–9.
2. Zeigarnik M. Cost of long-term treatment with NSAIDs: there is a choice. // Remedium. No. 11, 1999 pp. 58–60.
3. Nasonov E.L. Non-steroidal anti-inflammatory drugs.//Russian Medical Journal. T7.No.8.P.392–396.
4. Kornienko V.V. Antihomotoxic therapy of rheumatic diseases.// Medical Bulletin No. 4. 1996. pp. 12–13.
5. Lawrence D.R., Bennitt P.N. Clinical pharmacology: in 2 volumes – M.: Medicine, 1993. – T.2. – P.583–584.
6. Kukes V.G. Clinical pharmacology: Academic/Scientific. Ed. A.Z. Baichurin. – 2nd ed., revised. and additional – M: GEOTAR Medicine, 1999. – 528С.
7. Karkishchenko N.N. Pharmacological foundations of therapy (manual and reference book for doctors and students). – M.: IMP – Medicine, 1996. – 560 p.
8. Mashkovsky M.D. Medicines in 2 volumes – 13th edition – Kharkov: Torsing, 1997. – Vol.1. – P.320.
Material provided by pharmaceutical
Indications of the drug
Diclofenac is a suppository that has a positive effect in the treatment of a large number of diseases.
Hemorrhoids
Recommendations for therapy
Indications for use:
- overheating of the body;
- arthritis of the vertebral joints (Bechterew's disease);
- chronic inflammatory process in the joints, in patients suffering from psoriasis;
- diseases of soft tissue structures;
- pain in the postoperative period;
- soreness of the head;
- diseases of the ears, pharynx, tonsils;
- diseases associated with gynecological problems.
It is recommended to use Diclofenac for hemorrhoids:
- to relieve inflammation in the rectum;
- with pain in the anal passage;
- in the treatment of hemorrhoids of varying degrees.
Benefits of treatment
Positive aspects of the drug Diclofenac:
- Suppositories are not addictive. There is no need to increase the amount of the drug; the product is used on an ongoing basis without losing effectiveness.
- The product is intended for external use, without making it dangerous and contraindicated for patients with kidney, liver, and gastric diseases.
- Suppositories are administered rectally. Provides an immediate effect on hemorrhoids, absolute safety for the functioning of other organs.
special instructions
Although Diclofenac is a safe drug for hemorrhoids, there are recommendations for the use of the medicine:
- It is permissible to use suppositories provided that the mucous membranes of the rectum are intact.
- It is not advisable to use it over a long period of time; there is a risk of negative side effects.
- The drug is used externally, ingestion will cause poisoning.
- Use the medicine carefully. Contact with the mucous membranes of the eyes or damaged surface will cause irritation and pain.
- There is no confirmed information on the safety of use when carrying a child or breastfeeding. The use of candles is not recommended.
Diclofenac in the treatment of pain syndromes
The connection between pain and inflammation has been known since ancient times. And today, the most common medications for pain relief are drugs that have both anti-inflammatory and analgesic effects - non-steroidal anti-inflammatory drugs (NSAIDs).
History of the creation of diclofenac
The prototype of modern NSAIDs was acetylsalicylic acid, which was first synthesized by the young scientist Felix Hoffman at the end of the 19th century. The chemical structure and properties of acetylsalicylic acid became the guidelines by which new representatives of this class of medications were created (at first they were usually designated as “aspirin-like”). It is not so much the lack of effectiveness as the toxicity of high doses of acetylsalicylic acid that served as a powerful incentive for the development of new, “non-salicylate” NSAIDs. In 1966, during the implementation of a program to develop an anti-inflammatory drug with improved biological properties, more than 200 analogues of 0-aminoacetic acid were synthesized in a research laboratory to create a molecule with the necessary parameters, among which the most interesting results were shown by diclofenac sodium - the sodium salt of 0-[(2 ,6 dichlorophenyl)-amino]-phenyl-acetic acid.
Initially, diclofenac was used mainly in the treatment of rheumatological diseases, where both components are important: a pronounced anti-inflammatory and powerful analgesic effect, but subsequently, the scope of use of diclofenac expanded significantly. Currently, diclofenac is used in surgery, traumatology and sports medicine (for damage to the musculoskeletal system, damage to soft tissues (bruises, sprains), for postoperative pain relief), in neurology (for the treatment of back pain, tunnel syndromes, migraines), in gynecology for dysmenorrhea, adnexitis, in oncology as a means of the first stage of pain relief in the WHO ladder. Intramuscular administration of diclofenac sodium is an effective method of combating renal and hepatic colic. A special dosage form of diclofenac in the form of drops has found application in ophthalmology. General practitioners also prescribe diclofenac for various pain syndromes (Table 1).
Mechanism of action of diclofenac
The anti-pain effect of diclofenac is due to several mechanisms. The main mechanism of action of diclofenac is the suppression of cyclooxygenase (COX), an enzyme that regulates the conversion of arachidonic acid into prostaglandins, mediators of inflammation, pain, and fever [3].
Diclofenac and COX selectivity
In the early 90s of the twentieth century, two isoforms of the COX enzyme were discovered - COX-1 and COX-2. Most of the positive effects of NSAIDs (suppression of inflammation, pain, fever) are associated with inhibition of COX-2, and the development of adverse reactions (mainly in the form of damage to the gastrointestinal tract) is associated with suppression of COX-1 synthesis [4].
However, there are a number of exceptions to this rule. It has been shown that COX-1 may also play a role in the development of the inflammatory process. COX-1, together with COX-2, is produced by the synovium of patients with rheumatoid arthritis (RA) [5]. This is probably due to the lower effectiveness of selective COX-2 in some pain syndromes. Recent studies have found an increased risk of cardiovascular complications with the use of highly selective COX-2 inhibitors [6].
Diclofenac inhibits both COX isoenzymes, mostly COX-2. Inhibition of COX-1 by diclofenac is less compared to ibuprofen and naproxen, and therefore diclofenac is less likely to cause gastrointestinal damage. At the same time, inhibition of COX-1 (albeit less pronounced than that of non-selective NSAIDs) may explain the greater effectiveness of diclofenac compared to selective COX-2 inhibitors (meloxicam, celecoxib) in a situation where COX-1 is also involved in the pathogenesis of the disease ( for example, with RA). Inhibition of COX-2 by diclofenac is less than that of etoricoxib and rofecoxib, which reduces the risk of cardiovascular complications [6]. This balanced effect of diclofenac ensures high therapeutic activity with good tolerability of treatment.
Other mechanisms of the analgesic action of diclofenac
In addition to inhibition of prostaglandins, other mechanisms of action of diclofenac have been identified. An experimental study showed that diclofenac sodium can significantly inhibit the migration of leukocytes to the site of inflammation [7]. To a certain extent, diclofenac sodium can also affect the balance of cytokines, reducing the concentration of interleukin-6 and increasing the content of interleukin-10 [8]. This change in the ratio of these products helps slow down the secretion of anti-inflammatory factors. A decrease in the production of free oxygen radicals, which occurs under the influence of diclofenac sodium, can also help reduce the activity of the inflammatory process and limit its damaging effect on tissue [9].
In addition to pronounced anti-inflammatory activity, diclofenac sodium also has a powerful analgesic potential that is not related to its effect on inflammation [10]. It has a complex effect on various mechanisms of pain perception, providing effective suppression of pain of various etiologies. The drug has both central and peripheral antinociceptive effects.
The central analgesic activity of diclofenac sodium is mediated by opioid receptors, as evidenced by the fact that this effect is blocked by naloxone [11]. It appears to be associated with the effect of diclofenac sodium on tryptophan metabolism. After administration of the drug, the concentration of tryptophan metabolites in the brain, which can reduce the intensity of pain, significantly increases [12].
The local antinociceptive effect of diclofenac sodium appears to be associated not only with the suppression of prostaglandin synthesis, since in several experimental models of pain, local use of prostaglandin synthesis inhibitors such as indomethacin and celecoxib, unlike diclofenac sodium, did not achieve a significant analgesic effect [ 13]. The peripheral analgesic effect of diclofenac sodium is not associated with the opioid effect, since it is not eliminated by naloxone. At the same time, the use of compounds that block the formation of NO and the activation of guanylate cyclase suppressed the analgesic effect of diclofenac sodium. Inhibitors of various types of potassium channels also produced a similar effect [13–16]. In a culture of rat cerebellar cells, diclofenac sodium increased the activity of potassium channels, increasing the release of potassium from the cell [17]. These results suggest that the peripheral antinociceptive effect of diclofenac sodium may be associated with activation of several types of potassium channels involving NO and guanosine cyclomonophosphate (cyclo-GMP).
Thus, the analgesic effect of diclofenac may be due to its effect on various levels and links in the pathogenesis of pain. In addition to the analgesic effect associated with a decrease in inflammation in the damaged area due to inhibition of prostaglandins (COX-1 and COX-2), diclofenac can reduce pain by reducing inflammation and through other mechanisms (restraining the migration of leukocytes to the site of inflammation, influencing the balance of cytokines) by affecting on potassium channels at the peripheral level, and also reduce the perception of pain through central mechanisms (by increasing the synthesis of the serotonin precursor (tryptophan) in brain tissue).
Indications for the use of diclofenac
Despite the wide range of currently existing NSAIDs and the creation in recent years of a new class of symptomatic anti-inflammatory drugs (selective COX-2 inhibitors), diclofenac sodium remains the most popular drug among NSAIDs.
The use of diclofenac in rheumatology
From the very beginning of its appearance, diclofenac has found wide use in rheumatology. An important feature that allowed diclofenac to displace other drugs from the NSAID group that were used before was its high analgesic and analgesic activity, along with good tolerability.
The effect of diclofenac is manifested by a decrease in the duration of morning stiffness, a decrease in pain (at rest and during movement), a decrease in swelling, swelling of the joints, as well as an improvement in the functional ability of the joints, which helps to increase the range of movements. Diclofenac is the drug of choice for most rheumatological diseases; it is used to treat inflammatory and degenerative rheumatic diseases (arthritis, arthrosis, etc.).
The use of diclofenac in general medical practice, orthopedics, traumatology, sports medicine
The most common disorders in general medical practice are disorders of the musculoskeletal system. Pathology of the musculoskeletal system is diverse in etiology and pathogenesis. Pain in this group of lesions can be caused by trauma, degenerative processes, inflammation, dysplasia, and trophic changes (osteoporosis). The mechanisms of development of the disease can be inflammatory, mechanical, neurogenic, etc. The pronounced analgesic effect of diclofenac in moderate and severe pain, inflammatory processes that occur after operations and injuries, rapid relief of spontaneous pain and pain during movement, reduction of inflammatory edema at the wound site made this drug one of the most necessary for the treatment of disorders of the musculoskeletal system, which are found in general medical practice, orthopedics, traumatology, sports medicine, and neurology.
When treating orthopedic and traumatic injuries, the form of release of the drug is also important. The possibility of combining local and general forms of diclofenac allows you to achieve maximum effectiveness while minimizing possible side effects. Local forms of diclofenac are most widely used for diseases of extra-articular tissues (tenosynovitis, bursitis, rheumatic soft tissue lesions), injuries of tendons, ligaments, muscles and joints. General forms, such as tablets, suppositories, solutions for injections,? - for massive injuries (combined and combined injuries, postoperative conditions, head injuries, fractures of large bones, etc.).
The use of diclofenac in neurology
Diclofenac has found widespread use for the relief of pain syndromes in neurological practice. Diclofenac is indicated for the treatment of acute back pain, tunnel syndromes (carpal tunnel syndrome, cubital tunnel syndrome, etc.), and migraines.
The duration of use and method of administration of the drug depend on the intensity of the pain syndrome. For moderate pain syndromes that do not limit the patient’s motor capabilities, it is possible to apply gels and ointments containing diclofenac sodium to the painful areas (spasmodic muscles) for 7–10 days. In case of intense pain that significantly limits the patient’s movement within the premises, injection routes of administration of diclofenac sodium are used for 3–7 days with a subsequent transition to oral forms [18]. There are reports of higher effectiveness of phonophoresis with diclofenac compared to the use of ointment forms of the drug [19].
The use of diclofenac in gynecology
The ability to eliminate pain and reduce the severity of blood loss during primary dysmenorrhea allowed the use of diclofenac in gynecological practice [20]. For primary dysmenorrhea, the daily dose is selected individually; it is usually 50–150 mg. The initial dose should be 50–100 mg; if necessary, over several menstrual cycles it can be increased to 150 mg/day. Diclofenac should be started when the first symptoms appear. Depending on the dynamics of clinical symptoms, treatment can be continued for several days. Diclofenac can also be used for pelvic inflammatory diseases, including adnexitis.
Method of administration and dosage: which dosage form to choose?
The undoubted advantage of diclofenac is the variety of dosage forms, including tablets (fast and retarded action), solution for parenteral administration, suppositories, as well as forms used for local therapy: ointments, creams, gels, spray, which creates convenience in selecting an individual dose and method use of the drug in different patients. The ability to combine different routes of administration in the same patient reduces the risk of adverse reactions.
Diclofenac tablets
Tablet forms of diclofenac are available in various dosages (
). The dose and route of administration of the drug for each patient are determined individually, taking into account the severity of the disease. The average recommended dose for adults is 100–150 mg/day. The maximum daily dose of diclofenac is 200 mg. In relatively mild cases of the disease, as well as for long-term therapy, a daily dose of 75–100 mg is sufficient. The daily dose should be divided into several single doses. If it is necessary to treat night pain or morning stiffness, in addition to taking the drug during the day, you can prescribe diclofenac in the form of suppositories before bedtime; however, the daily dose should not exceed 150 mg. Once the clinical effect is achieved, the dose is reduced to the minimum maintenance dose.
Children aged 6 to 15 years (inclusive) are prescribed only 25 mg tablets. The daily dose is 0.5–2 mg/kg body weight (in 2–3 doses, depending on the severity of the disease).
Adolescents aged 16 to 18 years can be prescribed 50 mg tablets. The tablets should be taken with plenty of liquid, preferably before meals. The tablets should not be split or chewed.
Diclofenac in the form of delayed-release tablets
A special form of the drug is diclofenac in the form of prolonged-release tablets. As a result of the delayed release of the active substance when taking retarded forms of diclofenac sodium, the effect occurs later, but lasts longer. These pharmacokinetic features make it possible to achieve a reduction in the number of drug doses taken by patients (1–2 times a day instead of 3–4 times a day) while maintaining a stable high concentration of the drug at the site of inflammation. This makes it preferable to use diclofenac in a retarded form when long-term use of the drug is necessary (for chronic pain syndromes, mainly in rheumatological practice).
The recommended starting dose for adults is 75 mg, that is, 1 retard tablet per day. The same dose is used in relatively mild cases of the disease, as well as for long-term therapy. In cases where the symptoms of the disease are most pronounced at night or in the morning, it is advisable to prescribe retard tablets at night.
The tablets should be swallowed whole, preferably with meals. If it is necessary to increase the dose, use an additional 1-2 tablets of diclofenac 25 mg. The maximum daily dose is 200 mg.
Currently, the Swiss pharmaceutical company Sandoz produces 75 mg bilayer tablets, which are unique in that each tablet consists of two layers and includes 12.5 mg diclofenac sodium immediate release and 62.5 mg diclofenac sodium sustained release, which provides both rapid onset of action and prolonged action of the drug.
Children and adolescents under 18 years of age should not be prescribed retard tablets.
Diclofenac in the form of rectal suppositories
The dosage form of diclofenac in the form of suppositories has a number of advantages. Suppositories do not cause the complications that are possible with parenteral administration of drugs (the development of muscle necrosis, infiltrates and suppuration at the injection site). It is advisable to prescribe suppositories if it is impossible to take drugs by mouth (in weakened patients, in the presence of esophageal strictures, etc.). When taken orally, there is a direct damaging effect of diclofenac on the cells of the gastric mucosa. With other methods of administering the drug (suppositories, ointments), the risk of damage to the gastrointestinal tract remains, but it is significantly lower. That is why, if there are signs of damage to the stomach and duodenum, preference is given to suppository forms of diclofenac.
Very often, suppositories are used in combination therapy: during the day the patient receives either injections or tablets, and at night - suppositories, which creates a better therapeutic effect due to a more uniform and long-term maintenance of the concentration of the drug in the blood. In this case, the total daily dose of diclofenac should not exceed 150 mg.
Children aged 6 to 15 years (inclusive) are prescribed only 25 mg suppositories. The daily dose is 0.5–2 mg/kg body weight (the daily dose, depending on the severity of the disease, should be divided into 2–3 single doses). For the treatment of RA, the daily dose can be increased to a maximum of 3 mg/kg (in several administrations). Adolescents aged 16 to 18 years can also be prescribed 50 mg suppositories.
The suppository is inserted into the rectum, as deep as possible, preferably after preliminary cleansing of the intestines. Suppositories should not be cut into pieces, since such a change in the storage conditions of the drug may subsequently lead to disruption of the distribution of diclofenac.
Diclofenac in the form of solution for injection
Diclofenac in injection form is preferably used when a faster analgesic effect is needed, usually with more severe acute pain (renal or hepatic colic, acute pain associated with soft tissue injuries (bruise, sprain), acute back pain, postoperative pain .Usually 1 ampoule per day is prescribed, but in severe cases, 2 injections per day can be prescribed at intervals of several hours, alternating the sides of administration.The use of injections can be combined with other dosage forms of diclofenac.The duration of parenteral use should not exceed two days; treatment if necessary continue with the same diclofenac, but in the form of tablets or rectal suppositories. When used intramuscularly, the drug is injected deep into the upper outer quadrant of the buttock; no more than 2 ampoules (150 mg) of the drug are used during the day. For renal and hepatic colic, the administration of diclofenac is usually combined with the use of antispasmodics.In case of a pronounced muscular component of back pain, the administration of diclofenac is combined with the use of muscle relaxants.
Combinations of two or more NSAIDs should be avoided as their effectiveness remains unchanged and the risk of side effects increases.
Diclofenac in the form of products for external (local) use
The undesirable effect of NSAIDs on the body is sharply limited if they are used in the form of local applications. The dosage form for such therapy is a mixture of the active drug with a base that ensures absorption under the skin. This method of treatment allows you to inject the drug directly into the lesion. At the same time, the impact on other organs and tissues is minimal.
Abroad, there are dosage forms in the form of plates for gluing to the skin containing 1.3% diclofenac epolamine. Diclofenac in the form of wafers first appeared in Switzerland in 1993; currently, diclofenac in the form of wafers is registered in 43 countries around the world. Diclofenac tablets are intended primarily for those who cannot take the oral form of diclofenac due to contraindications. They are used for soft tissue damage (bruise, sprain, compression, osteoarthritis) provided that the integrity of the skin is maintained 2 times a day. The plates are convenient for use, but are more expensive than other dosage forms.
These drugs are convenient to use and easy to dose. After applying the drug to the skin, the active compound accumulates in regional soft tissues and no more than 6% of the active substance enters the bloodstream. Moreover, the content of the drug in the muscles in the application zone is approximately three times higher than its level in distant muscle tissue. This makes the use of gel forms of diclofenac preferable for a wide range of disorders of the musculoskeletal system. Gel forms of diclofenac are over-the-counter medications and are very popular.
Diclak gel is the only diclofenac preparation on the Russian market with a 5% maximum concentration of the active substance, which allows you to reduce the dose of the drug taken orally, and in some cases even replace tablets. Approved for use by children over 6 years of age.
Diclofenac as part of combination drugs for the treatment of pain
There are also dosage forms (ointments, gels) in which diclofenac is one of the main components. The combination of several drugs with different mechanisms of action can increase the effectiveness of treatment.
Safety
Diclofenac has an optimal combination of analgesic and anti-inflammatory effects and is well tolerated. Therefore, in the absence of contraindications, it can be used even for a long time. Studies have confirmed that treatment with diclofenac in fairly high doses (150 mg) with long-term use (up to 8 months or more) was well tolerated by patients [2]. Of course, diclofenac, like any NSAID, may have side effects and contraindications. However, it should be noted that side effects, among which ulceration of the gastrointestinal mucosa (GIT) should be primarily feared, develop more often in individuals with risk factors.
Risk factors for gastrointestinal tract damage include:
- age over 65 years;
- history of peptic ulcer;
- eating food that increases gastric secretion (spicy, fatty, salty foods);
- large doses or simultaneous use of several NSAIDs;
- concomitant therapy with glucocorticoids;
- female gender, since increased sensitivity of women to this group of drugs has been detected;
- smoking;
- drinking alcohol;
- presence of Helicobacter pylori.
In this regard, treatment should begin with the lowest recommended dose, especially in risk groups. In individuals at risk, the daily dose of diclofenac should not exceed 100 mg; preference should be given to short-lived dosage forms of diclofenac and prescribed either 50 mg 2 times a day or 25 mg 4 times a day. Diclofenac should be taken after meals. When taking the drug for a long time, you should refrain from drinking alcohol, since diclofenac, like alcohol, is metabolized in the liver. If complaints from the gastrointestinal tract appear, it is necessary to perform esophagogastroduodenoscopy (EGD), and if you are systematically taking diclofenac, this procedure should be prescribed every 4-6 months, since NSAID gastropathy is often asymptomatic - “silent”.
If long-term use of diclofenac is necessary, which is especially important in rheumatology, it is advisable to prescribe diclofenac together with misoprostol, which protects the gastric mucosa from damage.
In patients with hypertension, it is necessary to monitor blood pressure levels; in patients with bronchial asthma, an exacerbation may occur while taking diclofenac. In patients with chronic liver and kidney diseases, small doses of the drug should be used, monitoring the level of liver enzymes.
Before prescribing diclofenac, the doctor must clarify whether the patient is taking any other medications due to concomitant diseases in order to avoid possible complications when using diclofenac in combination with other medications. It is known that diclofenac increases the plasma concentration of digoxin, lithium, cyclosporine A, including increasing its nephrotoxicity; increases the toxicity of methotrexate. Against the background of potassium-sparing diuretics, diclofenac increases the risk of hyperkalemia, and against the background of anticoagulants - the risk of bleeding. Diclofenac reduces the effect of diuretics, antihypertensives and hypnotics. Concomitant use of antidiabetic agents can lead to both hypo- and hyperkalemia.
More than 30 years have passed since the introduction of diclofenac into clinical practice. During this time, many new NSAIDs appeared. This has significantly expanded the ability to provide effective care to patients, since individual response to treatment is highly variable. However, diclofenac occupies a special place in this therapeutic arsenal. The combination of high efficiency, good tolerability and a variety of dosage forms of the drug make it possible to select the optimal therapy for a wide range of pain syndromes.
For questions regarding literature, please contact the editor.
A. B. Danilov , Doctor of Medical Sciences
FPPOV them. I. M. Sechenova, Moscow
Table 1. Indications for the use of diclofenac
Preparations for systemic use (tablets, injections, suppositories)
Rheumatology:
- rheumatism;
- RA, juvenile RA;
- extra-articular forms of rheumatism, rheumatism of soft tissues - periarthritis, bursitis, tendovaginitis, fibrositis, myositis;
- ankylosing spondylitis - ankylosing spondylitis;
- osteoarthritis;
- spondyloarthritis;
- other mono- and polyarthritis;
- degenerative joint diseases - arthrosis (coxarthrosis, spondyloarthrosis);
- back pain associated with degenerative changes in the spine;
- acute attack of gout
Neurology, traumatology, orthopedics, sports medicine, general medical practice:
- dorsalgia (lumbago, sciatica, myofascial and muscle-tonic pain);
- migraine and other types of headaches;
- tunnel syndromes, other diseases accompanied by inflammation of non-rheumatic origin (neuralgia, neuritis, lumbar ischialgia, bursitis, capsulitis, synovitis, tendinitis or tenosynovitis);
- traumatic bruises, sprains of ligaments, muscles and tendons; inflammatory swelling of soft tissues, muscle soreness (myalgia) and joints caused by heavy physical activity
Oncology:
- drug of the 1st step of the WHO ladder for the treatment of pain due to cancer
General medical practice:
- renal and biliary colic
Gynecology:
- gynecological diseases accompanied by pain and inflammation (primary dysmenorrhea, adnexitis, etc.)
Traumatology, surgery, dentistry:
- post-traumatic and postoperative pain syndromes;
- obstetrics, gynecology, dental or other surgical procedures
Otorhinolaryngology:
- for severe inflammatory diseases of the ear, nose and throat, which occur with severe pain, for example, pharyngitis, tonsillitis, otitis media. Treatment of the underlying disease is carried out in accordance with generally accepted principles, including the use of etiotropic therapy
Preparations for external and local use
Traumatology, sports medicine:
- post-traumatic inflammation of soft tissues and the musculoskeletal system (tendons, ligaments, muscles and joints);
- musculoskeletal injuries characteristic of sports medicine and sports: sprains, dislocations, bruises, contusions, overloads, etc.
Rheumatology:
- local treatment of inflammatory and degenerative joint diseases: RA, osteochondrosis of peripheral joints and spine, periarthropathy, etc.
Rheumatology, neurology:
- local treatment of inflammatory and degenerative diseases of soft tissues and periarticular tissues: tendovaginitis, shoulder-hand syndrome, bursitis, osteochondrosis, osteoarthrosis, periarthropathy, etc.;
- arthralgia;
- dorsalgia;
- myalgia
Traumatology, surgery:
- tenderness and inflammation of soft tissues
Ophthalmology:
- non-infectious conjunctivitis, post-traumatic inflammation after penetrating and non-penetrating wounds of the eyeball, pain syndrome when using an excimer laser, during surgery for removal and implantation of the lens (pre- and postoperative prevention of miosis, cystoid edema of the optic nerve)
Table 2.
Instructions for use
The absorption capacity of suppositories when used externally is low; the occurrence of negative effects when doses are exceeded is low.
Symptoms of overdose
In rare cases, the following may occur:
- head pain;
- nauseating sensations;
- gag reflexes;
- severe pain in the abdominal area;
- cloudy consciousness.
Treatment consists of relieving symptoms.
Features of use
The suppository contains 25, 50 or 100 mg of medication. The drug is administered after defecation, after washing your hands. Hemorrhoid suppositories are quickly removed from the packaging material and inserted deeply into the anus. Hands are thoroughly cleaned of the drug.
It is allowed to use up to 150 mg of the substance per day; in practice, a smaller amount of the drug is required to eliminate pain. Treatment terms are minimal - a few days.
Combination with other drugs and contraindications
When treating hemorrhoids, careful use of the drug in combination with antibiotics and medications intended for the treatment of epilepsy is recommended. Self-medication is unacceptable. Seek advice from a doctor in the field of proctology.
Contraindications to the use of Diclofenac for hemorrhoids:
- rectal fissures;
- erosive and ulcerative proctitis;
- allergies and intolerance to the medication;
- peptic ulcers of the gastrointestinal tract;
- the period of bearing a child and breastfeeding;
- insufficient function of the heart, liver, kidneys;
- age up to 12 years;
- bronchial asthma.
Side effects
The use of the drug in rare cases provokes side effects.
The functioning of the gastrointestinal tract is disrupted by abnormalities: consolidation of fecal matter, colic, nausea, gag reflexes, excessive gas formation, diarrhea, stomatitis, loss of appetite, bloating, and spotting.
Allergies are represented by: anaphylactic shock, tongue, lip swelling.
On the skin side, the following is recorded: baldness, itching, rashes, eczema, increased sensitivity to radiation.
The central nervous system experiences: tendency to sleep, reluctance to go to sleep, weakening of the body, depressive states, dizziness, anxiety, convulsions.
From the sensory organs: deterioration of auditory functions, the appearance of blind spots in visual characteristics, blurred vision, noise effect in the ears, changes in taste.
The genitourinary system is susceptible to kidney diseases and swelling as a result of poor fluid drainage from the body.
In the hematopoietic organs, the following occur: a decrease in platelets, a decrease in hemoglobin, an increase in eosinophils, and a tendency to bleeding.
From the respiratory system: swelling of the larynx, cough, bronchial spasms.
ENZYME
DICLOFENAC rectal suppositories 50 mg and 100 mg
Trade name: Diclofenac
International nonproprietary name (INN): diclofenac
Dosage form: rectal suppositories
Composition: one suppository contains -
active substance: sodium diclofenac - 0.05 g; 0.1 g
excipients: solid fat - 1.2 g; 1.85 g
DESCRIPTION:
Suppositories are white or white with a yellowish tint, torpedo-shaped. On a longitudinal section there is a homogeneous mass without foreign inclusions. An air rod or funnel-shaped recess may be present. Pharmacotherapeutic group:
Non-steroidal anti-inflammatory drug (NSAID).
ATX code : М01АВ05
PHARMACOLOGICAL PROPERTIES
Pharmacodynamics:
Diclofenac has anti-inflammatory, analgesic and antipyretic effects. By indiscriminately inhibiting cyclooxygenase 1 and 2, it disrupts the metabolism of arachidonic acid and reduces the amount of prostaglandins at the site of inflammation. In rheumatic diseases, the anti-inflammatory and analgesic effect of diclofenac helps to significantly reduce the severity of pain, morning stiffness, and swelling of the joints, which improves the functional state of the joint. For injuries, in the postoperative period, diclofenac reduces pain and inflammatory swelling.
Pharmacokinetics:
When administered rectally, the maximum plasma concentration of 1.2 mcg/ml is created after 40-60 minutes. and is linearly dependent on the dose used. No changes in the pharmacokinetics of diclofenac are observed during repeated administration and do not accumulate.
Communication with plasma proteins is more than 99% (most of it is associated with albumin). Penetrates into synovial fluid. The maximum concentration in synovial fluid is observed 2-4 hours later than in plasma. The half-life from synovial fluid is 3-6 hours (the concentration of the active substance in synovial fluid 4-6 hours after administration of the drug is higher than in plasma, and remains higher for another 12 hours). The relationship between the concentration of the drug in the synovial fluid and the clinical effectiveness of the drug has not been clarified.
50% of the active substance is metabolized during the “first pass” through the liver. Metabolism occurs as a result of multiple or single hydroxylation and conjugation with glucuronic acid. The enzyme system P450 CYP2C9 takes part in the metabolism of the drug. The pharmacological activity of the metabolites is lower than that of diclofenac.
Systemic clearance is 350 ml/min, volume of distribution is 550 ml/kg. Plasma half-life -2 hours. 65% of the administered dose is excreted in the form of metabolites
kidneys; 1% is excreted unchanged, the rest of the dose is excreted in the form of metabolites in bile.
In patients with severe renal failure (creatinine clearance less than 10 ml/min), the excretion of metabolites in bile increases, but no increase in their concentration in the blood is observed.
In patients with chronic hepatitis or compensated liver cirrhosis, the pharmacokinetic parameters of diclofenac do not change.
Diclofenac passes into breast milk.
INDICATIONS FOR USE:
The drug is intended for symptomatic therapy, reducing pain and inflammation at the time of use, and does not affect the progression of the disease.
Diseases of the musculoskeletal system:
- rheumatoid arthritis,
- psoriatic, juvenile chronic arthritis,
- ankylosing spondylitis,
- gouty arthritis,
- rheumatic soft tissue lesions,
- osteoarthritis of peripheral joints and spine, including radicular syndrome,
- tenosynovitis,
- bursitis.
Pain syndrome of mild or moderate severity:
- neuralgia,
- myalgia,
- sciatica,
- post-traumatic pain syndrome accompanied by inflammation,
- postoperative pain,
- headache,
- migraine,
- algodismenorrhea,
- adnexitis,
- toothache.
As part of complex therapy for infectious and inflammatory diseases of the ear, nose and throat with severe pain (pharyngitis, tonsillitis, otitis media).
Use strictly as prescribed by your doctor.
CONTRAINDICATIONS AND SIDE EFFECTS:
- hypersensitivity (including to other NSAIDs);
- complete or incomplete combination of bronchial asthma, recurrent polyposis of the nasal mucosa and paranasal sinuses and intolerance to acetylsalicylic acid or other non-steroidal anti-inflammatory drugs (including a history);
- erosive and ulcerative lesions of the gastric or duodenal mucosa, active gastrointestinal bleeding;
- inflammatory bowel diseases (ulcerative colitis, Crohn's disease) in the acute phase;
- period after coronary artery bypass grafting;
- decompensated heart failure;
- severe liver failure or active liver disease;
- severe renal failure (creatinine clearance less than 30 ml/min), progressive kidney disease;
- confirmed hyperkalemia;
- hemostasis disorders (including hemophilia);
- III trimester of pregnancy;
- lactation period;
- children's age (up to 18 years - for suppositories of 100 mg; up to 15 years - for suppositories of 50 mg);
- rectal bleeding, hemorrhoids, trauma or inflammation of the rectum.
Carefully:
- cerebrovascular diseases,
- anemia,
- bronchial asthma,
- cardiac ischemia,
- chronic heart failure,
- congestive heart failure,
- peripheral arterial diseases,
- arterial hypertension,
- edema syndrome,
- liver and kidney failure (creatinine clearance less than 30-60 ml/min),
- dyslipidemia/hyperlipidemia,
- inducible porphyria,
- smoking,
- alcoholism,
- inflammatory bowel diseases,
- anamnestic data on the development of peptic ulcer disease of the gastrointestinal tract, the presence of Helicobacter pylori infection,
- diabetes,
- condition after extensive surgical interventions,
- diverticulitis,
- systemic connective tissue diseases.
- severe somatic diseases,
- pregnancy I-II trimester,
- elderly age,
- long-term use of NSAIDs,
- simultaneous use of glucocorticosteroids (for example, prednisolone), anticoagulants (for example, warfarin), antiplatelet agents (for example, acetylsalicylic acid, clopidogrel), selective serotonin reuptake inhibitors (for example, citalopram, fluoxetine, paroxetine, sertraline).
.
Side effect:
Frequency of all side effects:
- often - 1-10%;
- sometimes - 0.1 -1.0%;
- rarely - 0.01-0.1%;
- very rarely - less than 0.001%, including isolated cases.
From the digestive system:
- often - epigastric pain, nausea, vomiting, diarrhea, dyspepsia, flatulence, anorexia, increased aminotransferase activity;
- rarely - gastritis, proctitis, bleeding from the gastrointestinal tract (vomiting with blood, melena, diarrhea mixed with blood), gastrointestinal ulcers (with or without bleeding or perforation), hepatitis, jaundice, impaired liver function;
- very rarely - stomatitis, glossitis, esophagitis, nonspecific hemorrhagic colitis, exacerbation of ulcerative colitis or Crohn's disease, constipation, pancreatitis, fulminant hepatitis, exacerbation of hemorrhoids.
From the nervous system:
- often - headache, dizziness;
- rarely - drowsiness;
- very rarely - sensory disturbances (including paresthesia), memory disorders, tremors, convulsions, anxiety, cerebrovascular disorders, aseptic meningitis, disorientation, depression, insomnia, nightmares, irritability, mental disorders.
From the senses:
- often - vertigo;
- very rarely - visual impairment (blurred vision, diplopia), hearing impairment, tinnitus, impaired taste.
From the urinary system:
- very rarely - acute renal failure, hematuria, proteinuria, interstitial nephritis, nephrotic syndrome, papillary necrosis.
From the hematopoietic organs:
- very rarely - thrombocytopenia, leukopenia, hemolytic and aplastic anemia, agranulocytosis.
Allergic reactions:
- rarely - anaphylactic/anaphylactoid reactions, including a marked decrease in blood pressure (BP) and shock;
- very rarely - angioedema (including the face).
From the cardiovascular system (CVS):
- very rarely - palpitations, chest pain, increased blood pressure, vasculitis, heart failure (HF), myocardial infarction.
From the respiratory system:
- rarely - bronchial asthma (including shortness of breath);
- very rarely - pneumonitis.
From the skin:
- often - skin rash;
- rarely - urticaria;
- very rarely - bullous rashes, erythema, incl. multiforme, and Stevens-Johnson syndrome, Lyell's syndrome, exfoliative dermatitis, itching, hair loss, photosensitivity, purpura, incl. allergic.
Other:
- rarely - swelling.
Special instructions:
During the period of treatment with the drug, monitoring of the peripheral blood picture, liver and kidney function, and examination of stool for the presence of blood should be carried out. If, while taking the drug, the increase in the activity of “liver” transaminases persists or increases, if clinical symptoms of hepatotoxicity are noted (including nausea, fatigue, drowsiness, diarrhea, itching, jaundice), treatment should be discontinued.
Because of the important role of prostaglandins in maintaining renal blood flow, special caution should be exercised when prescribing to patients with cardiac or renal insufficiency, as well as when treating the elderly, taking diuretics, AND patients who have a decrease in circulating blood volume for any reason (eg , after extensive surgery). If diclofenac is prescribed in such cases, monitoring of renal function is recommended as a precaution. In patients with liver failure (chronic hepatitis, compensated cirrhosis of the liver), the kinetics and metabolism do not differ from similar processes in patients with normal liver function. When carrying out long-term therapy, it is necessary to monitor liver function, peripheral blood patterns, and stool analysis for occult blood. Due to the negative effect on fertility, the drug is not recommended for women wishing to become pregnant. In patients with infertility (including those undergoing examination), it is recommended to discontinue the drug. To reduce the risk of developing adverse events from the gastrointestinal tract, the minimum effective dose should be used for the shortest possible course. Patients taking the drug must refrain from drinking alcohol.
Use during pregnancy and lactation:
The use of diclofenac is contraindicated in the third trimester of pregnancy (possible suppression of uterine contractility and premature closure of the ductus arteriosus in the fetus), and in the first and second trimester its use is possible only in cases where the expected benefit to the mother outweighs the potential risk to the fetus. The drug is prescribed in the minimum effective dose.
Diclofenac and its decomposition products pass into breast milk in small quantities. If it is necessary to use the drug in high doses and for a long time, you should consider stopping breastfeeding.
Impact on the ability to drive vehicles and machinery:
During the treatment period, the speed of mental and motor reactions may decrease, so it is necessary to refrain from driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
METHOD OF APPLICATION AND DOSAGE:
Rectally. Before using the suppository, it is recommended to empty the intestines.
Suppositories 100 mg: adults: 1 suppository 1 time per day.
Suppositories 50 mg: adults and children over 15 years of age. 1 suppository 2 times a day. The maximum daily dose is 150 mg.
When used simultaneously with oral forms of diclofenac, it is rational to use a single dose of 100 mg at night (in this case, evening administration of oral forms of diclofenac is excluded).
The duration of use of the drug is no more than 7 days.
Use during pregnancy and lactation:
The use of diclofenac is contraindicated in the third trimester of pregnancy (possible suppression of uterine contractility and premature closure of the ductus arteriosus in the fetus), and in the first and second trimester its use is possible only in cases where the expected benefit to the mother outweighs the potential risk to the fetus. The drug is prescribed in the minimum effective dose.
Diclofenac and its decomposition products pass into breast milk in small quantities. If it is necessary to use the drug in high doses and for a long time, you should consider stopping breastfeeding.
Overdose:
Symptoms:
- vomit,
- bleeding from the gastrointestinal tract,
- epigastric pain,
- diarrhea,
- dizziness,
- noise in ears,
- lethargy,
- convulsions,
- rarely - increased blood pressure (BP), acute renal failure, hepatotoxicity, respiratory depression, coma.
Treatment:
symptomatic therapy aimed at eliminating increased blood pressure, renal dysfunction, seizures, gastrointestinal irritation, respiratory depression; in case of erroneous oral use of suppositories, gastric lavage and activated charcoal are recommended. Forced diuresis and hemodialysis are ineffective (due to the significant connection with proteins and intensive metabolism).
INTERACTIONS WITH OTHER MEDICINES:
Increases plasma concentrations of digoxin, methotrexate, lithium and cyclosporine.
Reduces the effect of diuretics; against the background of potassium-sparing diuretics, the risk of hyperkalemia increases; against the background of anticoagulants, thrombolytic agents (alteplase, streptokinase, urokinase) - the risk of bleeding (usually from the gastrointestinal tract). Reduces the effects of antihypertensive and hypnotic drugs.
Cefamandole, cefoperazone, cefotetan, valproic acid and plicamycin increase the incidence of hypoprothrombinemia.
Cyclosporine and gold preparations increase the effect of diclofenac on the synthesis of prostaglandins in the kidneys, which increases nephrotoxicity.
Simultaneous administration with ethanol, colchicine, corticotropin and St. John's wort preparations increases the risk of bleeding in the gastrointestinal tract.
Diclofenac enhances the effect of drugs that cause photosensitivity.
Drugs that block tubular secretion increase the plasma concentration of diclofenac, thereby increasing its toxicity.
Concomitant use with paracetamol increases the risk of developing nephrotoxic effects of diclofenac.
Increases the likelihood of side effects of other NSAIDs and glucocorticosteroids (gastrointestinal bleeding), methotrexate toxicity and cyclosporine nephrotoxicity.
Acetylsalicylic acid reduces the concentration of diclofenac in the blood. Reduces the effect of hypoglycemic drugs.
RELEASE FORM:
Rectal suppositories 50 mg, 100 mg.
5 suppositories per blister pack made of polyvinyl chloride film. 2 blister packs along with instructions for use in a cardboard pack.
CONDITIONS FOR DISCHARGE FROM PHARMACIES:
Dispensed by prescription.
BEST BEFORE DATE:
2 years. Do not use after expiration date.
STORAGE AND TRANSPORTATION:
In a dry place, protected from light, at a temperature not exceeding 25 ° C.
Keep out of the reach of children.
About consumer reviews
The network contains numerous reviews about the experience of treating hemorrhoids with Diclofenac suppositories. Basically, these are positive points that describe the practice of treating hemorrhoids and other inflammatory diseases, vividly and colorfully describing how the drug helped heal external or internal hemorrhoids at different stages of development, helped resolve bleeding nodes, and heal anal fissures. They also talk about effectiveness and the absence of side effects for a long time.
Don't trust reviews entirely. Consult a doctor. Read the instructions for use. Consider individual intolerance to the drug.
Diclofenac suppositories
Registration number: P N000061/01
Trade name of the drug: Diclofenac - MFF.
International nonproprietary name: Diclofenac.
Dosage form: Rectal suppositories.
Composition per suppository: Active ingredient:
- Diclofenac sodium – 50 mg
Auxiliary component:
- Solid fat (base for suppositories) - until a suppository weighing 1.50 g is obtained
Description: Suppositories are white or white with a slightly yellowish tint, odorless, torpedo-shaped; an air rod or a funnel-shaped depression is allowed on the cut.
Pharmacotherapeutic group: Non-steroidal anti-inflammatory drug.
ATX code: М01АВ05
Pharmacological properties: Non-steroidal anti-inflammatory drug, phenylacetic acid derivative; has anti-inflammatory, analgesic and antipyretic effects. By indiscriminately inhibiting cycloxygenase 1 and cycloxygenase 2, it disrupts the metabolism of arachidonic acid and reduces the amount of prostaglandins at the site of inflammation. Most effective for inflammatory pain. Like all non-steroidal anti-inflammatory drugs, the drug has antiplatelet activity.
Pharmacokinetics: The maximum concentration in the blood plasma is created after 30 - 40 minutes and is linearly dependent on the dose used. No changes in the pharmacokinetics of diclofenac are observed during repeated administration and do not accumulate. Communication with plasma proteins is more than 99% (most of it is associated with albumin). Penetrates into synovial fluid. The maximum concentration in synovial fluid is observed 2 - 4 hours later than in plasma. The half-life from synovial fluid is 3 - 6 hours (the concentration of the active substance in synovial fluid 4 - 6 hours after administration of the drug is higher than in plasma, and remains higher for another 12 hours). The relationship between the concentration of the drug in the synovial fluid and the clinical effectiveness of the drug has not been clarified. Metabolism occurs as a result of multiple or single hydroxylation and conjugation with glucuronic acid. The enzyme system P450 CYP2C9 takes part in the metabolism of the drug. The pharmacological activity of the metabolites is lower than that of diclofenac. Systemic clearance is 350 ml/min, volume of distribution is 550 ml/kg. The half-life from plasma is 2 hours. 65% of the administered dose is excreted in the form of metabolites by the kidneys; less than 1% is excreted unchanged, the rest of the dose is excreted as metabolites in the bile. In patients with severe renal failure (creatinine clearance less than 10 ml/min), the excretion of metabolites in bile increases, but no increase in their concentration in the blood is observed. In patients with chronic hepatitis or compensated liver cirrhosis, the pharmacokinetic parameters of diclofenac do not change. Diclofenac passes into breast milk.
Indications for use: Symptomatic treatment of diseases of the musculoskeletal system (rheumatoid arthritis, psoriatic, ankylosing spondylitis; gouty arthritis, rheumatic soft tissue lesions, osteoarthritis of peripheral joints and spine, including radicular syndrome, tenosynovitis, bursitis). Pain syndrome of mild or moderate severity: neuralgia, myalgia, lumboischialgia, post-traumatic pain syndrome accompanied by inflammation, postoperative pain, headache, migraine, algomenorrhea, adnexitis, proctitis, toothache. As part of complex therapy for infectious and inflammatory diseases of the ear, nose and throat with severe pain (pharyngitis, tonsillitis, otitis media).
Contraindications: The period after coronary artery bypass grafting; III trimester of pregnancy, breastfeeding period; Uncompensated heart failure; Hypersensitivity to the active substance or auxiliary components; Anamnestic data on an attack of bronchial obstruction, rhinitis, urticaria after taking acetylsalicylic acid or other NSAIDs (complete or incomplete acetylsalicylic acid intolerance syndrome - rhinosinusitis, urticaria, nasal polyps, asthma); Erosive and ulcerative changes in the mucous membrane of the stomach or duodenum, active gastrointestinal bleeding; Inflammatory bowel diseases (ulcerative colitis, Crohn's disease); Cerebrovascular bleeding or other bleeding and hemostasis disorders; Severe liver failure or active liver disease; Severe renal failure (creatinine clearance less than 30 ml/min), progressive kidney diseases, incl. confirmed hyperkalemia; Children's age (up to 18 years for 100 mg suppositories, up to 15 years for 50 mg suppositories); Rectal bleeding, hemorrhoids, trauma or inflammation of the rectum.
With caution: Anemia, bronchial asthma, cerebrovascular diseases, coronary heart disease, congestive heart failure, arterial hypertension, peripheral arterial disease, edema syndrome, liver or renal failure, dyslipidemia/hyperlipidemia, diabetes mellitus, smoking, inflammatory bowel disease, condition after extensive surgical interventions, inducible porphyria, old age, diverticulitis, systemic connective tissue diseases, creatinine clearance less than 60 ml/min, pregnancy (I-II trimester). Anamnestic data on the development of gastrointestinal ulcers, the presence of Helicobacter pylori infection, long-term use of NSAIDs, frequent alcohol consumption, severe somatic diseases. Concomitant therapy with anticoagulants (for example, warfarin), antiplatelet agents (for example, acetylsalicylic acid, clopidogrel), oral glucocorticosteroids (for example, prednisolone), selective serotonin reuptake inhibitors (for example, citalopram, fluoxetine, paroxetine, sertraline).
Method of administration and dosage: Rectally, for adults, the initial dose is 100 mg/day, divided into 2 doses; in mild cases and with long-term therapy - 50 mg/day; in addition to oral administration, the total daily dose (rectal and oral) should not exceed 150 mg. For algodismenorrhea (when the first symptoms appear), the initial dose is 50 - 100 mg / day, which, if necessary, is increased over several menstrual cycles to 150 mg. Migraine attack - 100 mg at the first sign of an attack. If necessary, repeat 100 mg. If it is necessary to continue treatment in subsequent days, the daily dose should not exceed 150 mg over several administrations. For adolescents over 15 years of age - no more than 1 suppository.
Side effects: Often - 1 - 10%; sometimes - 0.1 - 1%; rarely - 0.01 - 0.1%; very rarely - less than 0.001%, including isolated cases. From the digestive system: often - epigastric pain, nausea, vomiting, diarrhea, dyspepsia, flatulence, anorexia, increased aminotransferase activity; rarely - gastritis, proctitis, bleeding from the gastrointestinal tract (vomiting with blood, melena, diarrhea mixed with blood), gastrointestinal ulcers (with or without bleeding or perforation), hepatitis, jaundice, impaired liver function; very rarely - stomatitis, glossitis, damage to the esophagus, diaphragm-like intestinal strictures (nonspecific hemorrhagic colitis, exacerbation of ulcerative colitis or Crohn's disease), constipation, pancreatitis, fulminant hepatitis, exacerbation of hemorrhoids. From the nervous system: often – headache, dizziness; rarely - drowsiness; very rarely - sensory disturbance, incl. paresthesia, memory disorders, tremor, convulsions, anxiety, cerebrovascular disorders, aseptic meningitis, disorientation, depression, insomnia, nightmares, irritability, mental disorders. From the senses: often – vertigo; very rarely - visual impairment (blurred vision, diplopia), hearing impairment, tinnitus, impaired taste. From the urinary system: very rarely - acute renal failure, hematuria, proteinuria, interstitial nephritis, nephrotic syndrome, papillary necrosis. From the hematopoietic organs: very rarely - thrombocytopenia, leukopenia, hemolytic and aplastic anemia, agranulocytosis. Allergic reactions: anaphylactic/anaphylactoid reactions, including severe decrease in blood pressure and shock; very rarely - angioedema (including the face). From the cardiovascular system: very rarely - palpitations, chest pain, increased blood pressure, vasculitis, heart failure, myocardial infarction. From the respiratory system: rarely - bronchial asthma (including shortness of breath); very rarely - pneumonitis. From the skin: often – skin rash; rarely - urticaria; very rarely - bullous rashes, eczema, incl. multiforme and Stevens-Jones syndrome, Lyell's syndrome, exfoliative dermatitis, itching, hair loss, photosensitivity, purpura, incl. allergic. Local reactions when used rectally: irritation of the rectal mucosa, mucous discharge mixed with blood, pain during defecation, rectal bleeding.
Overdose: Symptoms: Dizziness, headache, hyperventilation, clouding of consciousness, in children - myoclonic convulsions, nausea, vomiting, abdominal pain, bleeding, impaired liver and kidney function. Treatment: Activated carbon, symptomatic therapy. Forced diuresis and hemodialysis are not very effective.
Interaction with other drugs: Increases plasma concentrations of digoxin, methotrexate, lithium and cyclosporine. Reduces the effect of diuretics; against the background of potassium-sparing diuretics, the risk of hyperkalemia increases; against the background of anticoagulants, thrombolytic agents (alteplase, streptokinase, urokinase) - the risk of bleeding (usually from the gastrointestinal tract). Reduces the effects of antihypertensive and hypnotic drugs. Increases the likelihood of side effects of other nonsteroidal anti-inflammatory drugs and glucocorticosteroids (bleeding in the gastrointestinal tract), the toxicity of methotrexate and the nephrotoxicity of cyclosporine. Acetylsalicylic acid reduces the concentration of diclofenac in the blood. Concomitant use with paracetamol increases the risk of developing nephrotoxic effects of diclofenac. Reduces the effect of hypoglycemic drugs. Cefamandole, cefoperazone, cefotetan, valproic acid and plicamycin increase the incidence of hypoprothrombinemia. Cyclosporine and gold preparations increase the effect of diclofenac on the synthesis of prostaglandins in the kidneys, which increases nephrotoxicity. Simultaneous administration with ethanol, colchicine, corticotropin, serotonin reuptake inhibitors and St. John's wort preparations increases the risk of bleeding in the gastrointestinal tract. Diclofenac enhances the effect of drugs that cause photosensitivity. Drugs that block tubular secretion increase the plasma concentration of diclofenac, thereby increasing its toxicity. Antibacterial drugs from the quinolone group - the risk of developing seizures. Effect on laboratory test results: diclofenac may affect serum transaminases (if this effect is prolonged or if complications occur, treatment should be discontinued) and may also cause an increase in potassium concentration.
Cautions: Due to the important role of prostaglandins in maintaining renal blood flow, special caution should be exercised when prescribing to patients with cardiac or renal failure, as well as when treating elderly patients taking diuretics, and patients who, for any reason, have a decrease in circulating volume. blood (for example, after major surgery). If diclofenac is prescribed in such cases, monitoring of renal function is recommended as a precaution. In patients with liver failure (chronic hepatitis, compensated cirrhosis of the liver), the kinetics and metabolism do not differ from similar processes in patients with normal liver function. When carrying out long-term therapy, it is necessary to monitor liver function, peripheral blood patterns, and stool analysis for occult blood. During the treatment period, the speed of mental and motor reactions may decrease, so it is necessary to refrain from driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Release form: Diclofenac-MFF rectal suppositories 50 mg; 5 suppositories per blister pack made of PVC film. Two blister packs together with instructions for medical use are placed in a cardboard pack.
Shelf life: 2 years. Do not use the drug after the expiration date.
Storage conditions: Store at a temperature not exceeding +20 °C. Keep out of the reach of children.
Conditions for dispensing from pharmacies: By doctor's prescription.